 ALONA SINIEHINA/ISTOCK/GETTY IMAGES PLUS
ALONA SINIEHINA/ISTOCK/GETTY IMAGES PLUS
Treatment Planning Strategies For Dental Implant Procedures
In dental implant treatment, clinicians can minimize biologic and technical complications by addressing these key factors prior to implant placement.
This course was published in the September 2019 issue and expires September 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss dental implant success rates, and how risk assessment and establishing an individual treatment plan contribute to long-term outcomes.
- Define the ultimate determinant of a successful dental implant procedure, and key clinical strategies in implant treatment.
- List common complications in implant dentistry, and the parameters for diagnosis of peri-implant disease.
Dental implants have become the most frequently recommended choice to replace missing teeth in both partially and fully edentulous patients. Supporting the popularity of this procedure, longitudinal studies have shown that when dental implant treatment is performed correctly and on the right patient, long-term implant survival and success rates are high.1,2 To be precise, Moraschini et al3 reported a 94.6% survival rate (defined as implant remaining in place) for dental implants with a follow-up time of ≥ 10 years, and success rates ranging from 34.9% to 100%.
“Implant success” criteria were originally described by Albrektsson et al4 in 1986 (Table 1). Nevertheless, those criteria have been modified and updated several times as new surfaces and implant designs have emerged. Despite these updates and modifications, there is lack of homogeneity in the literature, and no definitive success criteria have been established.
According to the American College of Prosthodontists, more than 156 million Americans are missing at least one tooth. If clinicians consider that approximately 6% of these patients have one or more implants,5 the number of patients with implants in the U.S. is at least 9.3 million — and this number could be growing at a rate of 500,000 implants annually.6 Despite the increasing popularity of dental implants, this therapy is not free of complications and potential failure. Two types of complications occur in implant dentistry: biologic and technical (i.e., mechanical). Biologic complications are disturbances in the implant function characterized by biological processes affecting the supporting peri-implant tissues, namely, early and late implant failures, and adverse reactions in the peri-implant hard and soft tissues. Technical complications refer to mechanical damage of the implant, implant components and/or prosthesis.7
With the goal of minimizing biologic and technical complications or failures in dental implant treatment, this paper will focus on key factors that should be considered and addressed prior to any dental implant treatment.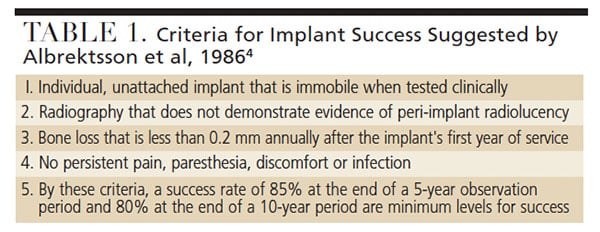
BIOLOGIC AND TECHNICAL COMPLICATIONS
Biologic Complications can include soft tissue dehiscence, peri-implant bone loss (≥ 2 mm) following initial healing, peri-implant mucositis, inflammation under the fixed prosthesis, and hypertrophy/hyperplasia of soft tissue.8 They are divided according to chronological criteria in early and late complications/failures.9 Early implant complications/failures occur soon after placement of implants, leading to a failure in achieving osseointegration, which might indicate an interference with the initial bone healing process. Factors thought to contribute to early implant failures include (but are not limited to) poor bone quantity and quality, the patient’s general health condition, smoking, early infection, post-insertion pain, lack of primary stability, or inadequate surgical and prosthetic techniques.9 On the other hand, late complications occur following a longer period after placement. These complications arise from pathologic processes after osseointegration is achieved. Most late complications fall within the categories of peri-implant mucositis (Figures 1A and 1B) and peri-implantitis (Figures 2A and 2B). As an example, the most frequently reported biologic implant-related complications are both considered late complications. These include peri-implant mucositis (inflammation of the peri-implant tissues with no bone loss), followed by excessive peri-implant crestal bone loss/peri-implantitis.10
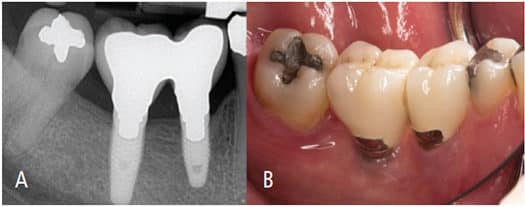
4-mm probing depths, with bleeding on probing and absence of radiographic bone
loss. This was diagnosed as peri-implant mucositis.
Peri-implant mucositis is an inflammatory lesion of the soft tissues surrounding an endosseous implant in the absence of loss of supporting bone or continuing marginal bone loss.11 Peri-implantitis is defined as a plaque-associated pathological condition occurring in tissues around dental implants, characterized by inflammation in the peri-implant mucosa and subsequent progressive loss of supporting bone.12 In a 2015 systematic review, Derks and Tomasi10 found a patient-based prevalence of peri-implant mucositis of 43% (range: 19% to 65%), and a 22% prevalence of peri-implantitis (range: 1% to 47%). Others have reported similar results.13–15
From a clinical standpoint, according to the 2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions,12 a diagnosis of peri-implantitis requires:
- Presence of bleeding and/or suppuration on gentle probing
- Increased probing depth compared to previous examinations
- Presence of bone loss beyond crestal bone level changes resulting from initial bone remodeling
In the absence of previous examination data, a diagnosis of peri-implantitis can be based on a combination of:12
- Presence of bleeding and/or suppuration on gentle probing
- Probing depths ≥ 6 mm
- Bone levels ≥ 3 mm apical of the most coronal portion of the intraosseous part of the implant
Therefore, inflammation around a dental implant will demand immediate attention to avoid any progression of peri-implant bone destruction.
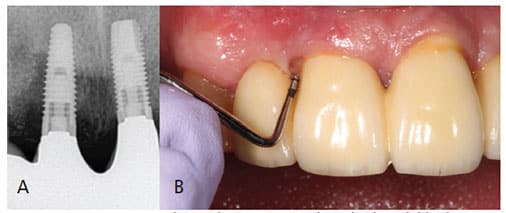
Technical Complications can include screw loosening, fracture (Figures 3A and 3B), veneering material chipping/fracture, wear and/or total replacement of acrylic resin teeth, framework fracture, loss of screw access filling material, fracture of the opposing restoration, implant fixture fracture, conversion of an implant-supported fixed complete dental prosthesis to an overdenture, or complete denture and patient dissatisfaction. The most common is reported to be abutment/occlusal screw loosening, with an estimated annual rate for this complication of 2.1%, and a 10-year estimate of 20.8%.16 The second most common is screw fracture, with an annual incidence rate of 1.9%, and a 10-year estimate of 18.5%.16

crown mobility. After removal of the crown and flap elevation, implant fracture
was observed. Possible causes include occlusal overload, marginal bone loss,
parafunctional habits, unfavorable buccal implant placement, manufacturer defect,
or combination of any of these. Explantation was performed.
RISK ASSESSMENT
The risk of failures and complications is not evenly distributed among individuals seeking dental implant treatment. Many patients will have one or more risk factors, making them more susceptible to complications than those with no significant risk factors. As defined by Genco17 in 1996, “a risk factor is an environmental, behavioral or biological factor that, if present, directly increases the probability of a disease occurring, and, if absent or removed, reduces that probability.” Most of the risk factors for complications and failures in dental implants also relate to periodontitis. Therefore, it is critical that clinicians are aware of these factors, know how to identify them, and, of utmost importance, know how to address and correct them.
Consequently, risk assessment for the implant patient should be a key part of the individual treatment plan. The main goals are to identify variables that increase the risk of complications leading to implant loss. It is a dynamic process in which risk will be assessed not only prior to dental implant treatment, but also during treatment, as well as after the implant is restored and functioning.
Absolute contraindications of implant placement are few, and mostly related to the patient’s unstable or uncontrolled medical history, such as recent myocardial infarction or cerebrovascular incident, valvular prosthesis surgery, immunosuppression, bleeding issues, active treatment of malignancy, drug abuse and/or psychiatric illness, as well as intravenous bisphosphonate use.18
Several risk factors/indicators have been found to be related to peri-implantitis, and these can be either local or general.19,20 Local risk factors can influence the bacterial composition and bacterial load at the implant. Examples include roughness at the implant surface, inaccessibility for oral hygiene, untreated periodontal pockets/active periodontitis, deep peri-implant pockets, the implant suprastructure connection, surface structure of the implant, excess cement, titanium particles, implant malposition, parafunctional habits/occlusal overload, and the absence of keratinized tissue adjacent to the implant. General risk factors relate to the patient and his or her susceptibility to infection. Examples include history of periodontal disease, genetic predisposition, smoking, general health status, systemic diseases that affect immunologic response (such as diabetes mellitus), inadequate oral hygiene, and the patient’s motivation to attend supportive care visits.
PRETREATMENT COMPREHENSIVE EXAMINATION
The ultimate goal of dental implant treatment is to achieve an esthetic, functional and long-lasting outcome that matches the patient’s expectations and needs. To do so, the first step is establishing an adequate and realistic individual treatment plan. This begins with a thorough review of the patient’s medical history, medications and medical treatment. Any general risk factors — such as uncontrolled systemic conditions — should be evaluated and corrected as indicated, since they may influence the patient’s healing potential and therefore the final outcome of treatment. In some cases, the patient will need to be referred to his or her primary care physician to address specific systemic conditions.
Patients should also be questioned about any substance abuse habits, such as tobacco, alcohol or drugs, as well as any parafunctional habits they may have. An initial assessment of patient motivation, compliance and oral hygiene should be performed. At this point, habit modifications, such as tobacco cessation, dietary changes or oral hygiene techniques, should be discussed and implemented, as needed.
CHIEF COMPLAINT
The patient’s chief complaint and goals of treatment should be addressed early on. Realistic endpoints should be targeted and described to patients. In the context of the individual treatment plan, the ultimate determinant of dental implant treatment success rates is the patient’s personal subjective criteria; therefore, realistic expectations should be determined and clarified at the beginning of treatment. Ultimately, it is clinician’s responsibility to ensure the patient’s expectations are realistic.
EXTRAORAL AND INTRAORAL EXAMINATION
The extraoral examination allows for head and neck assessment, including facial asymmetry, facial contours, skeletal profile, the temporomandibular joint and lymph nodes. Intraoral examination is performed to assess the condition of the oral hard and soft tissues, including lips, buccal and vestibular mucosa, hard and soft palate, oropharynx and fauces, tongue, floor of the mouth, gingiva and alveolar mucosa.
CLINICAL EXAMINATION
After a thorough extraoral and intraoral examination, the clinician can evaluate the potential implant sites. Several factors should be considered, including the available alveolar bone, current interdental and interocclusal space, and the quantity and quality of keratinized tissue. If a hopeless or nonrestorable tooth is still present, but the site will receive an implant in the future, this should also be considered at this time.
Alveolar Bone: It is important to ensure there is enough tridimensional bone to house the desired implant diameter and length. If a neurovascular structure is in close proximity (e.g., the inferior alveolar nerve), a minimum safety distance of at least 1.5 mm is suggested in presurgical planning.21
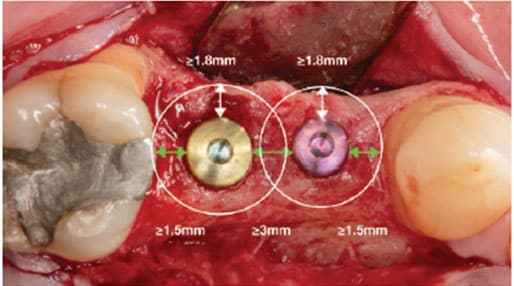
Interdental Space: The mesiodistal space must also be measured to determine whether there is enough space to place the implant and future restoration. The distance between an implant body and the adjacent tooth root should be ≥ 1.5 mm22,23 to minimize bone resorption and reduction or loss of the interproximal papilla.24 If several implants must be placed adjacent to each other, an interimplant distance of at least 3 mm should also be considered to minimize crestal bone loss and interimplant papilla loss (Figure 4).25
Interocclusal Space: With a cemented crown, a minimum distance of 7 mm is needed from the shoulder of the implant to the opposing dentition (abutment height ≥ 5 mm + ≥ 2 mm for the height of the crown).26 If needed, the abutment could be shortened to the head of the abutment screw, but, in that case, retention would be highly compromised.
Because a screw-retained crown is a one-piece component, this restoration will require a minimum of 4 to 5 mm from the implant shoulder to the opposing dentition.27 The screwhead should be at least 1 mm apical from the occlusal table in order to adequately seal the screw access.
If a hybrid type of restoration is planned, > 15 to 17 mm of interocclusal space will be needed.
Soft Tissue: Evaluation of the quantity, quality and location of soft tissues present in the future implant site is of critical importance to ensure both an ideal esthetic outcome, as well as prevent future biological implant complications related to plaque accumulation. Although controversial, recent evidence suggests plaque buildup and marginal inflammation may be more frequent at implant sites with < 2 mm of keratinized mucosa.28–30 Additionally, keratinized mucosa may have advantages regarding patient comfort and ease of plaque removal.12
In addition to the aforementioned considerations, the use of extraoral and intraoral photographs, along with mounted and articulated diagnostic casts, can aid in establishing a comprehensive dental implant treatment plan, and facilitating communication with the patient and other clinicians involved in the case.
RADIOGRAPHIC EXAMINATION
The implant surgeon has to consider certain anatomic landmarks or conditions that may influence or determine implant placement, such as the inferior alveolar nerve, mental nerve, nasopalatine nerve, floor of the sinus, lingual concavities on the mandible, or simply inadequate bone dimensions for adequate implant placement (Figures 5A through 5D).31 Not considering these structures or conditions can place the patient at risk of reversible or irreversible nerve injuries, as well as sinus or bleeding complications. Several radiographic options are available for dental implant treatment planning. These range from standard intraoral projections (periapical or bitewing radiographs), extraoral projections (panoramic or cephalometric radiographs), and three-dimensional (3D) cross-sectional imaging (cone beam computed tomography [CBCT]). Currently, CBCT is a useful tool with the potential to improve today’s standard of care in implant dentistry. Its use should be based on a case-by-case selection of patients whose treatment plans will be significantly impacted by additional 3D information.32
The use of CBCT imaging has also aided in the development and improvement of guided implant surgery. The files from the CBCT scan can be imported to software to simulate virtual implant placement and design a surgical guide33 that will ensure more precise placement.
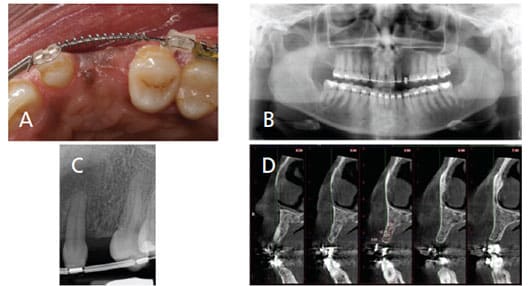
placement (C). Cone beam computed tomography shows 4.01 mm of bone buccolingually. There is inadequate bone for implant placement at this time, so it was decided to perform guided bone regeneration prior to implant placement (D).
DIAGNOSIS AND IMPLANT PLANNING
Once an adequate prosthetic plan has been established and the medical, clinical and radiographic examinations have been completed, the patient will be ready to receive dental implants. As noted, surgical guides help facilitate ideal implant placement. The four main objectives of using a surgical guide for the partially edentulous patient are:34
- Delineating the embrasure
- Locating the implant within the tooth contour
- Aligning the implants with the long axis of the eventual completed restoration
- Identifying the level of the cementoenamel junction or tooth emergence from soft tissue
As previously discussed, several parameters and distances must be observed in order to achieve optimal treatment outcomes. Hence, successful implant placement must be accomplished in the following 3D planes (Figure 4):
Mesiodistal Plane: As noted, the minimum distance between an implant and root of a tooth should be 1.5 mm22,23 and the interimplant distance between two adjacent implants should be ≥ 3 mm.25,35
Buccolingual Plane: To avoid losing bone height, the bone thickness on the buccal of the implant should be at least 1.8 to 2 mm.36 The same thickness may be expected for the lingual, as well. Knowing this, in anterior sites it is suggested the long axis of the implant should correspond to the incisal edge of the future restoration or to adjacent teeth, assuming that 1.5 to 2.0 mm of buccal bone can be maintained.37 If this is not possible, the implant can also be placed at the cingulum of the final restoration or 1.5 to 2.0 mm palatal to the incisal margin.22 Nevertheless, caution is needed in this case because the more palatal the implant placement, the greater the buccal cervical contour of the final crown. The type of final restoration planned (cemented versus screw-retained) will also determine the implant’s bucco-palatal placement.
Apicocoronal Plane: In the esthetic area, the implant shoulder should be placed 3 to 4 mm apical to the gingival margin of the final restoration to achieve the correct emergence profile.37
In instances where limited bone is available, pre-implant guided bone regeneration should be performed to increase the dimensions of the alveolar bone. When minor bone deficiencies are present, a bone graft can be performed at the time of implant placement.
Lastly, to ensure long-term results, the dental implant treatment plan should also include a maintenance phase once treatment is finalized.38 Maintenance intervals must be individualized to each patient and should consider existing risk factors. Mombelli39 described the three main components of maintenance:
- Measures taken by the patient
- Preventive measures taken by an oral health care professional
- Supportive therapy addressing the cause or sequelae of recurrent or residual disease
CONCLUSION
The ideal dental implant treatment plan will create a blueprint to achieve the best possible biological, functional and esthetic outcomes for each individual patient, while ensuring long-lasting results. Successful outcomes depend on the clinician performing all steps throughout planning and therapy with careful consideration of the final restorative/prosthetic goals.
Once the chief complaint of the patient is considered, a thorough medical and dental history, followed by a clinical examination, will allow practitioners to develop an individual treatment plan. In view of the examination results, risk factors and indicators should be identified, explained to the patient, and addressed, as necessary. The radiographic examination is crucial part of treatment planning. A CBCT scan may be recommended in cases where there is need for a 3D view of bony structures. By combining the radiographic examination with the prosthetic plan, surgical guides may be used to enhance the accuracy of implant placement while maintaining the constraints of 3D implant positioning guidelines.
Finally, once the implant is surgically inserted and restored appropriately, an adequate maintenance interval should be tailored for each patient to ensure long-term results and minimize future complications.
REFERENCES
- Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implan. 1990;5:347–359.
- Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10–16-year follow-up of non-submerged dental implants. Clin Oral Implants Res. 2010;21:772–777.
- Moraschini V, Poubel LA, Ferreira VF, Barboza Edos S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44:377–388.
- Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25.
- Elani HW, Starr JR, Da Silva JD, Gallucci GO. Trends in dental implant use in the U.S., 1999–2016, and projections to 2026. J Dent Res. 2018;97:1424–1430.
- What are Dental Implants? American Academy of Implant Dentistry. Available at: https://www.aaid-implant.org/dental-implants/what-are-dental-implants/. Accessed July 29, 2019.
- Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197–212;discussion 232–233.
- Papaspyridakos P, Chen CJ, Chuang SK, Weber HP, Gallucci GO. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int J Oral Maxillofac Implants. 2012;27:102–110.
- Sakka S, Baroudi K, Nassani MZ. Factors associated with early and late failure of dental implants. J Investig Clin Dent. 2012;3:258–261.
- Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015;42(Suppl 16):S158–S171.
- Heitz-Mayfield LJ, Salvi GE. Peri-implant mucositis. J Periodontol. 2018;89(Suppl 1):S257–S266.
- Berglundh T, Armitage G, Araujo MG, et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 45):S286–S291.
- Atieh MA, Alsabeeha NH, Faggion CM Jr., Duncan WJ. The frequency of peri-implant diseases: a systematic review and meta-analysis. J Periodontol. 2013;84:1586–1598.
- Dreyer H, Grischke J, Tiede C, et al. Epidemiology and risk factors of peri-implantitis: A systematic review. J Periodontal Res. 2018;53:657–681.
- Rokn A, Aslroosta H, Akbari S, Najafi H, Zayeri F, Hashemi K. Prevalence of peri-implantitis in patients not participating in well-designed supportive periodontal treatments: a cross-sectional study. Clin Oral Implants Res. 2017;28:314–319.
- Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012;91:242–248.
- Genco RJ. Current view of risk factors for periodontal diseases. J Periodontol. 1996;67(Suppl 10):1041–1049.
- Hwang D, Wang HL. Medical contraindications to implant therapy: Part I: absolute contraindications. Implant Dent. 2006;15:353–360.
- Renvert S, Quirynen M. Risk indicators for peri-implantitis. A narrative review. Clin Oral Implan Res. 2015;26(Suppl 11):15–44.
- Stacchi C, Berton F, Perinetti G, et al. Risk factors for peri-implantitis: effect of history of periodontal disease and smoking habits. A systematic review and meta-analysis. J Oral Maxillofac Res. 2016;7:e3.
- Sammartino G, Marenzi G, Citarella R, Ciccarelli R, Wang HL. Analysis ofthe occlusal stress transmitted to the inferior alveolar nerve by an osseointegrated threaded fixture. J Periodontol. 2008;79:1735–1744.
- Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;(Suppl 19):43–61.
- Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25:113–119.
- Esposito M, Ekestubbe A, Gröndahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Branemark implants. Clin Oral Implants Res. 1993;4:151–157.
- Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546–549.
- Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol. 2012;38:298–307.
- Chee W, JivraJ S. Screw versus cemented implant supported restorations. Br Dent J. 2006;201:501–507.
- Giannobile WV, Jung RE, Schwarz F, Groups of the 2nd Osteology Foundation Consensus Meeting. Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 1 — Effects of soft tissue augmentation procedures on the maintenance of peri-implant soft tissue health. Clin Oral Implants Res. 2018;29(Suppl 15):7–10.
- Lin GH, Chan HL, Wang HL. The significance of keratinized mucosa on implant health: a systematic review. J Periodontol. 2013;84:1755–1767.
- Roccuzzo M, Grasso G, Dalmasso P. Keratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study. Clin Oral Implants Res. 2016;27:491–496.
- Boyce RA, Klemons G. Treatment planning for restorative implantology. Dent Clin North Am. 2015;59:291–304.
- Rios HF, Borgnakke WS, Benavides E. The use of cone-beam computed tomography in management of patients requiring dental implants: an American Academy of Periodontology best evidence review. J Periodontol. 2017;88:946–959.
- D’Haese J, Ackhurst J, Wismeijer D, De Bruyn H, Tahmaseb A. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73:121–133.
- Section V Surgical Treatment Planning Considerations. J Oral Maxillofac Surg. 2017;75:23–27.
- Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75:1242–1246.
- Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5:119–128.
- Testori T, Weinstein T, Scutellà F, Wang HL, Zucchelli G. Implant placement in the esthetic area: criteria for positioning single and multiple implants. Periodontol 2000. 2018;77:176–196.
- Monje A, Aranda L, Diaz KT, et al. Impact of maintenance therapy for the prevention of peri-implant diseases: a systematic review and meta-analysis. J Dent Res. 2016;95:372–379.
- Mombelli A. Maintenance therapy for teeth and implants. Periodontol 2000. 2019;79:190–193.
From Decisions in Dentistry. September 2019;5(8):18,21—24 .




