 VIKTORIIANOVOKHATSKA/ISTOCK/GETTY IMAGES PLUS
VIKTORIIANOVOKHATSKA/ISTOCK/GETTY IMAGES PLUS
Periodontal Grafting in Patients With Inadequate Keratinized Gingiva
These grafting procedures will enhance restorative results in periodontal patients with inadequate keratinized gingiva.
This course was published in the October 2019 issue and expires October 2022. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss periodontal grafting techniques and parameters designed to ensure adequate keratinized gingiva and predictable restorative outcomes.
- List clinical considerations to help decide whether grafting is advisable, and scenarios in which free gingival grafts or connective tissue grafts are indicated.
- Explain graft placement techniques and options to make postprocedural recovery more comfortable.
When presented with a patient who has an inadequate zone of keratinized gingiva, dental professionals should consider two periodontal grafting procedures that offer predictable benefits for restorative, esthetic or simply health reasons. The focus of this article is free gingival grafts (FGG) and connective tissue grafts (CTG), which have shown more predictable outcomes than other approaches to grafting. In addition, patient fears about grafting procedures will be addressed, as will options that increase patient comfort and enhance recovery. The latter is germane since patient fears about grafting procedures often center on the potential for painful postoperative sequalae. Finally, the paper will also attempt to answer the clinical question of whether “to graft or not to graft?”
Since the early 1970s, following the work of Lang and Löe,1 experts have agreed that 2 mm of keratinized gingiva will provide adequate stabilization for gingival margins. However, more recent research indicates the possible necessity for a wider zone of keratinized tissue to help prevent further recession — although there is no consensus on a specific measurement.2
Techniques or considerations for determining whether to proceed with a periodontal graft include:
- Clinicians should determine if recession has begun. If not, optimal plaque control and regular dental visits can often stabilize narrow tissue zones. Of course, this requires patient compliance and adequate after-care.3
- Operators can use digital photographs to track progression. To track the progression of gingival recession in borderline cases, take a series of digital photographs with a probe to reference the location of the free gingival margin to more easily track recession should it occur. If the area continues to recede over time, consider a graft.
- A graft is indicated when restoring an area of thin tissue. When planning a restoration — such as a subgingival crown — on a thin tissue area with no initial recession, a graft should be used in most cases prior to restorative treatment, as the preparations, impressing, and provisional restoration will likely disturb an otherwise stable area.4
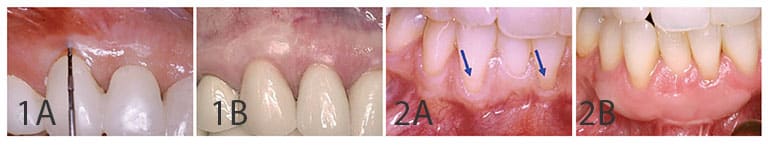
- Clinicians should perform grafting if continued recession is evident. If continued recession is evident after tracking, a graft will often offer reliable stability and a foundation for predictable restorative results. Grafting thin or receded areas prior to placing a restoration helps avoid the disappointment of finding recession (in some cases, even in less than a year later, as illustrated in Figure 1A). This area has a good chance for recession whether a restoration is placed or not.
The following tips will help providers choose which type of graft is appropriate for the case.
FREE GINGIVAL GRAFT
Basically a form of epithelialized palatal graft that involves removal of a thin layer of tissue from the palate to graft at the site of gingival recession, use of an FGG may prevent recession (including recession in a restoration area), as in Figures 1A and 1B. Alternately, it could be used to stabilize tissue at the margin of a current or future crown, or natural tooth, as Figures 2A and 2B illustrate. The FGG procedure has shown predictable results in stopping recession from progressing, especially in areas with non-esthetic requirements, such as the mandibular anterior or posterior.
A case study on epithelized graft procedures, such as the FGG technique, supports the use of this approach over other grafting procedures for mandibular anteriors because it best addresses the specific anatomy of the that region and creates a “tensionless environment during healing.”5 In the study, Berridge et al5 refer to epithelial grafts as the “gold standard” for treating areas of receding keratinized gingiva. They are not, it should be noted (and as stated by Berridge et al), as predictable for root coverage in other areas of the mouth.
As previously mentioned in Item 3, providers should also seriously consider the FGG option at a crown restoration site that presents with thin keratinized tissue because the restoration — and the process to prepare and impress for the restoration — could trigger further destabilization of the tissue and lead to recession of the soft tissue margin.
One criticism of the FGG procedure is that grafts are often bulky and may appear unesthetic. While this is true, clinicians should keep in mind the thickness of graft tissues (which allow differing amounts of subepithelial blood supply) may produce differing color results. If the grafted tissue approximates the thickness of the adjacent tissues, the color blend can be satisfying (Figures 3A and 3B). Alternately, if the tissue is too thick and has a whiter appearance than adjacent tissues, the thicker graft can be thinned after healing with a plasty procedure using either a bur or soft tissue laser.

CONNECTIVE TISSUE GRAFT
In areas where esthetics matter, oral health professionals should consider CTG procedures, as this approach offers highly predictable results for soft tissue coverage of exposed roots.6
As evidenced by the accompanying patient photos, the CTG technique can enhance results in both purely esthetic situations (Figures 4A and 4B), and in conjunction with restorative treatment (Figures 5A and 5B).

Techniques for obtaining root coverage continue to evolve. While it has been used since the mid-1980s, CTG is a relatively new procedure compared to other grafting techniques, with the first FGG article published some 17 years earlier. A 2019 study by Chambrone and Pini Prato6 showed long-term stabilization of the gingival margin and keratinized gingiva in a 20-year span following a CTG procedure. In this study, researchers followed the progress of 45 patients with maxillary gingival recession (Miller class I or II) and measured the stability of the gingival margin at one year, five years, 10 years, 15 years and 20 years.
As the technique has been refined over the past few decades, this study and others show increasingly positive results for root coverage. Consequently, CTG is often recommended for esthetic areas. For example, after a four-year follow-up, Harris7 found the autogenous tissues of a CTG to be much more stable when compared to an acellular dermal graft.

CLARIFYING THE GOALS OF GRAFTING PROCEDURES
It is prudent to remember that FGG is intended to prevent recession from advancing. Professionals can also employ the procedure to prevent recession, with an excellent indication being its use to create stable marginal tissue prior to starting a restoration, as illustrated previously in Figures 1A and 1B in an esthetic application, or in an area not considered esthetic by the patient and not being restored, as in Figures 2A and 2B. Both illustrations show benefits of creating stable tissue margins — one to prevent recession around a restoration, and the other simply for stable tissue health.
By comparison, CTG is used primarily for root coverage, either to enhance esthetics or address root sensitivity. The coverage could be for either purpose. The resultant increased zone of attached and keratinized gingiva will also reduce the chances for continued recession.
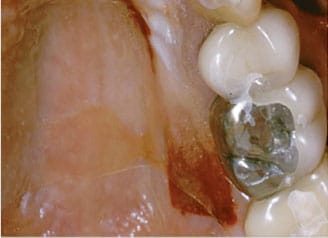
Additionally, it is worth noting that in comparison to an FGG, which is placed in an open window recipient site, a CTG is placed inside an envelope flap (Figure 6). This flap, and the resulting double blood supply coming from the periosteum and overlying flap, could contribute to the viability of tissue over an avascular root surface, which allows for stable soft tissue coverage. In a human histologic study, Bruno and Bowers8 examined the results of this tissue attachment and suggest it indicates stable, predictable tissue.

blood supply. In turn, this enhances the potential for coverage of the avascular root surface.
MANAGING PATIENT CONCERNS AND RECOVERY OPTIONS
Patient fears and objections often become major factors when weighing the question of whether to perform a graft procedure, and operators need to address these concerns. Upon hearing the details of the procedure, many patients fear a painful recovery. Worse, others have heard from friends that a palatal graft is a terrible experience and are thus reluctant to accept treatment, even if the clinical rationale and benefits are solid.
While patients should expect some mild pain or discomfort following a surgical procedure, there are options to make recovery much more comfortable than in years past. One approach that might not be on the radar of many dental professionals is a palatal stent made from vacuum-formed plastic (Figures 7A and 7B).

model.
The palatal stent process involves:
- Taking a maxillary impression and pouring a model.
- Using the model to create a vacuum-formed stent.
- Trimming to avoid the soft palate and gingival tissues.
- Checking the fit on the patient.
- After surgery, placing the stent, along with two thin layers of resorbable collagen over the donor site.
- Patient instructions for use are to leave stent in overnight on the first night, and then wear it full-time for the first week, taking it out only for brushing; after the first week, the patient can use at his or her discretion.
The addition of collagen serves two purposes: pain reduction and almost immediate clotting. The resulting clotting effect helps ensure the patient will not experience postoperative bleeding from the palate. In the author’s experience, with this technique most patients are comfortable or reasonably so — certainly more than they anticipated after hearing the bad publicity often associated with grafting from the palate.
While some clinicians advocate the use of an acellular dermal matrix, or human donor skin, as a way to avoid the allegedly painful experience of taking palatal tissue, the author has found consistent success with stent coverage on the palate, which allows the use of autogenous palatal tissue in a comfortable and predictable way.
the patient’s collagen wound dressing.
FINAL THOUGHTS
Researchers have referred to using palatal tissue as the “gold standard” because it offers solid and predictable results.9 The author concurs with this conclusion, and patient experience over the course of several decades bears out both anecdotal and empirical evidence that FGG and CTG procedures lead to favorable tissue stabilization and/or root coverage. In addition, the stability of tissue around restorations is practically assured, so there is no premature recession around recently placed crowns.
REFERENCES
- Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43:623–627.
- Agudio G, Cortellini P, Buti J, Pini Prato G. Periodontal conditions of sites treated with gingival augmentation surgery compared with untreated contralateral homologous sites: an 18– to 35–year long‐term study. J Periodontol. 2016;87:1371–1378.
- Kim DM, Neiva R. Periodontal soft tissue non-root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(Suppl 2):S56–S72.
- Scheyer ET, Sanz M, Dibart S, et al. Periodontal soft tissue non-root coverage procedures: a consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86(Suppl 2):S73–S76.
- Berridge JP, Johnson TM, Lane JD, Miller PD. Focus on epithelialized palatal grafts. Part 1: multiple adjacent recession defects in the mandibular anterior. Clin Advan Periodont. 2018;8:160–166.
- Chambrone L, Pini Prato GP. Clinical insights about the evolution of root coverage procedures: The flap, the graft, and the surgery. J Periodontol. 2019;90:9–15.
- Harris RJ. A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J Periodontol. 2004;75:734–743.
- Bruno JF, Bowers GM. Histology of a human biopsy section following the placement of a subepithelial connective tissue graft. Int J Periodontics Restorative Dent. 2000;20:225–231.
- Sonick M, Hwang, D. The dependability of connective tissue grafting for the resolution of full-mouth recession. Compend Contin Educ Dent. 2011; 32:48–53.
From Decisions in Dentistry. October 2019;5(9):37–40.




