 maroke / iStock / Getty Images Plus
maroke / iStock / Getty Images Plus
Revolutionizing Denture Stability: Implant Solutions for Older Adults
A 94-year-old woman’s quality of life dramatically improved as she received dental implants to secure her mandibular denture.
With modern medical care, many individuals are living longer and healthier lives. Among older adults, tooth loss due to periodontal diseases, injury, and caries is common, and many of these patients wear partial or full dentures. These appliances can cause further bone and tooth loss. As a typical denture becomes loose, the underlying soft tissue develops inflamed areas and eating becomes difficult. Dental implants improve life quality for many older individuals by facilitating better nutritional intake and encouraging a more social and active lifestyle. Following is a case study of a dental implant placement in a 94-year-old woman.
In January 2022, a 94-year woman presented for an exam, X-rays, and replacement of her existing mandibular denture. Her main complaint was that the denture moved when she spoke or during mastication. The patient reported having trouble eating and that she frequently developed sore spots. In addition, the denture would sometimes fall out when she coughed or laughed.
An examination of her health history showed she has arthritis, asthma, high blood pressure, and thyroid disease. It was noted she is currently taking levothyroxine 125 mcg, lisinopril 30 mg, famotidine 20 mg, atorvastatin 20 mg, fluticasone propion-salmeterol inhaler, bid, clopidogrel 75 mg, and a daily aspirin. The patient indicated she had spoken to an individual who had received implants at the practice, and wanted to know if implants might be a viable approach to retain her mandibular denture.
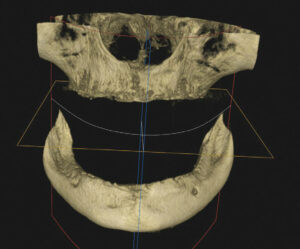
Physical examination of the patient revealed a very loose mandibular denture. Cone-beam computed tomography (CBCT) was used to determine the quality and quantity of bone present so a definitive treatment plan could be established (Figure 1). After review of the CBCT scan and residual mandibular bone volume, it was determined that 3.5×10 mm implants could be placed in the anterior mandibular ridge, which should provide stability and adequate function.
The patient was presented with three treatment plan options:
- New maxillary and mandibular dentures
- An implant-retained mandibular denture, along with relining of her existing maxillary denture
- An implant-supported fixed mandibular denture, along with relining of her existing maxillary denture.
In addition to these options, the patient was given a detailed explanation of each procedure, associated healing time, the expected result, and fees for each option. After questions and discussion, she chose the second option.
Due to her age and medical history, a decision was made to use a treatment plan that included a punch procedure instead of the more common full-flap technique. This minimally invasive surgical approach was possible due to the presence of sufficient keratinized gingival tissue and bone volume in the implant recipient sites.10 This would minimize any trauma associated with reflecting a full tissue flap to expose the mandibular osseous tissue and avoid excess bleeding that might arise due to her long-term aspirin regimen.
The patient said she understood the treatment plan and was ready to move forward as soon as possible. She was provided with prescriptions for amoxicillin 500 mg, ibuprofen 800 mg, and codeine/acetaminophen 30/300 mg to manage any possible post-placement pain. The patient was instructed to start the antibiotic and ibuprofen 24 hours prior to the punch procedure, and subsequently scheduled for implant placement.
In approximately 2 weeks, the patient returned to have the implants placed. After reviewing the scheduled treatment, she was given four cartridges of 2% lidocaine in the area of teeth #21 to 29. Using a tissue punch, the tissue at the height of the residual mandibular ridge was removed in the approximate areas where teeth #22, 25, 26 and 28 were previously located. A curet was used to remove any tissue tags.
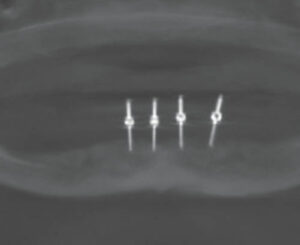
After an initial pilot hole was obtained, guide pins were inserted to verify the angulation of each site (Figure 2). Next, osteotomies were performed at all four sites. Figure 3 and Figure 4 represent the area of tooth #25 and the typical volume/shape of the mandible in each of the final implant locations. The clinical team placed 3.5×10 mm implants in each location with a 3 mm attachment cuff height (Figure 5). Figure 6 represents an oblique CBCT slice revealing the final implant locations within the mandibular osseous structure. Figure 7 represents the quality of the soft tissue immediately following implant placement, which shows excellent tissue adaption, color, and lack of any residual trauma.
Finally, the existing mandibular denture was hollowed out to accept the implant cuffs and metal housing that would be used to secure any retentive devices. Acrylic was placed in the denture and the housings were captured in a picked-up impression (Figure 8). A complete relining of the maxillary and mandibular dentures was done with the new attachment hardware in place. No sutures were necessary and there was no bleeding at any of the implant sites. She returned the following day and everything appeared to be within normal limits. She was then scheduled to return in 2 weeks for follow-up and instructed to call if she had any questions or if there were any issues with her soft tissue, the implants or dentures.
This information originally appeared in Hottel T, Chirla C. Dental implants in older adults. Decisions in Dentistry. 2023;9(2):28-31.








