 OLEKSANDR HRYTSIV/ISTOCK/GETTY IMAGES PLUS (SUBJECT IS A MODEL)
OLEKSANDR HRYTSIV/ISTOCK/GETTY IMAGES PLUS (SUBJECT IS A MODEL)
Oral Health Management for Patients with Autism Spectrum Disorder
Dental teams will benefit from an understanding of the oral health challenges faced by this patient population, as well as strategies for successful management.
This course was published in the March 2022 issue and expires March 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the clinical manifestations of autism spectrum disorder (ASD) and how it is diagnosed.
- Discuss the literature describing the association between ASD and dental caries.
- Describe treatment strategies to improve the oral health of patients with ASD.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by persistent impairment in social communication, and restricted, repetitive patterns of behavior and interest.1 The global occurrence of ASD is approximately 1%, while in the United States, about one in 44 individuals is diagnosed with ASD, most frequently during childhood.2,3 The age of diagnosis can vary, but 2 years is typically the age at which most diagnoses are made. Boys are four times more likely to be affected by ASD than girls.2 In light of these statistics, oral health professionals are likely to encounter these patients in the provision of care, and thus will benefit from an understanding of the oral health challenges faced by this patient population.
Characteristics of ASD include difficulty communicating and relating with others, impaired social interaction, and repetitive behaviors.4 Children with ASD may also display abnormal emotional and linguistic development, intellectual disability, and sensory perception problems.5,6 Early signs and symptoms may include absence of speech, language and other developmental delays, and lack of eye contact.6 Among those diagnosed after age 8, the signs and symptoms may also include hand flapping, extreme tantrums or outbursts, self-injurious behavior, and head banging.7
Some evidence shows that genetics play a role in the etiology of ASD.8,9 Studies have shown that up to 40% of ASD cases present with genetic aberrations.10 Environmental factors may also increase the risk of ASD. These include both exogenous factors, such as maternal exposure to tobacco and alcohol, and endogenous factor, including advanced parental age at conception, oxidative stress, or mitochondrial dysfunction.9,11 Some evidence suggests that maternal stress may contribute to an increased occurrence of ASD traits.9–11
OBTAINING A DIAGNOSIS
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the current standard used for diagnosis of all categories of ASD. After the American Psychiatric Association adopted a new standard for ASD in the DSM-5 criteria in 2013, a patient with any of the following four conditions — autistic disorder, Asperger syndrome, pervasive developmental disorder, or pervasive developmental disorder not otherwise specified (PDD-NOS) — is now diagnosed under the umbrella of ASD.12 Previously, ASD was deemed more clinically severe than PDD-NOS.13 On the other hand, some disorders previously diagnosed within the spectrum are no longer included in the DSM-5 diagnosis of ASD. For instance, social communication disorder, which is the absence of both verbal and nonverbal abilities to form social connections, is now classified separately from ASD.
When parents/caregivers or primary healthcare providers first suspect ASD, an initial screening exam is completed that includes both a patient and provider questionnaire, along with a physical examination. If ASD is tentatively diagnosed during the screening exam, the patient will be referred to a specialist who will perform further testing to confirm the diagnosis. This comprehensive testing typically involves a series of both physical and mental assessments, and may include genetic testing as well. Specific tests and diagnostic instruments are approved by the American Academy of Pediatrics and American Psychiatric Association to confirm a diagnosis and reduce the likelihood of misdiagnosis; these assays include the Ages and Stages Questionnaire, Communication and Symbolic Behavior Scales, Parents Evaluation of Developmental Status, Modified Checklist for Autism in Toddlers, and the Screening Tool for Autism in Toddlers and Young Children.6,11,12
Problems with social interaction, attention deficit, and executive functioning frequently affect the lives of individuals with ASD. These issues can make caregiving by family members, educators and healthcare providers challenging.14,15 One study suggests that — due to sensory, motor and cognitive deficiencies — individuals with ASD are twice as likely to lack essential oral healthcare than those without developmental disabilities.16 As a result of these barriers, individuals with ASD may be at increased risk for dental caries.17,18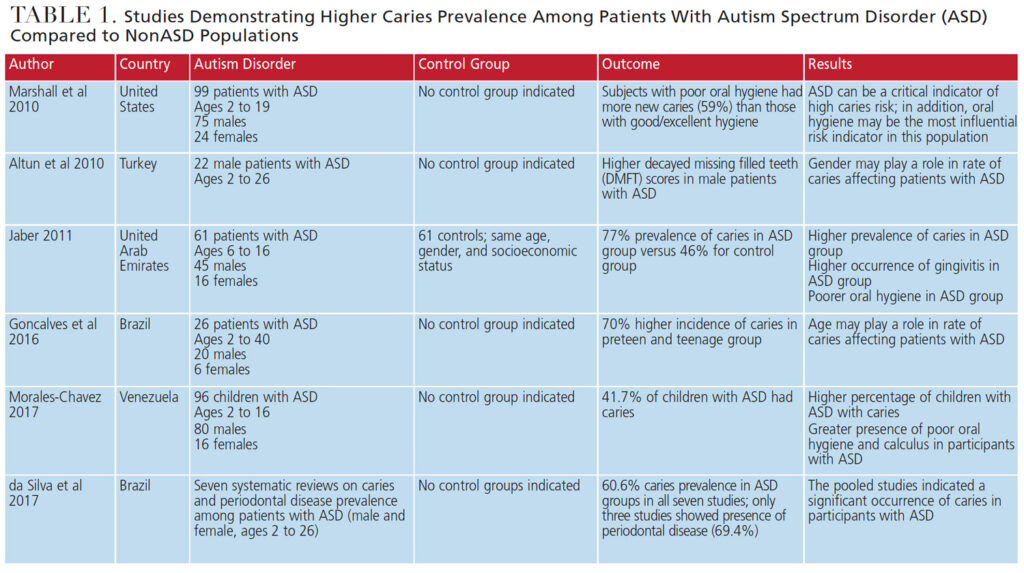
AUTISM SPECTRUM DISORDER AND CARIES
Caries is the most common chronic disease of childhood, impacting 45.8% of those between the ages of 6 and 19 in the United States.1,19 Nine out of 10 U.S. adults (ages 19 to 64) also have experienced caries in their permanent teeth.1 These numbers emphasize the importance of early intervention, prevention, and treatment to promote optimal oral health. Some studies suggest that adults and children with ASD have a higher prevalence of dental caries, malocclusion, enamel hypoplasia, gingivitis and periodontitis.4 Other studies, however, show that patients with ASD experience a similar or even lower caries prevalence than those without ASD. This variation may be the result of differences on how various studies score caries prevalence, demographics of the population studied (such as age and gender), oral hygiene abilities, diet, and access to professional dental care.20–23
While inconsistencies exist in ascertaining caries prevalence among those with ASD, a number of studies focused on children, adolescents and young adults.24,25 For example, in 2016, Gonçalves et al26 concluded that their preteen to teenage subjects with ASD showed an incidence of caries averaging 70%. Other studies found that children and young adults with ASD were at high risk for caries.27,28 Table 1 details additional studies that show a higher prevalence of caries in those with ASD than nonASD subjects.
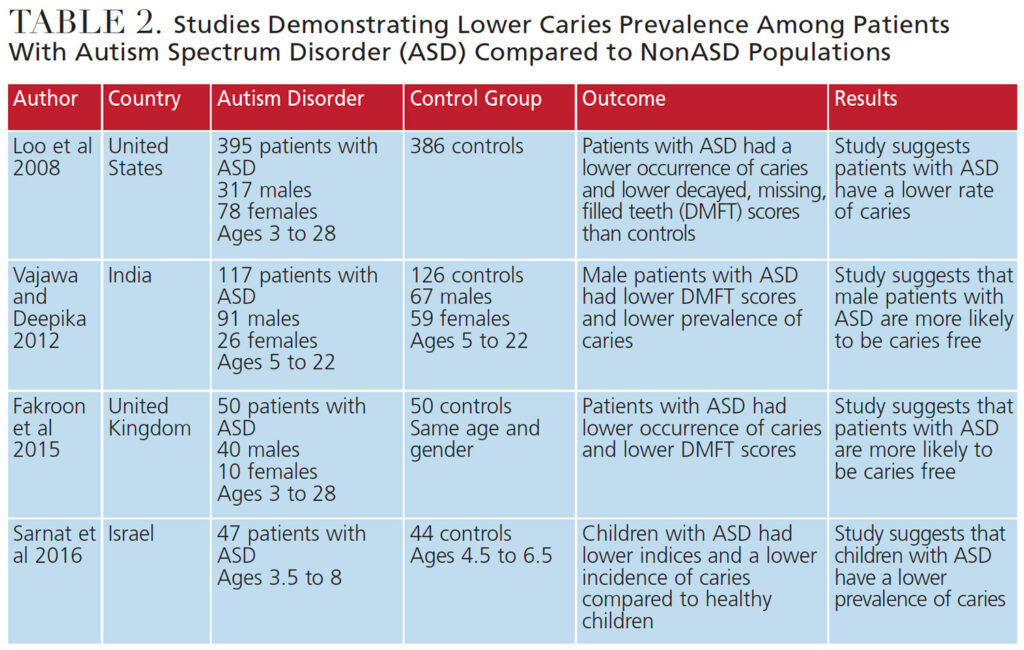
Conversely, some studies revealed lower rates of caries in children with ASD. In 2008, Loo et al29 observed significantly lower rates of caries in children with ASD compared to those without ASD. Table 2 explores additional studies demonstrating a lower prevalence of caries in patients with ASD compared to nonASD populations.
Furthermore, Table 3 recaps two studies that observed no difference in caries prevalence between patients with ASD and nonASD subjects. The inconsistencies in these studies reveal the need for further research with larger population groups.
DENTAL TEAM’S ROLE IN CARIES PREVENTION
Patients with ASD may avoid dental treatment due to sensory processing deficits that can create anxiety, often leading to uncooperative behavior during the dental visit.30,31 Reducing anxiety by desensitization and implementing specific treatment strategies prior to, and during, dental appointments are effective when caring for patients with ASD.32,33 By facilitating the provision of dental care for this patient population in traditional private practice, the burden of seeking treatment under general anesthesia or hospital-based providers is eased. Dental practitioners play an important role in this process and can help significantly improve oral hygiene and reduce caries incidence.
Dental teams can improve oral healthcare for patients with ASD by providing the following:
- Verbal preparation for the patient and parent/caregiver prior to treatment
- Firm, deep touch (rather than a light touch)
- Reclining the dental chair prior to patient seating
- Dark glasses for the patient to wear to block out bright lights
- Headphones to decrease the noise associated with dental care
- Various textures and tastes in prophylaxis pastes
- Weighted blanket to provide comfort
- Management of certain dental tools and practices to address the needs of individual patients34
Effective communication with patients with ASD and their parents/caregivers is critical to supporting oral health and reducing caries risk. Oral health professionals can help this patient population address risks caused by diet, functional habits, and the presence of xerostomia due to medication usage.4 For instance, behavioral and educational interventions can be introduced to reduce the consumption of sugar-sweetened beverages.35 In addition, pamphlets, posters, website links, books and videos can be recommended to patients with ASD and their caregivers. Pretreatment desensitization techniques are also available on smartphone and tablet apps that help patients with ASD and their parents/caregivers prepare for the dental office experience.30
Oral hygiene instruction is imperative for improving the oral health of patients with ASD. Caries risk assessment tools, such as those developed by the American Dental Association and the University of California, San Francisco School of Dentistry (caries management by risk assessment), can be instrumental in preventing caries among patients with ASD.28 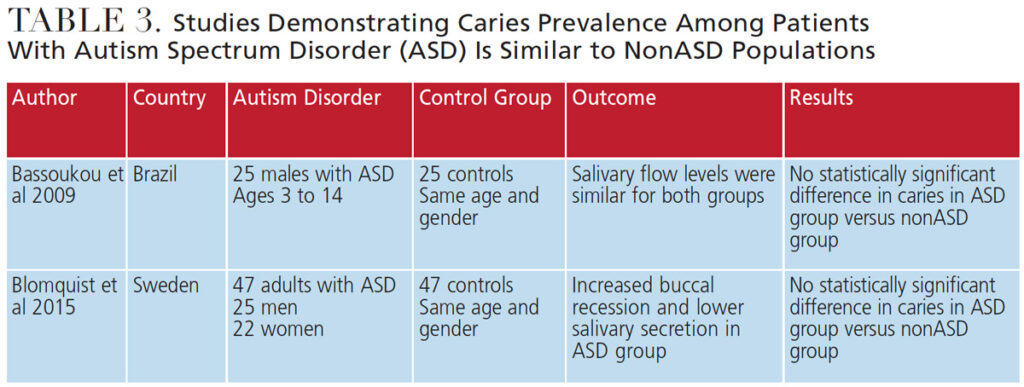
CONCLUSION
As the incidence of ASD continues to increase, it behooves oral healthcare providers to be trained in special needs care while attending dental, dental hygiene, or dental assistant school — and, following graduation, seek continuing education on effective treatment strategies for this population. Dao et al36 found that much improvement is needed in the application and delivery of education regarding patients with special needs, especially in undergraduate dental education programs.
While it remains uncertain whether those with ASD are at higher risk for caries than the general population, it is clear that dental personnel are key to helping these patients achieve and maintain optimal oral health. Clinicians should seek further education to support their efforts to ensure effective care for this patient population, and educate patients and parents/caregivers about strategies to improve and maintain oral health for a lifetime.
REFERENCES
- Shi B, Wu W, Dai M, et al. Cognitive, language and behavioral outcomes in children with autism spectrum disorders exposed to early comprehensive treatment models: a meta-analysis and meta-regression. Front Psychiatry. 2021;12:1.
- U.S. Centers for Disease Control and Prevention. Autism. Available at: cdc.gov/ncbddd/autism/data.html. Accessed January 25, 2022.
- Autism Speaks. What Is Autism? Available at: autismspeaks.org/what-autism. Accessed January 25, 2022.
- Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. 2011;19:212–217.
- Bartolome-Villar B, Mourelle-Martinez MR, Dieguez-Perez M, Nova-Garcia MJ. Incidence of oral health in pediatric patients with disabilities: sensory disorder and autism spectrum disorder. Systematic review II. J Clin Exp Dent. 2016;8:e344–e351.
- DePalma AC, Raposa KA. Building bridges: dental care for patients with autism. Available at: pathfindersforautism.org/docs/BuildingBridges1.pdf. Accessed January 25, 2022.
- Lyall K, Croen L, Daniels J, et al. The changing epidemiology of autism spectrum disorders. Annu Rev Public Health. 2017;38:81–102.
- Sanchack KE, Thomas CA. Autism spectrum disorder: primary care principles. Am Fam Phys. 2016;94:972–979.
- Siu MT, Weksberg R. Epigenetics of autism spectrum disorder. Adv Exp Med Biol. 2017;978:63–90.
- Jeste SS, Geschwind DH. Disentangling the heterogeneity of autism spectrum disorder through genetic findings. Nat Rev Neurol. 2014;10:74–81.
- Chaste P, Leboyer M. Autism risk factors: Genes, environment, and gene-environment interactions. Dialogues Clin Neurosci. 2012;14:281–292.
- Lord C, Bishop SL. Recent advances in autism research as reflected in DSM-5 criteria for autism spectrum disorder. Annu Rev Clin Psychol. 2015;11:53–70.
- Zhang Y, Lin L, Liu J, Shi L, Lu J. Dental caries status in autistic children: a meta-analysis. J Autism Dev Disord. 2020;50:1249–1257.
- Topal Z, Samurcu ND, Tufan AE, Semerci B. Social communication disorder: a narrative review on current insights. Neuropsychiatr Dis Treat. 2016;14:2039–2046.
- Cooper M, Martin J, Langley K, Hamshere M, Thapar A. Autistic traits in children with ADHD index and clinical and cognitive problems. Eur Child Adolesc Psychiatry. 2014;23:23–24.
- Onol S, Kirzioglu Z. Evaluation of oral health status and influential factors in children with autism. Niger J Clin Pract. 2018;21:429–435.
- Pi X, Liu C, Li Z, Guo H, Jiang H, Du M. A meta-analysis of oral health status of children with autism. J Clin Pediatr Dent. 2020;44:1–7.
- Stein LI, Leah I, Polido JC, Najera SO, Cermak SA. Oral care experiences and challenges in children with autism spectrum disorders. Pediatr Dent. 2012;34:387–391.
- Chi DL, Scott JM. Added sugar and dental caries in children: a scientific update. Dent Clin North Am. 2019;63:17–33.
- Bassoukou IH, Nicolau J, Dos SM. Saliva flow rate, buffer capacity, and pH of autistic individuals. Clin Oral Investig. 2009;1:23–27.
- Latifi-Xhemajli B, Begzati A, Kutlovci T, Ahmeti D. Dental health status of children and adolescents with special health care needs. J Int Dent Med Res. 2018;11:945–949.
- Vajawat M, Deppika PC. Comparative evaluation of oral hygiene practices and oral health status in autistic and normal individuals. J Int Soc Prev Community Dent. 2012;2:58–63.
- Sarnat H, Samuel E, Ashkenazi-Alfasi N, Peretz B. Oral health characteristics of preschool children with autistic syndrome disorder. J Clin Pediatr Dent. 2016;40:21–25.
- Fakroon S, Arheiam A, Omar S. Dental caries experience and periodontal treatment needs of children with autism spectrum disorder. Eur Arch Paediatr Dent. 2015;16:205–209.
- Morales-Chavez MC. Oral health assessment of a group of children with autism disorder. J Clin Pediatr Dent. 2017;4:147–150.
- Gonçalves LT, Gonçalves FY, Noguera BM, et al. Conditions for oral health in patients with autism. Int J Odontostomat. 2016;10:93–97.
- da Silva SN, Gimenez T, Souza RC, et al. Oral health status of children and young adults with autism spectrum disorders: systemic review and meta-analysis. Int J Pediatr Dent. 2017;27:388–398.
- Marshall J, Sheller B, Manci L. Caries-risk assessment and caries status of children with autism. Pediatr Dent. 2010;32:69–75.
- Loo CY, Graham RM, Hughes CV. The caries experience and behavior of dental patients with autism spectrum disorder. J Am Dent Assoc. 2008;139:1518–1524.
- Elmore JL, Bruhn AM, Bobzien JL. Interventions for the reduction of dental anxiety and corresponding behavioral deficits in children with autism spectrum disorder. J Dent Hyg. 2016;90:111–120.
- Capozza LE, Bimstein E. Preferences of parents of children with autism spectrum disorder concerning oral health and dental treatment. Pediatr Dent. 2012;34:480–484.
- Kuhaneck HM, Chisolm EC. Improving dental visits for individuals with autism spectrum disorders through an understanding of sensory processing. Spec Care Dent. 2012;32:229–233.
- Cermak SA, Duker LI, Williams ME, Dawson ME, Lane CJ, Polido JC. Sensory adapted dental environments to enhance oral care for children with autism spectrum disorders: a randomized controlled pilot study. J Autism Dev Disord. 2015;45:2876–2888.
- Burgette JM, Rezaie A. Association between autism spectrum disorder and caregiver reported dental caries in children. JDR Clin Trans Res. 2020;5:254–261.
- Zoellner JM, Hedrick VE, You W, et al. Effects of a behavioral and health literacy intervention to reduce sugar-sweetened beverages: a randomized-controlled trial. Int J Behav Nutr Phys Act. 2016;13:38.
- Dao LP, Zwetchkenbaum S, Inglehart MR, Habil P. General dentists and special needs patients: does dental education matter? J Dent Educ. 2005;69:1107–1115.
From Decisions in Dentistry. March 2022;8(3)34-36,39.




