 CARLOS PASCUAL / ISTOCK / GETTY IMAGES PLUS
CARLOS PASCUAL / ISTOCK / GETTY IMAGES PLUS
Clinical Considerations for Relining a Complete Denture
Choosing the most appropriate denture liner requires a knowledge of available materials, as well as their indications and limitations.
This course was published in the November 2022 issue and expires November 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 670
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain applications for denture liners.
- Discuss tissue changes, pathologies, and functional mechanics that affect denture fit and function.
- Describe clinical considerations that influence the choice of liner materials and approaches to denture management.
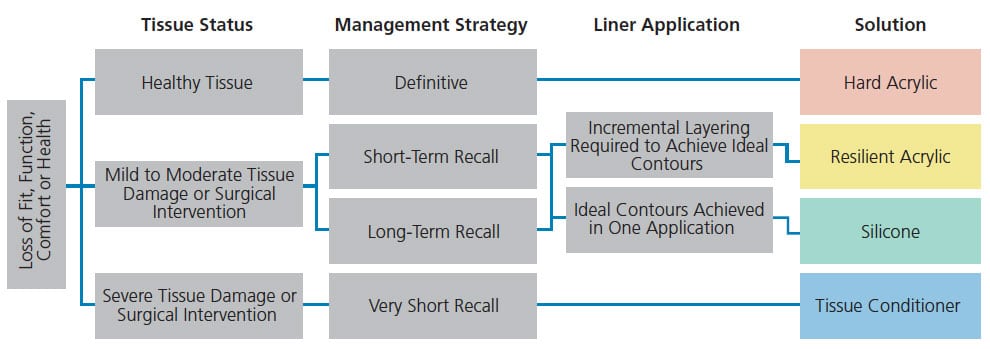
Resurfacing acrylic resin bases of complete dentures with a resilient or hard material is a necessary and common clinical and laboratory procedure in modern prosthodontics. Clinical applications of liners include managing abused oral tissues, enhancing comfort, improving fit and/or function of an existing prosthesis, retrofitting implant components, and extending the life of a prosthesis during a prolonged adjustment, transition or evaluation period.1–4 Appropriate clinical application is facilitated by a knowledge of available materials that includes their indications and limitations. The purpose of this article is to describe the different types of liner materials and present a decision tree (Figure 1) that aids liner selection.
Applying the correct reline material can only be accomplished with a thorough understanding of the procedure, as summarized here:
Step 1: With the patient’s chief complaint(s) in mind, examine the denture and underlying tissues. With a new prosthesis, poor functional mechanics are often caused by incomplete adaptation to the denture-bearing surface. Meticulous evaluation and adjustment may significantly improve retention, stability and support. Ulcerated and/or hyperplastic mucosa is indicative of chronically traumatized residual ridge tissues and may require surgical intervention as the first line of therapy.2 If the denture cannot be adjusted to fit properly and surgery is not warranted, a reline (resurfacing the intaglio), rebase (replacement of the entire denture base) or remake may be indicated.
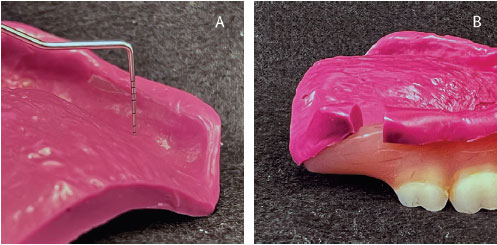
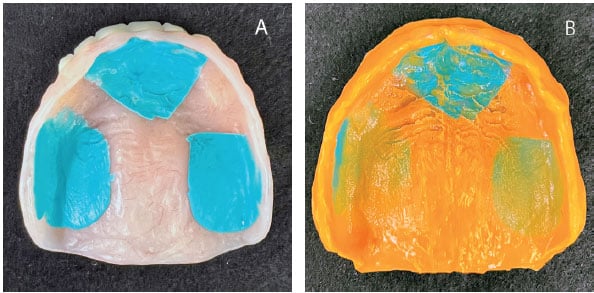
Step 2: Diagnose the problem(s). Denture-bearing tissue change is “progressive and inevitable”5 and, at times, intentional with surgical procedures, such as implants. Minor alterations in tissue contour may be perceived by the patient as a nuisance, diminishing denture fit and comfort. Moderate to extensive tissue change and associated deterioration of esthetics and function are often accompanied by trauma-induced pathologies. Once the etiology of the chief complaint has been resolved using a soft liner, a preview of the effectiveness of the definitive denture liner can be created with a “preview impression.” This simple diagnostic step involves making a closed mouth impression using an elastomeric material to capture intaglio surface detail and appropriate border contours and extensions in the unmodified denture. When the denture is removed and the resulting impression assessed, areas of thick impression material indicate dead space or incomplete vestibular fill (Figures 2A and 2B), while areas of thin material indicate intimate contact with the supporting tissues.6 The preview impression can be reinserted to determine if the patient’s chief complaint has been addressed.
Step 3: Develop a treatment plan. This may involve a hard reline or placement of a temporary resilient chairside liner, followed by remaking the denture. Either way, the plan must address all problems and result in a definitive solution.
Step 4: Reestablish occlusal vertical dimension (OVD) and centric occlusion. In an older denture, it is not uncommon for tissue resorption and prosthetic tooth wear to result in reduced OVD and forward rotation of the mandible (Figure 3).7 Reduced OVD is often accompanied by secondary pathologies, such as angular cheilitis, papillary hyperplasia of the denture-bearing soft tissues, and epulis fissuratum.2 If the occlusal plane of the maxillary denture is poorly positioned when the patient is in repose or smiling, heavy-body elastomeric impression material can be used to form tissue stops that reorient the denture. The mandibular denture may then be repositioned in a similar fashion to establish the appropriate OVD in maximal intercuspation position (MIP) in centric relation (CR).8 An interocclusal registration (i.e., bite registration) and recording of the OVD should be used to maintain this position during subsequent procedures.
Step 5: Create relief in the denture. Removing 2 mm of denture base acrylic from the intaglio surfaces ensures sufficient liner thickness, eliminates bacteria, and improves adhesion of the liner.3 All liners have a recommended minimal thickness (~2 mm) to facilitate optimal adhesion, durability, softness and/or strength.2,3
Step 6: Protect polished and occlusal surfaces. Precautions should be taken to protect the cameo surfaces (polished and occlusal surfaces) of the denture to avoid adherence of lining materials during clinical procedures. These critical surfaces can be protected using liner-specific surface protectants, silicone-based gels, petroleum-based lubricant, or simply applying medical-grade tape.
Step 7: Impress or apply the correct liner. Laboratory hard acrylic resin liners require an accurate impression of the denture-bearing tissues made while maintaining the appropriate vertical and horizontal occlusal relationships. The tissue stops are used to reorient the denture in the correct position and can be washed during the final impression to maintain this position (Figures 4A and 4B). Tissue conditioners and elastomeric impression materials are commonly employed for a functional or closed-mouth impression technique.8 If a chairside technique is indicated, primer or adhesive is applied to the relieved surfaces (after the tissue stops are removed) to facilitate liner adherence to the denture base. The liner can then be mixed and/or dispensed into the denture according to the manufacturer’s instructions. The denture containing the liner is placed in the mouth, and the patient is guided to close gently into MIP using the interocclusal registration until the predetermined OVD in CR is achieved. Once polymerized, excess material should be removed and the borders refined using scissors, a sharp blade, burs, wheels or points, as indicated by the manufacturer.
CHOOSING THE CORRECT LINER
Determining the most appropriate liner may be accomplished by asking four fundamental questions:
- What problem(s) exist with the denture(s)?
- What is the health of the underlying tissues?
- How long must the liner last?
- Can the desired contours be achieved with one application of material?
What problem(s) exist with the denture(s)?
Restoring the fit, function and comfort of a complete denture using a liner requires careful evaluation of the prosthesis itself. The nature of the problem may limit the usefulness of specific liners and/or require fabrication of a new definitive or treatment denture. These problems involve denture base thickness, evidence of previous repair, and excessively worn dentition. Use of a preview impression (mentioned in Step 2 above) will permit assessment of denture base thickness after completing the reline. Excessive base thickness (> 4 mm) in a maxillary denture prior to relining may best be managed using a rebase procedure to minimize palatal thickness. A denture base measuring < 2 mm, or displaying evidence of significant repair, may be subject to irreparable damage during denture base removal in preparation for the reline procedure.
Acrylic and composite resin denture teeth have the propensity for wear, especially when opposing natural dentition or ceramic restorations.9 Wear directly impacts OVD, occlusal relationships and esthetics. Relining is only indicated if existing occlusal surface morphology is serviceable (< 1 mm of wear) and the denture(s) can be repositioned to achieve OVD, occlusal relationships and esthetics.
What is the health of the underlying tissues?
Denture base movement results in damage to supporting oral tissues. Minor unavoidable movements during function have the potential to escalate with direct or indirect changes of edentulous ridge morphology.7 Resolution of pathology before fabrication of a definitive prosthesis is essential to optimize fit, comfort and function. Damaged denture-bearing soft tissues can benefit from a very soft liner, such as a tissue conditioner, replaced every two to four days to permit full tissue recovery.1 Tissues with mild to moderate damage or postsurgical wounds can be treated with resilient liners that are replaced at a longer recall interval (e.g., two to four weeks).1,2 Healthy tissues can be treated with laboratory or chairside hard acrylic liners or laboratory-processed resilient liners. Laboratory-processed resilient liners may be beneficial for patients with friable soft tissues and complicated health histories that include radiation therapy, bisphosphonates, poor salivary flow or irregular ridge contour.10
How long must the liner last?
The chemistry of a liner, specific oral conditions, and patient habits determine the liner’s useful durability. Hard acrylic resin liners are intended for definitive treatment during the serviceable life of the denture. However, resilient liners (silicone or acrylic resin) have a finite service life.11 Acrylic resin resilient liners contain plasticizers that interfere with the rigid set of methacrylate polymer chains.11,12 The volatile nature of plasticizers results in leaching over time, leading to dimensional distortion and hardening of the material.13 The typical useful life of an acrylic resin resilient liner is two to four weeks. Silicone liners are elastomeric materials that do not incorporate plasticizers;12 thus, silicone may be a better choice for long-term or definitive applications due to its stable softness and dimensional accuracy for up to two years. However, oxidation, sorption, delamination from the denture base resin, and tendency for bacterial and fungal accumulation lead to deterioration of silicone liners.3

Can the desired contours be achieved with one application of material?
One fundamental difference between silicone and acrylic resin liners is their ability to chemically adhere to the acrylic resin denture base materials. Silicone liners require a primed interface, such as ethyl acetate, to bond to acrylic resin. The inability to achieve a significant chemical bond between subsequent layers of silicone limits this material to a single application from which desired contours must be achieved.13 Acrylic resin liners chemically adhere to poly(methylmethacrylate) (PMMA) denture base material. Acrylic primers are composed of ethanol and benzyl butyl phthalate, which clean and soften PMMA polymer chains for increased chemical bonding.12 This chemistry allows for incremental layering of acrylic resin liners to better manage difficult contours or desired vertical dimension, making them especially useful for applications where significant tissue changes have occurred or are anticipated due to healing or surgery.
LINER MATERIALS
Laboratory-Processed Hard Acrylic Resin Liners — Laboratory-processed PMMA hard liners can be polymerized using compression- or injection-molding or processed in a positive-pressure vessel. When compared to resilient or chairside hard liners, laboratory-processed acrylic resin liners have superior physical properties related to dimensional accuracy, porosity, water absorption, solubility, elastic deformation, cleansability and durability.14 Laboratory-processed acrylic resin liners are the material of choice for a definitive solution for resurfacing a serviceable denture in an otherwise healthy oral environment.
Chairside Hard Resin Acrylic Liners — Chairside hard acrylic resin liners are chemically activated resins that can be applied directly to the denture base for intraoral polymerization. Typically, these materials combine pre-polymerized poly(ethylmethacrylate) (PEMA) or PMMA powder with liquid methacrylate. Alternatively, cartridge-dispensed, dual polymerized, resin composite-filled acrylics resins are available. Caution should be used with all chairside hard acrylic resins, as a significant exothermic reaction can result in thermal damage to oral tissues if not controlled by intermittent removal of the denture during polymerization.15 Patients may also complain of strong odor or burning sensation (especially with damaged tissues) related to monomer evaporation during polymerization. This material is contraindicated for use in patients with damaged tissues or edentulous ridge morphology with significant undercuts. Unlike laboratory-processed liners, chairside liners are not polymerized under pressure, which results in increased porosity, dimensional distortion, and eventual bacterial/fungal contamination. Although often considered a definitive procedure, a chairside hard reline yields inferior physical properties as compared to a laboratory hard reline and should only be used as an alternative when time or cost are concerns.16
Tissue Conditioners — Tissue conditioners consist of PEMA and a high concentration of plasticizers, which render a very soft material often described as a viscous gel.2 This property allows the material to continue to flow or deform over time, which is considered beneficial for healing severely damaged tissue or making functional impressions.2 However, rapid leaching of the plasticizer results in precipitous deterioration of the material that requires replacement in two to four days. Once acute symptoms of damaged tissues are mitigated, the tissue conditioner must be replaced with a resilient reline material for extended treatment periods or a definitive, laboratory-processed hard liner.
Resilient Acrylic Resin Liners — Resilient acrylic resin liners are composed of PMMA or PEMA and plasticizers such as dibutyl phthalate. This material can chemically bond to all methacrylate resins, allowing adherence to denture bases as well as to itself. Therefore, incremental application is possible for achieving ideal contours (in the same appointment or over a series of appointments) to adapt to tissue changes during prolonged therapy. Modifying the ratio of powder to liquid allows for controlled modification of material softness, as indicated by soft tissue status and patient comfort.
However, fluid sorption and material solubility of acrylic resin liners decrease longevity and color stability, while increasing potential for microbial biofilm formation.13 The prescribed duration of an acrylic resin liner (generally two to four weeks) is greatly influenced by obtaining at least 2 mm of liner thickness, adequate bonding to the denture base, and the patient’s ability to carefully clean and store the dentures without damaging the liner.3,17 Prolonging the recall period may result in hardening, distortion, and bacterial and/or fungal colonization of the liner, perpetuating tissue problems. Consequently, resilient acrylic resin liners are a transitional material that must be replaced by a definitive liner or denture remake upon resolution of symptoms.
Silicone Liners — The popularity of silicone liners may be attributed to their prolonged clinical durability. Devoid of methacrylate, silicone is the material of choice for patients allergic to acrylic resin. Dispensed by auto-mixed cartridge, this liner provides improved material properties when compared to resilient acrylic resin liners. Because silicone liners are not dependent on plasticizers, their serviceable life may span up to two years. Furthermore, health concerns related to phthalate esters, which resemble estrogen hormones, are eliminated. Although silicone liner resiliency cannot be adjusted through a monomer-to-polymer ratio, many brands offer multiple formulations for varying levels of softness.
The inability of silicone liners to bond directly with acrylic resin denture base material in the absence of a cement primer and deterioration of that bond over time are considered significant disadvantages. Procedures requiring incremental layering are not applicable with silicone liners. Additionally, silicone longevity is affected by water sorption and solubility, which lead to dimensional changes, increased hardness, and reduced bond strength at the liner-denture base interface.14,18 Therefore, surface sealers are often suggested to preserve denture cleanliness, silicone adherence, liner resiliency and color stability.14
CONCLUSION
Extending the serviceable lifespan of a complete denture can be facilitated by resurfacing the intaglio aspect of the denture with a diagnostic, transitional, therapeutic or definitive liner. While the overall clinical procedure may be similar, the indications for, and longevity of, various denture lining materials are determined, in part, by their chemistry and mechanical durability. Selecting the appropriate liner requires consideration of the prosthesis’ condition, tissue health, planned length of service, and the desired final contours.
REFERENCES
- Garcia LT, Jones JD. Soft liners. Dent Clin North Am. 2004;48:709–720.
- Dorocka-Bobkowska B, Medyński D, Pryliński M. Recent advances in tissue conditioners for prosthetic treatment: A review. Adv Clin Exp Med. 2017;26:723–728.
- Chladek G, Żmudzki J, Kasperski J. Long-term soft denture lining materials. Materials (Basel). 2014;7:5816–5842.
- MacGregor AR. Pressure-indicating pastes. J Dent. 1983;11:264–270.
- Zarb GA, Hobkirk J, Eckert S, Jacob R. Prosthodontic Treatment for Edentulous Patients: Complete Dentures and Implant-Supported Prostheses. 13th ed. Maryland Heights, Mo: Mosby; 2012:303.
- Phoenix RD, Cagna DR, DeFreest CF. Stewart’s Clinical Removable Partial Prosthodontics. 4th ed. New Delhi, India: CBS; 2008:447.
- Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120–132.
- Cagna DR, Massad JJ. Vinyl polysiloxane impression material in removable prosthodontics. Part 2: Immediate denture and reline impressions. Compend Contin Educ Dent. 2007;28:519–26; quiz 527–528.
- Ghazal M, Hedderich J, Kern M. Wear of feldspathic ceramic, nano-filled composite resin and acrylic resin artificial teeth when opposed to different antagonists. Eur J Oral Sci. 2008;116:585–592.
- Graham BS, Jones DW, Sutow EJ. Clinical implications of resilient denture lining material research. Part II: Gelation and flow properties of tissue conditioners. J Prosthet Dent. 1991;65:413–418.
- Hashem MI. Advances in soft denture liners: An update. J Contemp Dent Pract. 2015;16:314–318.
- Parr GR, Rueggeberg FA. In vitro hardness, water sorption, and resin solubility of laboratory-processed and autopolymerized long-term resilient denture liners over one year of water storage. J Prosthet Dent. 2002;88:139–144.
- Aloul RK, Shen C. The influence of plasticizer loss on the viscoelasticity of temporary soft liners. J Prosthodont. 2002;11:254–262.
- Mese A, Guzel KG. Effect of storage duration on the hardness and tensile bond strength of silicone- and acrylic resin-based resilient denture liners to a processed denture base acrylic resin. J Prosthet Dent. 2008;99:153–159.
- Dimiou AM, Michalakis K, Pissiotis A. Influence of thickness increase of intraoral autopolymerizing hard denture base liners on the temperature rise during the polymerization process. J Prosthet Dent. 2014;111:512–520.
- Mutluay MM, Ruyter IE. Evaluation of adhesion of chairside hard relining materials to denture base polymers. J Prosthet Dent. 2005;94:445–452.
- Murata H, Haberham RC, Hamada T, Taguchi N. Setting and stress relaxation behavior of resilient denture liners. J Prosthet Dent. 1998;80:714–722.
- Abe Y, Taji T, Hiasa K, Tsuga K, Akagawa Y. Dynamic viscoelastic properties of vinyl polysiloxane denture soft lining materials. J Oral Rehabil. 2009;36:887–893.
From Decisions in Dentistry. November 2022;8(11)30-33.




