
Minimally Invasive Treatment of Gingival Clefts
This case series explores the efficacy of a modified coronally advanced tunnel technique with acellular dermal matrix for treating gingival clefts
This course was published in the November/December 2023 issue and expires December 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 490
Educational Objectives
After reading this course, the participant should be able to:
- Identify the etiology and characteristics of gingival clefts, differentiating between red and white clefts.
- Discuss treatment modalities for red and white gingival clefts.
- Evaluate the effectiveness of the modified coronally advanced tunnel technique with acellular dermal matrix in achieving complete root coverage, increased keratinized tissue, and long-term stability in cases of gingival clefts.
A recent systematic review reported that although the majority of the observational studies confirmed a relationship between toothbrushing and gingival recession, the data to support or question the association are inconclusive.3 To date, the etiology and pathogenesis of this gingival defect remains unclear even though the assumptions are related to chronic factors that ulcerate the epithelium and healing occurs through the anastomosis of the external and internal epithelium in the gingival sulcus, creating a triangular defect.4
Depending on whether the entire connective tissue has been destroyed, gingival clefts can be divided into red when the gingival clefts are superficial and the entire connective tissue has not been destroyed, or white when the connective tissue is completely destroyed, and the underlying root surface is visible. Furthermore, other distinctive characteristics of the white cleft compared to the red cleft is its complete epithelialization of the edges/margins of the cleft.
The treatment of these clefts is different according to their type. If a patient is diagnosed with a red cleft, cessation of the mechanical self-care (toothbrushing and flossing) is recommended. After the first 2 weeks, oral hygiene should be restarted, modifying the toothbrushing approach to the roll technique.
The treatment of white clefts is more complex and involves a surgical procedure. The surgical protocol consists of excising the cleft in order to create a more manageable contour of the gingival recession for subsequent treatment and a subepithelial connective tissue graft to cover the exposed root surface.5 In 2013, Pilloni6 reported that a laterally moved, coronally advanced technique could eliminate this kind of anatomical lesion. He demonstrated that such a surgical approach was effective in treating an isolated Stillman cleft and the result remained stable over a 5-year period.6
Acellular dermal matrix (ADM) has been used for more than two decades as a connective graft substitute for the treatment of gingival recession.7,8 Among all, the modified coronally advanced tunnel (MCAT) technique presents the ideal features of a minimal invasive procedure, favorable flap relaxation, and the opportunity to stabilize the graft close to the gingival margin.9 In addition, it eliminates the need for a second surgical (donor) site, which can cause postoperative discomfort in some patients.
To our knowledge, no authors reported the use of ADM for the treatment of gingival recession defects with gingival clefts. Therefore, this case series presents short- and long-term outcomes of multiple adjacent gingival recession defects associated with gingival clefts treated with MCAT and ADM using a tunneling technique.
Case 1

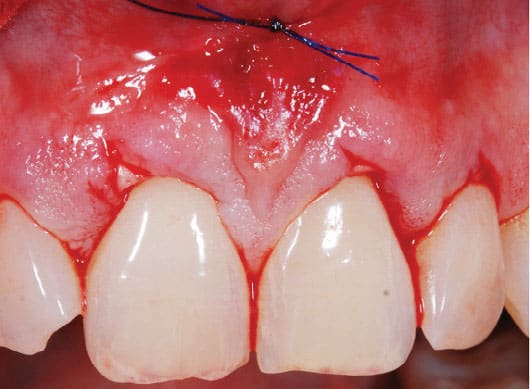
In 2012, a systemically healthy, 51-year-old nonsmoking man was referred for periodontal evaluation because of his chief complaint of poor esthetics and root hypersensitivity involving teeth #8 and 9. Clinical examination revealed the presence of multiple adjacent gingival recession defects of the involved sites associated with Stillman clefts (Figure 1).
The diagnosis was formulated as Miller Class I type I recession defects (RT1) with > 2 mm of keratinized tissue apical to the recessions.10 Risks and benefits of perio-plastic surgical intervention were discussed with the patient who expressed the desire to proceed with recession coverage treatment.
Prior to the surgical procedure, the patient underwent oral hygiene instructions, supragingival scaling, and prophylaxis. Oral hygiene instructions on proper flossing techniques were emphasized as part of the treatment protocol. The following parameters were assessed at the beginning of the treatment, prior to the periodontal surgery: recession depth measured from the cementoenamel junction (CEJ) to the most apical aspect of the cleft recession width, probing depth, clinical attachment level, tissue thickness via sulcular probing, and keratinized tissue width. All measurements were performed by the same operator using a standard periodontal probe.
After local anesthesia, hand instruments were used to ensure a smooth root surface. Use of surgical loupes enhanced the visibility to ensure that any composite or carious lesion was removed. After thorough debridement and smoothing of all root surfaces, the exposed root surface was treated with 17% ethylene-diaminetetraacetic acid for 1 minute using a cotton tip applicator to remove the smear layer and to expose the dentinal collagen fibers/tubules.
Flap elevation was performed in a minimally invasive fashion,11 using the technique reported by Allen.9 The site preparation was initiated with an intrasulcular incision made with an end-cutting intrasulcular knife followed by a supra-periosteal blunt dissection to the mucogingival junction using a periosteal elevator. A partial thickness dissection was then made using a modified periodontal gingivectomy knife extending apically, approximately 10 mm from the gingival margin, to allow for a passive advancement of the pouch. The palatal tissue was then elevated approximately 3 mm and the papillae were dissected from the alveolar crest. This palatal elevation of the flap, a modification from the original supra-periosteal protocol was completed to facilitate the flap advancement. The pouch was extended laterally to include the papillae of the adjacent teeth and a frenectomy was also completed at the same time.

The allograft was rehydrated following the manufacture’s instructions for a minimum of 10 minutes. It was then trimmed lengthwise to the site’s adjacent line angles, and vertically, to a dimension of 8 mm (Figure 2). The graft was placed in the pouch and aligned with the gingival margin and the connective tissue side of the ADM was placed against the tooth surface, as recommended by the manufacturer.

The tension-free pouch was coronally positioned to cover the ADM and 2 mm of tooth enamel (Figure 3). Double sling 5.0 polypropylene sutures were used around each tooth to secure the graft and to coronally position the graft and the pouch simultaneously (Figure 4). Analgesics were prescribed to control postoperative discomfort (Ibuprofen 800mg q6h for one week, Tylenol #3 q6h as needed). Azithromycin (500 mg) was prescribed; two tablets were taken the day of surgery, followed by one tablet per day for 3 days to prevent postoperative infection. To control any swelling, steroids were also prescribed (dexamethasone 8 mg 2 hours before surgery, 6 mg on the second day, 4 mg on the third day and 2 mg on the fourth day).


The patient was advised to avoid brushing or flossing of the surgical site for 3 weeks. Twice daily use of chlorhexidine gluconate (0.12%) mouthrinse was prescribed for 3 weeks after the surgery to control plaque buildup. The patient was seen postoperatively at 3 weeks and sutures were removed (Figure 5). Oral hygiene instructions were reinforced and prophylaxis was performed at each of the follow-up visits if indicated (ie, visible plaque present). Additional follow-up visits were scheduled at 3 and 6 months to monitor the surgical healing. Figure 6 represents the tissue at 10 years postsurgery.
Case 2
In 2012, a systemically healthy, 43-year-old nonsmoking woman was referred for periodontal evaluation with the chief complaint of poor esthetics and root hypersensitivity from teeth #10 and 11. Clinical examination revealed the presence of multiple adjacent gingival recession defects of the involved sites associated with a Stillman cleft on tooth #11 (Figure 7).


The diagnosis was formulated as Miller Class I10 RT1, with > 2 mm of keratinized tissue apical to the recessions. Risks and benefits of perio-plastic surgical intervention were discussed with the patient who decided to proceed with recession coverage treatment. A surgical procedure (Figures 8 and 9) and follow-up similar to Case 1 were performed. Figure 10 represents the 4 year follow-up and Figure 11, the 10 year follow-up.


Case 3

In 2012, a systemically healthy, 41-year-old nonsmoking woman with allergies to codeine and nitrous oxide was referred for periodontal evaluation because of poor esthetics and root hypersensitivity on teeth #10, 11, and 13. Clinical examination revealed the presence of multiple adjacent gingival recession defects of the involved sites associated with a Stillman cleft on tooth #11 (Figure 12). The diagnosis was Miller Class I10 RT1, with < 2 mm of keratinized tissue apical to the recessions. Risks and benefits of periodontic-plastic surgical intervention were discussed with the patient who expressed the desire to proceed with recession coverage treatment. A surgical procedure (Figure 13) and follow-up care similar to cases 1 and 2 were provided. Figure 14 represents the tissue at 4 years and Figure 15 at 10 years.




Clinical Outcomes
The patients in both cases complied with the recommended instructions, the healing was uneventful, and the self-reported discomfort was minimal. Clinical outcomes were evaluated at 3 months after therapy, and at every hygiene recare appointment. Position of the gingival margin was recorded by the same operator using a standard periodontal probe. Esthetic evaluation was performed according to the root coverage esthetic score by Cairo et al.12
- Gingival margin position:
- 0 points = failure to obtain root coverage (gingival margin apical or equal to the baseline recession)
- 3 points = partial root coverage
- 6 points = complete root coverage
- Marginal tissue contour:
-
0 points = irregular gingival margin (does not follow the CEJ)
-
1 point = proper marginal contour/ scalloped gingival margin (follows the CEJ)
-
- Soft-tissue texture:
-
0 points = scar formation and/or keloid-like appearance
-
1 point = absence of scar or keloid formation
-
- Mucogingival junction alignment:
-
0 points = mucogingival junction not aligned with the mucogingival junction of adjacent teeth
-
1point = mucogingival junction aligned with the mucogingival junction of adjacent teeth
-
- Gingival color
-
0 points = color of tissue varies from the gingival color at adjacent teeth
-
1 point = normal color and integration with the adjacent soft tissues
-
At all the time intervals — 3 months, 4 years and 10 years — both treated cases achieved complete root coverage, thickening of the gingival phenotype and excellent root coverage esthetic score. Stability of gingival margin and pleasant esthetics were documented in 2016, 4 years after treatment, and in 2022, 10 years after treatment. Throughout the follow-up period, no negative outcomes, such as the development of keloid tissue, increased probing depths, or dental hypersensitivity, were noted. The tissue contour, texture, color, and mucogingival junction post-surgically were identical to those of the adjacent teeth and the recession depths remained at 0 throughout the 10 year period The patients were happy with the pleasant esthetic result.
Discussion
These case reports present a minimally invasive treatment modality of the recession defects associated with the presence of the Stillman clefts that resulted in complete root coverage and perfect root coverage esthetic score in the short and long term. Previous treatment modalities for recession defects described in the literature5 involved the gingivectomy of the interrupted tissue as far as the apical limit of the cleft followed by a coronally advanced flap or an envelope flap in the case of multiple adjacent recession defects of the apical keratinized tissue.
If the cleft extends all the way to the alveolar mucosa, there will be insufficient keratinized tissue after the gingivectomy for a coronally advanced flap alone. A root coverage procedure will be required in addition to the subepithelial connective tissue graft and the coronally advanced flap.
The procedure described in theses case reports does not involve the removal of the margins of the cleft. We believe that the intrasulcular knife used in a submarginal incision is sufficient to cut/remove the epithelium from the margins of the cleft, exposing the underlying intact connective tissue. Furthermore, by not removing any tissue as was outlined in the procedures described in the literature,5 the keratinized tissue present apical and lateral to the cleft is preserved during the MCAT technique, increasing the chances of complete root coverage. By coronally advancing the tunnel, the cut margins of the cleft will be approximated and maintained in that position until a union of the exposed gingival connective tissue can occur.
The favorable outcomes observed at 3 months, 4 years and 10 years after therapy validate the efficacy of the MCAT with ADM for treatment of single and multiple adjacent recession defects complicated by the presence of the gingival clefts. Periodontal literature is in strong support of minimally-invasive procedures and armamentarium for reduced vascular damage and, ultimately, improved root coverage.11 Literature extensively published on efficacy of ADM in the absence of cervical lesions or previous restorations13-15 suggests that the addition of the ADM improves the short-term outcome of the flap-alone counterparts.16
The increase in the tissue thickness is one of the advantages attributed to ADM compared to flap alone.16-18 ADM serves as a scaffold that promotes cellular migration and revascularization from the host tissue.19 The increase in gingival thickness, ranging from 0.51 mm17 to ≥ 1.2 mm,8 makes the gingival margin more stable and less prone to relapse in the long‐term, as noted in the present case reports as well as in the periodontal literature.20
Conclusion
In the case examples discussed, the healing of the surgical sites progressed without any complications. The 4- and 10-year follow up of these cases showed that complete root coverage achieved was maintained for the duration of the follow-up period and a definite increase in the amount of the keratinized tissue was also evident.
Gonzalez et al21 confirmed the higher increase in keratinized tissue with a milder patient surgical experience when tunneling compared to a connective tissue graft. The MCAT technique, proposed by Aroca et al22 with ADM and approximation of the lateral edges of recessions provides good esthetic and functional results for treating Stillman clefts that evolved into true gingival recession.
References
- Cassini MA, Cerroni L, Ferlosio A, Orlandi A, Pilloni A. The gingival Stillman’s clefts: histopathology and cellular characteristics. Ann Stomatol (Roma). 2015;6:100-103.
- Greggianin BF, Oliveira SC, Haas AN, Oppermann RV. The incidence of gingival fissures associated with toothbrushing: crossover 28-day randomized trial. J Clin Periodontol. 2013;40:319-326.
- Rajapakse PS, McCracken GI, Gwynnett E, Steen ND, Guentsch A, Heasman PA. Does tooth brushing influence the development and progression of non-inflammatory gingival recession? A systematic review. J Clin Periodontol. 2007;34:1046-1061.
- Novaes AB, Ruben MP, Kon S, Goldman HM, Novaes AB, Jr. The development of the periodontal cleft. A clinical and histopathologic study. J Periodontol. 1975;46:701-709.
- Hallmon WW, Waldrop TC, Houston GD, Hawkins BF. Flossing clefts. Clinical and histologic observations. J Periodontol. 1986;57:501-504.
- Pilloni A, Dominici F, Rossi R. Laterally moved, coronally advanced flap for the treatment of a single Stillman’s cleft. A 5-year follow-up. Eur J Esthet Dent. 2013;8:390-396.
- Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86:S8-51.
- Tavelli L, Barootchi S, Di Gianfilippo R, et al. Acellular dermal matrix and coronally advanced flap or tunnel technique in the treatment of multiple adjacent gingival recessions. A 12-year follow-up from a randomized clinical trial. J Clin Periodontol. 2019;46:937-948.
- Allen EP. Subpapillary continuous sling suturing method for soft tissue grafting with the tunneling technique. Int J Periodontics Restorative Dent. 2010;30:479-485.
- Miller PD, Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:8-13.
- Di Gianfilippo R, Wang IC, Steigmann L, Velasquez D, Wang HL, Chan HL. Efficacy of microsurgery and comparison to macrosurgery for gingival recession treatment: a systematic review with meta-analysis. Clin Oral Investig. 2021;25:4269-4280.
- Cairo F, Rotundo R, Miller PD, Pini Prato GP. Root coverage esthetic score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J Periodontol. 2009;80:705-710.
- Ayub LG, Ramos UD, Reino DM, et al. A Randomized comparative clinical study of two surgical procedures to improve root coverage with the acellular dermal matrix graft. J Clin Periodontol. 2012;39:871-878.
- Wang HL, Romanos GE, Geurs NC, Sullivan A, Suarez-Lopez Del Amo F, Eber RM. Comparison of two differently processed acellular dermal matrix products for root coverage procedures: a prospective, randomized multicenter study. J Periodontol. 2014;85:1693-1701.
- Ozenci I, Ipci SD, Cakar G, Yilmaz S. Tunnel technique versus coronally advanced flap with acellular dermal matrix graft in the treatment of multiple gingival recessions. J Clin Periodontol. 2015;42:1135-1142.
- Ahmedbeyli C, Ipci SD, Cakar G, Kuru BE, Yilmaz S. Clinical evaluation of coronally advanced flap with or without acellular dermal matrix graft on complete defect coverage for the treatment of multiple gingival recessions with thin tissue biotype. J Clin Periodontol. 2014;41:303-310.
- Modaressi M, Wang HL. Tunneling procedure for root coverage using acellular dermal matrix: a case series. Int J Periodontics Restorative Dent. 2009;29:395-403.
- Barootchi S, Tavelli L, Di Gianfilippo R, et al. Gingival phenotype modification as a result of root coverage procedure with two human dermal matrices: long-term assessment of a randomized clinical trial. Int J Periodontics Restorative Dent. 2021;41:719-726.
- Bohac M, Danisovic L, Koller J, Dragunova J, Varga I. What happens to an acellular dermal matrix after implantation in the human body? A histological and electron microscopic study. Eur J Histochem. 2018;62:2873.
- Barootchi S, Tavelli L, Di Gianfilippo R, et al. Soft tissue phenotype modification predicts gingival margin long-term (10-year) stability: Longitudinal analysis of six randomized clinical trials. J Clin Periodontol. 2022;49:672-683.
- Gonzalez-Febles J, Romandini M, Laciar-Oudshoorn F, et al. Tunnel vs. coronally advanced flap in combination with a connective tissue graft for the treatment of multiple gingival recession: a multi-center randomized clinical trial. Clin Oral Invest. 2023:27:3627–3638.
- Aroca S, Moinar B, Windisch P, Grea I, Salvi GE, Nikolidakis D. Treatment of multiple adjacent Miller cladd l and ll gingival recessions with a modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. J Clin Periodontol. 2013;40:713-720.
From Decisions in Dentistry.November/December 2023; 9(10):32-35




