Guest Editorial: Pathway to Professional Excellence
Helping patients develop and maintain wellness-focused habits and lifestyles is critical to long-term clinical success.
Decisions in Dentistry is devoted to helping dentists and their teams better understand the scope, scale and nature of clinical practice. Most articles are procedure-oriented and focus on the technical and biologic aspects of our rapidly evolving profession. What journals like this seldom discuss, however, are the psychosocial aspects of health care practice that help build powerful, lasting relationships among health care teams, their patients, families and communities.
The premise is simple: If we cannot help patients become motivated toward wellness by controlling their diseases, our treatments will fail. Creating and maintaining that motivation within patients requires an entirely different skill set than the technical and biologic aspects of practice. As our profession evolves, long-term clinical success will be largely predicated on a clinician’s ability to encourage patients to adopt healthy behaviors and embrace preventive health-management strategies.
Building an enduring bond with patients is a primary requirement for ongoing success for any attending dentist and team, but it is no less important for specialists. Patients respond best to office teams whom they like and trust to always put patients’ welfare first.
There is a looming health crisis facing most of the world’s population. In underdeveloped and poorer areas of developed countries, critical needs — such as clean air, food and sanitation — are often unmet, posing significant societal challenges. And in developed countries, poor dietary choices, lack of exercise, alcohol/drug/tobacco abuse, inadequate hygiene, environmental pollution, and unhealthy sexual practices threaten public health. The major difference in these conditions besides the obvious? The bad habits of inhabitants in developed countries are largely self-inflicted diseases of opportunity. The organized health professions must play a key role in both environments by advocating for improved conditions and better choices. Most of the ideas stated here require change — change within the health professions, and change among the populations we serve.
 It has been said that only wet newborns embrace change, but change is ever-present in our lives and practices. The half-life of knowledge shortens by the month, and new equipment, instruments and materials are introduced regularly. The ability to embrace change — and utilize it to our professional and personal advantage — plays a critical role in our happiness and satisfaction as clinicians.
It has been said that only wet newborns embrace change, but change is ever-present in our lives and practices. The half-life of knowledge shortens by the month, and new equipment, instruments and materials are introduced regularly. The ability to embrace change — and utilize it to our professional and personal advantage — plays a critical role in our happiness and satisfaction as clinicians.
This guest editorial offers reflections of a long-term practitioner who was taught psychosocial principles of human behavior, and tried to practice them. Most of these lessons were learned and reinforced in the crucible of private practice, so these are words of experience, not theory. Dentists can build successful practices by using these principles and behaviors to create loyal patient bases that endure.
Success in dental practice — as defined by the concepts of satisfaction, joy, security and sense of worth to others — relates to four broad areas: (1) personal and family security, harmony and wellness; (2) technical competency; (3) biologic understanding; and (4) psychosocial sensitivity. Contemporary health care education tends to stress the middle two, with less regard for the first and last. In today’s practice, much attention is given to treating disease symptoms, often at the expense of controlling or preventing disease and its attendant risks.
As clinicians, each of these four areas must be regarded as an individual responsibility that requires self-directed learning. Hippocrates said, “There are, in effect, two things: To know and to believe one knows; to know is science, to believe one knows is ignorance.” Two of life’s healthiest habits are to be persistently inquisitive and remain open to careful evaluation of new or modified ideas. Yet it is equally important to remember that dentists are, first and foremost, in the “people business.” Whatever practice environment you operate in, strive to build and nurture powerful interpersonal relationships.
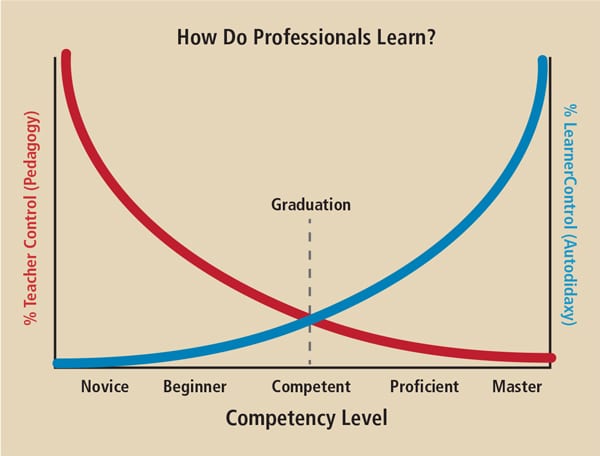
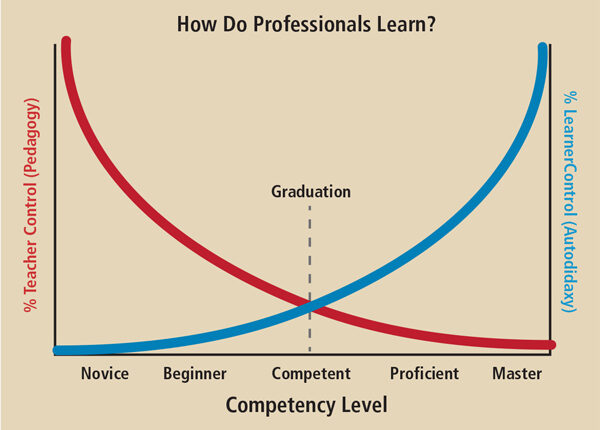
Chambers divided lifelong professional development into five stages of proficiency1 (Figure 1). Based on today’s knowledge half-life, the need for constant learning and revision is greater than ever. With the rapid development of new knowledge about the interrelations of human diseases, dramatic changes in dental examinations and treatment plans will be crucial in order to comply with escalating (and often confusing) standards of care.2–5 Dentists and their teams are expected to keep current on treatment guidelines, and, in the best interest of patients, should be able to defend their treatment choices.
The first three stages of professional development are accomplished in the prelicensure years of dental school, and are the minimum expectations of a practitioner. Following graduation and licensure, however, providers are expected to practice to minimum standards of care without supervision. All learning after that is the clinician’s responsibility. Achieving and maintaining these last two stages — proficiency and mastery — presents a constant professional challenge.
As you seek to stay abreast of emerging technologies and evolving practice standards, don’t neglect the psychosocial aspects of practice that not only contribute to our satisfaction as providers, but also to clinical success. Ultimately, the key to excellence in practice and optimal outcomes is to use the relationships we build to motivate our patients to embrace healthy choices and, ultimately, wellness.
References
- University of the Pacific, Arthur A. Dugoni School of Dentistry. Faculty & Research: Competency-Based Education and Evaluation. Available at: http://dental.pacific.edu/ Faculty_and_Research/Research/Areas_of_Research_Interest/Education_Research_Topic s/Competency-Based_Education_and_Evaluation.htm. Accessed June 7, 2016.
- Lewis K. Professional standards and their escalating impact upon the dental profession. Br Dent J. 2015;218(10):381–383.
- Genco RJ, Williams RC (Eds). Periodontal Disease and Overall Health: A Clinician’s Guide. Ed2. 2014. Available at: http://www.colgateprofessional.com/professionaleducation/ articles/periodontal-disease-and-overall-health-a-clinicians-guide. Accessed June 7, 2016.
- Stefanac SJ, Nesbit SP. Treatment Planning in Dentistry. Ed2. Mosby/Elsevier 2007.
- Little JW, Falace DA, Miller CS, Rhodus NL. Dental Management of the Medically Compromised Patient. Ed8. Elsevier 2013.
- Maslow A. Motivation and Personality. Ed2. Harper and Row 1954.
- Mostofsky DL, Fortune F. Behavioral Dentistry. Ed2, Wiley Blackwell 2014.
- Goleman D. Emotional Intelligence. Bantam Books 1995.
- . Sewell C, Brown P. Customers for Life. Doubleday 2002.
- Clow D. A Few Words From the Chair: A Patient Speaks to Dentists. Selfpublished 2008.
- Combs AW, Gonzalez DM. Helping Relationships: Basic Concepts for Helping Professions. Ed4. Allyn & Bacon 1994.
- Green ES, Kohn N. Selection, Hiring, and Training of Dental Auxiliaries. WB Saunders 1970.
- Creagan E. The Mayo Clinic Plan for Healthy Aging. Mayo Clinic Health Solutions 2006.
- Homoly P. Making it Easy for Patients to Say Yes. Self-published 2005.
- Harris NO, Garcia-Godoy F. Primary Preventive Dentistry. Ed8. Pearson/Prentice- Hall 2013.
- Penn Dental Medicine. Community Outreach/Service Learning. Available at: http://www.dental.upenn.edu/academic_programs_admissions/dmd_program/commu nity_outreach. Accessed June 7, 2016.
- Substantive Action Report. Available at: http://www.ada.org/~/media/ADA/ Publications/Files/SubstantiveActionReport_March2016CMC_2016Apr11.pdf?la=en. Accessed June 7, 2016.
From Decisions in Dentistry. July 2016;1(09):12–13.


