 MILANEXPO / E+/ GETTY IMAGES PLUS
MILANEXPO / E+/ GETTY IMAGES PLUS
Utility of Cone Beam Imaging in Periodontics And Implant Therapy
This review will help providers understand applications for cone beam computed tomography in implant planning and placement, as well as when diagnosing and treating periodontal disease.
Cone beam computed tomography (CBCT) was introduced to the dental community more than 20 years ago.1 This technology gathers quality images of the dentition and surrounding structures that provide valuable, real-time information for dental implant planning. More recently, CBCT imaging has been found to aid in the diagnosis and treatment of various periodontal conditions — and these scans are captured more quickly and easily than conventional medical computed tomography.2 But this added radiation dose, and how it compares with conventional diagnostic imaging, should be considered. Table 1 shows comparative dosage levels from various radiation sources. It is important to remember that no matter how low the radiation dose, it is deemed excessive if it does not improve therapeutic outcomes.3,4 It is hoped this review will provide context for the possible application of cone beam imaging in dental implant planning and placement, as well as when diagnosing and treating periodontal disease.
Professional dental associations have authored opinion or position papers on the role of CBCT in dental implant surgical planning. The American Academy of Oral and Maxillofacial Radiology suggests the preoperative diagnostic phase of implant planning should use cross-sectional imaging, as it will provide diagnostic value at a tolerable radiation dose.5 In some countries, acquiring a CBCT for implant planning purposes is already the standard of care.6 In 2017, the American Academy of Periodontology investigated whether cone beam imaging should replace standard two-dimensional films for patients requiring dental implant surgery.7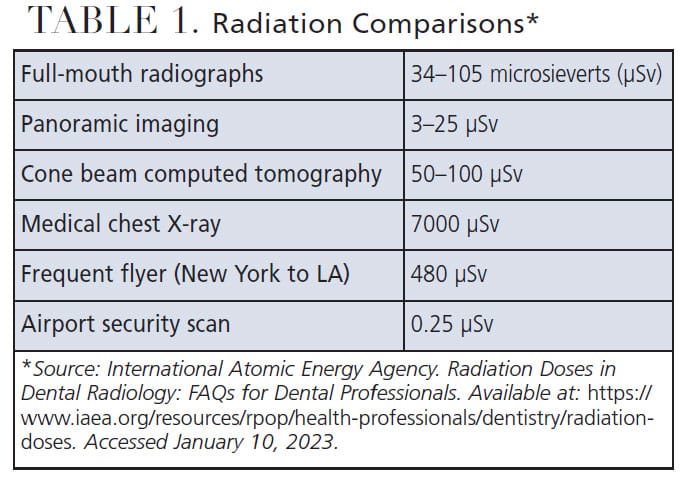
With these position papers demonstrating the usefulness of CBCT scans in implant planning, it would behoove those training today’s implant surgeons to implement this technology with greater emphasis and frequency. A survey of CBCT utilization among U.S. postdoctoral periodontics programs for implant planning showed that while a majority of programs train with this technology, it was still underutilized as part of guided implant therapy.8
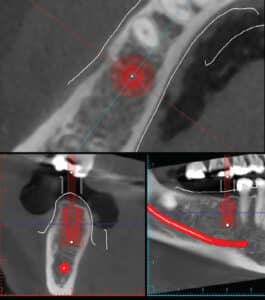
Cone beam scans are also useful in surgical guide fabrication and other digital workflows, such as dynamic navigation (Figure 1). Various working platforms are available commercially in which three-dimensional bony data are merged with intraoral landmarks. The practitioner is then provided an intraoral guide, and the implant is placed with guided assistance.
DIAGNOSING AND MANAGING PERIODONTITIS
Currently, a complete periodontal assessment and a full-mouth radiographic series are still key components in establishing a periodontal diagnosis.7 However, an exact measurement of the alveolar bone height and morphology using CBCT scans could enhance accuracy when assessing different periodontal conditions.9 That noted, the decision to utilize this imaging modality must be reached on a case-by-case basis, because the increased radiation exposure may not be warranted for all patients.7
There have been numerous ex-vivo studies on dry human skulls showing the increased accuracy of cone beam imaging compared to routine periapical radiographs for detecting periodontal intrabony defects.10–12 Misch et al10 found that all defects were detected by CBCT, but only 67% were noted with periapical radiographs. Vandenberghe et al11 further showed that all bony craters and furcation defects were seen with CBCT, compared to only 56% to 71% of bony discrepancies shown with conventional bite-wing and periapical films. And still other work by Fuhrmann et al12 showed similar sensitivity between CBCT and other intraoral films in detecting different experimental defects, including dehiscences, fenestrations and furcation defects.
These ex-vivo studies can produce a valid reference with artificially created bony defects for detection and analysis much more reliably than what occurs naturally in the mouth. But the literature shows these ex-vivo studies should be read with caution. With a dry skull, all images are captured without the added burden of patient movement.13 Also, others will note that in these skull studies, all metal artifacts have usually been removed, reducing bothersome scatter, and the dehydrated skulls result in a faded cementoenamel junction, complicating the main reference point for calculating periodontal osseous defects.14 In summary, although interesting, the results from ex-vivo dry-skull studies should be interpreted with caution.15

Cone beam imaging can also detect bony abnormalities that may be missed as part of a routine clinical and radiographic assessment (Figure 2). However, there is still a lack of literature to support the use of CBCT technology to improve short- and long-term clinical outcomes of periodontal treatment.15 A systematic review found that while helpful in supporting the results of regenerative periodontal therapy, CBCT information may not lead to a better periodontal diagnosis.16 Overall, there is insufficient clinical evidence at this time to support the routine use of CBCT for the diagnosis and treatment of common periodontal defects.15
ADDITIONAL USES FOR CONE BEAM IMAGING
Common locations of localized advanced periodontitis and its bone destruction frequently include interproximal and furcation areas, and these defects are often candidates for regenerative periodontal procedures.17 Cone beam scans provide the ability to evaluate the configuration of these defects, aiding in the diagnosis of their severity and extent. It has been shown that CBCT yields the highest sensitivity and greatest diagnostic accuracy for the detection of these periodontal defects.18 The number of remaining bony walls of the defect often dictates the extent of the periodontal regeneration attainable. With this information, the later success of periodontal regenerative therapy may be made clearer from the CBCT data.
Similarly, CBCT scans can help identify complicating root morphology, such as the presence of developmental root grooves. These, in turn, predispose the tooth to periodontal attachment loss. Developmental grooves most frequently present on maxillary incisors; more specifically, the central incisors (0.28%) and lateral incisors (4.4%).19,20 These grooves are often associated with soft tissue attachment loss and the progression of bacteria subgingivally.20 With prior knowledge of the configuration and extent of the developmental groove, the prognosis of the tooth — along with the success rate of periodontal therapy for tooth retention — can be determined.
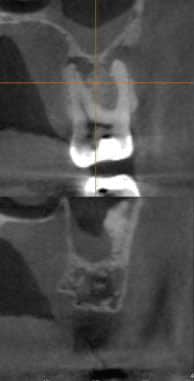
Lastly, from an interdisciplinary perspective, the ability to visualize circumferentially around a tooth with cone beam imaging can help clinicians identify the presence of combined periodontal-endodontic pathology.21 In fact, the literature indicates that peri-radicular pathology can be detected with greater accuracy from CBCT scans than it can from conventional, two-dimensional radiography (Figure 3).22 The impact from this increased accuracy in the diagnosis of periodontal-endodontic lesions translates to more precise treatment planning, improved clinical success, and better overall patient care.
CONCLUSION
Cone beam scanning has given dentists the ability to capture quality images of the dentition and surrounding structures. This modality’s usefulness in dental implant planning can aid the practitioner in the diagnostic phase of case planning, and the CBCT data can then be used when fabricating implant surgical guides. There is no doubt the fine detail of periodontal bony architecture attained with CBCT surpasses that obtained with conventional films — but it has not been shown the added cost of cone beam imaging improves periodontal diagnosis and overall treatment outcome. Nevertheless, CBCT can be useful in analyzing bony regenerative changes and detecting differing root anomalies.
Key Takeaways
- Cone beam computed tomography (CBCT) generates quality images of the dentition and surrounding structures that provide valuable, real-time information for dental implant planning.
- These scans have also been found to aid in the diagnosis and treatment of various periodontal conditions — and these images are captured more quickly and easily than conventional medical computed tomography.2
- Despite the utility of cone beam imaging and no matter how low the radiation dose, exposure is deemed excessive if it does not improve therapeutic outcomes.3,4
- Cone beam scans are also useful in surgical guide fabrication and other digital workflows, including dynamic navigation.
- While complete periodontal assessment and a full-mouth radiographic series are still key components in establishing a periodontal diagnosis,7 an exact measurement of the alveolar bone height and morphology using CBCT scans could enhance accuracy when assessing periodontal conditions.9
- Lastly, from an interdisciplinary perspective, the ability to visualize circumferentially around a tooth with cone beam imaging can help clinicians identify the presence of combined periodontal-endodontic pathology.21
References
- Eke PI, Thornton‐Evans GO, Dye BA, Genco RJ. Advances in surveillance of periodontitis: The Centers for Disease Control and Prevention periodontal disease surveillance project. J Periodontol. 2012;83:1337–1342.
- Acar B, Kamburoglu K. Use of cone beam computed tomography in periodontology. World J Radiol. 2014;6:139–147.
- American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902.
- Walter C, Weiger R, Zitmann N. Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol. 2010;37:436–441.
- Tyndall DA, Price JB, Tetradis S, Ganz SD. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:817–826.
- Mandelaris GA, Scheyer ET, Evans M, et al. American Academy of Periodontology best evidence consensus statement on selected oral applications for cone-beam computed tomography. J Periodontol. 2017;88:939–945.
- McAllister B, Eshraghi VT. Commentary: cone-beam computed tomography — an essential technology for management of complex periodontics and implant cases. J Periodontol. 2017;88:937–938.
- Beals DW, Parashar VP, Francis JR, Agostini GM, Gill A. CBCT in advanced dental education: a survey of U.S. postdoctoral periodontics programs. J Dent Educ. 2020; 84:301–307.
- Mol A, Balasundaram A. In-vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol. 2008;37:319–324.
- Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–1266.
- Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: an in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol. 2008;37:252–260.
- Fuhrmann RA, Bucker A, Diedrich PD. Furcation involvement: comparison of dental radiographs and HR-CT slices in human specimens. J Periodontal Res. 1997;32:409–418.
- Spin-Neto R, Wenzel A. Patient movement and motion artefacts in cone beam computed tomography of the dentomaxillofacial region: a systematic literature review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121:425–433.
- Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:395–401.
- Kim DM, Bassir SH. When is cone-beam computed tomography imaging appropriate for diagnostic inquiry in the management of inflammatory periodontitis? An American Academy of Periodontology best evidence review. J Periodontol. 2017;88:978–998.
- Woelber JP, Fleiner J, Rau J, Ratka-Krüger P, Hannig C. Accuracy and usefulness of CBCT in periodontology: a systematic review of literature. Int J Periodontics Restorative Dent. 2018;38:289–297.
- Liu X, Gao M, Bai Q, Ruan J, Lu Q. Evaluation of palatal furcation groove and root canal anatomy of maxillary first premolar: a CBCT and micro-CT study. Biomed Res Int. 2021;2021:8862956.
- Bagis N, Kolsuz ME, Kursun S, Orhan K. Comparison of intraoral radiography and cone-beam computed tomography for the detection of periodontal defects: an in vitro study. BMC Oral Health. 2015;15:64.
- Withers JA, Brunsvold MA, Killoy WJ, Rahe AJ. The relationship of palato-gingival grooves to localized periodontal disease. J Periodontol. 1981;52:41–44.
- Giner-Lluesma T, Micó-Muñoz P, Prada I, et al. Role of cone-beam computed tomography (CBCT) in diagnosis and treatment planning of two-rooted maxillary lateral incisor with palatogingival groove. Case report. J Clin Exp Dent. 2020;12:e704–e707.
- Ozcan G, Sekerci AE. Classification of alveolar bone destruction patterns on maxillary molars by using cone-beam computed tomography. Niger J Clin Pract. 2017;20:1010–1019.
- Patel S, Wilson R, Dawood A, Mannocci F. The detection of periapical pathosis using periapical radiography and cone beam computed tomography — part 1: pre-operative status. Int Endod J. 2012;45:702–710.
From Decisions in Dentistry. February 2023;9(2)16-18.


