 HAILSHADOW/ISTOCK/GETTY IMAGES PLUS
HAILSHADOW/ISTOCK/GETTY IMAGES PLUS
Managing Measles in the Dental Setting
With the increasing incidence of measles in the United States, dental professionals should be able to recognize this disease and understand the related oral health considerations.
This course was published in the December 2019 issue and expires December 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define measles and identify reasons for the resurgence of measles.
- Discuss prevention, diagnosis and treatment of this disease.
- List the role of oral health professionals in curbing the rise in measles cases.
Once thought to be eradicated in the United States, measles (rubeola) is one of the most contagious infectious diseases — and incidence is increasing in this country. Prior to 1912, when measles became a nationally notifiable disease, incidence was difficult to determine.1 However, in the first decade of mandatory reporting of diagnosed cases, an average of 6000 measles-related deaths were reported each year.1
In 1954, John F. Enders, PhD, and Thomas C. Peebles, MD, used blood samples from ill children in Boston to isolate the virus in order to develop a vaccine. The initial vaccine became available in 1963 and was further refined in 1968.1 The current vaccination includes measles and mumps, and is known as the measles, mumps and rubella (MMR) vaccine (while another form includes mumps, rubella and varicella).
The recommendations for vaccination against measles include two doses of the MMR vaccine beginning at 12 to 15 months. The initial dose provides individuals with a 90% to 95% immunity.2 A secondary dose of MMR is given typically between the ages of 4 and 6.3 With the second dose of MMR, immunity increases to 99.7%.2 With the advent of the MMR vaccination, the incidence of the disease decreased such that in 2000, measles was declared eliminated from the U.S., as there had been no occurrences for more than 12 months.1
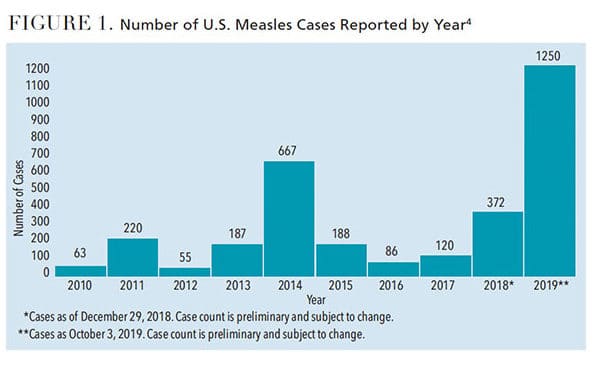
Today, however, this preventable disease is on the rise again. Between January 1 and October 3, 2019, 1250 individual cases of measles had been confirmed in 31 states (Figure 1).4 Outbreaks have been linked with travel to areas where the disease is still endemic, such as Europe, Asia/Pacific and Africa.5,6 Other reasons for the increase include MMR vaccination hesitancy and vaccine refusal.
Oral health professionals may not be familiar with the signs and symptoms of active measles. With the recent rise in incidence, however, it behooves dental teams to be able to recognize measles and understand its related oral health considerations.
Measles virus is transmitted through the respiratory route via coughing and sneezing, but transmission can also occur through direct contact with secretions. Once an individual is infected, clinical signs will appear within nine to 19 days.7 Measles can affect individuals of all ages.8 Risk factors include children with immunodeficiency, such as human immunodeficiency virus, leukemia, or those taking corticosteroids. Additional risk factors involve travel to areas where measles is endemic, individuals whose parents declined to immunize the child, and infants who lose passive antibodies before the age of routine immunization.8,9 Malnutrition, pregnancy and vitamin A deficiency are also known risk factors for measles.8
CLINICAL PRESENTATION
Measles cases typically begin with a high fever (up to 104°F or more) that lasts for four to seven days. The prodromal phase is also characterized by the classic triad of cough, coryza (head cold, fever and sneezing) and conjunctivitis (red eyes), known as the “3Cs.” Other symptoms may include malaise, anorexia, photophobia, periorbital edema, myalgias and diarrhea. Adults may experience a transient hepatitis.9
Clinical measles begins with small Koplik’s spots on the buccal mucosa, considered to be pathognomonic for the disease (Figure 2). The lesions can be numerous small, blue-white macules surrounded by erythema.9,10 Occurring one to two days prior to the characteristic maculopapular skin rash, Koplik’s spots may appear on the buccal mucosa, as well as the labial mucosa and soft palate — in some cases, however, they may not occur at all.10,11 Other oral manifestations associated with measles include candidiasis, necrotizing ulcerative gingivitis, and necrotizing stomatitis if the individual is experiencing severe malnutrition. Pitted enamel hypoplasia of developing permanent dentition may occur in severe cases of measles in early childhood. Enlargement of lingual and pharyngeal tonsils may be found during the course of illness.10

As the disease progresses, the cutaneous rash generally erupts approximately 14 days after exposure to the virus. Erythematous macules and papules begin on the face, head and neck. Within 48 hours, the lesions coalesce to patches that spread to the trunk and extremities. During this period, patients are most ill. The rash tends to disappear at the location where it first appeared, and fades after five to seven days.8,9
Individuals who were vaccinated for measles between 1963 and 1967 using the original killed-virus measles vaccine may have incomplete immunity and are at risk for atypical measles.8,9 During this time, the vaccine was administered to U.S. children who were approximately 1 year old. Atypical measles presents with milder symptoms that include prodromal signs and symptoms of fever, headache, abdominal pain and myalgias, which precedes a rash. The rash begins on the hands and feet and spreads centripetally (moving toward the center). Fortunately, the live-attenuated MMR vaccine replaced the killed vaccine in 1967 and is not associated with atypical measles.8,9
DIAGNOSIS AND TREATMENT
The diagnosis of measles is often made through the classic clinical presentation. However, laboratory confirmation can be made through serologic testing using measles-specific IgM or IgG titers or viral culture using throat or nasal swabs.8 Prior to the presentation of the rash, measles can mimic other diseases and conditions, including influenza, croup, other viral illnesses and pneumonia. Once the rash develops, other differential diagnoses may include allergic drug reactions, Epstein-Barr virus, infectious mononucleosis, Kawasaki disease, Rocky Mountain spotted fever, toxic shock syndrome, scarlet fever, fifth disease, rubella (German measles) and varicella (chickenpox).8,9
Because measles is caused by a virus, there is no known cure. Treatment chiefly consists of good hydration with fluids, rest, antipyretics and vitamin A supplementation. In some cases in which an individual is markedly febrile, dehydration occurs and intravenous rehydration is required.
Most cases of measles are uncomplicated and resolve in seven to 10 days after the onset of illness. Secondary bacterial infections, such as otitis media or pneumonia, will need to be treated with antibiotics. On rare occasions, the virus infects the central nervous system, causing encephalitis-related complications. One of the neurologic complications is acute disseminated encephalomyelitis. This disease, which can be fatal, is characterized by demyelination resulting in ataxia, motor and sensory loss, and mental status changes.12 Measles inclusion body encephalitis is another neurologic complication that typically occurs in young infants or immunocompromised individuals who cannot clear the infection. Symptoms include mental status changes, focal seizures, and/or visual or hearing loss that occurs 12 months after immunization or acute measles infection, followed by rapid disease progression, coma and death.12–14 The third, and more rare type of neurologic complication is subacute sclerosing panencephalitis. This disease occurs several years after a normal episode of measles and begins with a change of behavior and intellectual decline, progressing to myoclonic seizures, ataxia and death within one to three years. Subacute sclerosing panencephalitis has been exclusively associated with measles infection (and not the MMR vaccine), but how it spreads throughout the central nervous system is unknown.7,15,16
PREVENTIVE STRATEGIES
In cases in which the MMR vaccine cannot be safely administered — such as in pregnant women or immunocompromised patients — travel or exposure to areas where the virus is active should be limited.6 To prevent measles from becoming endemic in the U.S., the herd immunity threshold must be maintained. This refers to the minimum percentage of a community that is immunized against a particular disease in order to prevent an epidemic.17 For measles, the minimum herd immunity threshold is between 93% and 95% of the population vaccinated.18 In 2015, the National Immunization Survey found that only 72.2% of children between the ages of 19 months and 35 months were fully vaccinated.19 This gap in protection allows periodic outbreaks of the virus.
VACCINE REFUSAL
Parents or caregivers may refuse to have their child vaccinated due to medical reasons or nonmedicinal exemptions (NMEs), which encompass vaccine confidence and concern, philosophical objections and religious barriers.20 Medical reasons for opting out of MMR vaccination include a severely compromised immune system, anaphylaxis reaction to a previous vaccine component, pregnancy, or a family history of altered immunocompetence.21
Of clinical note, NMEs are on the rise in the U.S. (Figure 3).22 In 2016, 18 states allowed NMEs for vaccination of children prior to registering for school. Olive et al22 analyzed data from these states and discovered that 12 of the 18 states demonstrated an upward trend in NMEs since 2009. Upon further examination of data at the county level within each state, researchers discovered that several large metropolitan areas had significant numbers of NMEs. These data suggest that if an outbreak occurs in these densely populated areas, measles would spread rapidly.22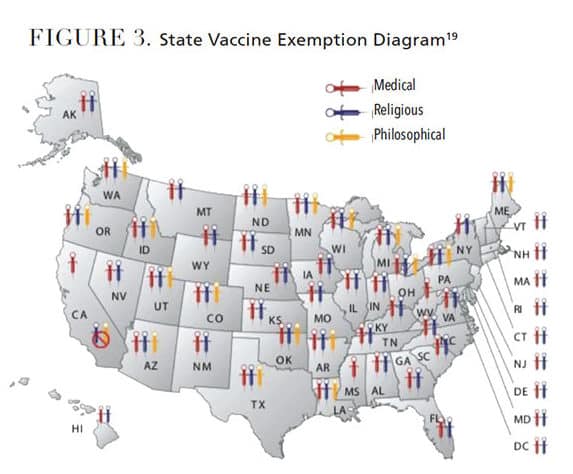
Another important aspect of vaccine hesitancy is parental beliefs regarding immunizations. Cacciatore et al20 found that a low confidence in the safety or efficacy of immunizations was associated with a greater likelihood of delay or refusal of childhood vaccinations. Social media is often used to spread unfounded beliefs in vaccine safety and efficacy.2 No scientific evidence supports any link between the MMR vaccination and autism.2,23,24 In fact, a recent study demonstrates MMR vaccination neither increases the risk of autism nor triggers autism in susceptible children.24 This study refutes the concern that MMR vaccination is associated with clustering of autism cases after vaccination.24
A final component to NMEs is family religious or philosophical beliefs. According to Wombwell et al,5 the primary components of the rubella vaccine come from aborted fetal tissue and animal-derived gelatins. Religious groups may have their own doctrines when it comes to these components; however, it should be noted that religious beliefs may be a determining factor for vaccination acceptance or refusal.
POSTEXPOSURE PRECAUTIONS
Oral health professionals are well positioned to support primary prevention. A main line of defense against spreading infectious diseases is assessment of the patient’s medical history. As such, all patients should have a full medical history taken and reviewed at each appointment. Collecting immunization information is also important, as it provides the opportunity to encourage vaccination for prevention of infectious diseases.
For patients who enter the office displaying symptoms of illness, appropriate infection control measures are paramount. As previously noted, measles is spread via coughing, sneezing and contact with infectious mucous secretions. For this reason, patient masks should be available in the reception area, along with a hand sanitizer dispenser. Furthermore, one of the first presenting symptoms for measles is hyperpyrexia (high fever). Therefore, collecting and assessing vital signs, including temperature, for a symptomatic patient is a critical factor in preventing further transmission of the virus.
Most important, if a patient is displaying signs and symptoms of measles infection, precautions must be implemented. First, dental treatment should be deferred and the patient immediately referred to his or her primary physician for diagnosis and treatment.25 Second, as measles is a nationally notifiable disease, oral health professionals need to be well versed in the procedures and protocols used to notify state health departments. The dental office is required to contact the state health department to document the case and ensure notification is rendered to other potentially exposed individuals.25 Finally, dental teams are encouraged to confirm that all office staff members have updated immunizations to prevent spreading the virus to potentially unvaccinated patients and family members.25
Once patients with measles are dismissed from the dental office and return home, they, too, must exercise precautions. Family members, friends and school contacts should be advised that measles is highly contagious, and infected family members should be isolated. The recommended isolation period is four days before to four days after the rash manifests.8,9 Individuals who have not been fully vaccinated should receive the MMR vaccine as soon as possible.9
CONCLUSION
Measles is a highly contagious — yet preventable — infectious disease that is resurging in the U.S. To prevent its spread, oral health professionals should be familiar with the systemic and oral signs and symptoms of this disease. As a primary line of defense, clinicians must be informed of appropriate preventive efforts and postexposure precautions. Furthermore, it is the dental team’s responsibility to support and advocate for MMR vaccination in order to reduce the prevalence of measles among the U.S. population.
REFERENCES
- U.S. Centers for Disease Control and Prevention. Measles History. Available at: cdc.gov/measles/about/history.html. Accessed September 26, 2019.
- DiPaola F, Michael A, Mandel ED. A casualty of the immunization wars: the reemergence of measles. JAAPA. 2012;25:50–54.
- U.S. Centers for Disease Control and Prevention. Measles Vaccination. Available at: cdc.gov/measles/vaccination.html. Accessed September 26, 2019.
- U.S. Centers for Disease Control and Prevention. Number of Measles Cases Reported by Year. Available at: cdc.gov/measles/cases-outbreaks.html. Accessed September 26, 2019.
- Wombwell E, Fangman MT, Yoder AK, Spero DL. Religious barriers to measles vaccination. J Comm Health. 2015;40:597–604.
- U.S. Centers for Disease Control and Prevention. Traveler’s Health. Available at: cdc.gov/travel. Accessed September 26, 2019.
- Laksono BM, DeVries RD, McQuaid S, et al. Measles virus host invasion and pathogenesis. Viruses. 2016;8:210.
- Chen S, Steele RW. Measles. Available at: https://emedicine.medscape.com/article/966220-overview. Accessed September 26, 2019.
- Koenig KL, Alassaf W, Burns MJ. Identify-isolate-inform: A tool for initial detection and management of measles patients in the emergency department. West J Emerg Med. 2015;16:212–219.
- Neville BW, Damm DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology. 4th ed. St. Louis: Elsevier; 2016:234–236.
- Regezi JA, Sciubba JJ, Jordan RCK. Oral Pathology: Clinical Pathologic Correlations. 7th ed. St. Louis: Elsevier; 2017:10–11.
- Griffin DE. Measles virus and the nervous system. Handb Clin Neurol. 2014;123:577–590.
- Freeman AF, Jacobsohn DA, Shulman ST, et al. A new complication of stem cell transplantation: measles inclusion body encephalitis. Pediatrics. 2004;11:657–660.
- Buchanan R, Bonthius DJ. Measles virus and associated central nervous system sequelae. Semin Pediatr Neurol. 2012;19:107–114.
- Rubin E, Reisner HM. Essential of Rubin’s Pathology. 6th ed. Philadelphia: Lipplincott Williams & Wilkins; 2014:199–200.
- Ludlow M, McQuaid S, Milner D, et al. Pathological consequences of systemic measles virus infection. J Pathol. 2015:235:253–265.
- Glick M. Vaccine hesitancy and unfalsifiability. J Am Dent Assoc. 2015;146:491–493.
- World Health Organization. Critical Immunity Thresholds for Measles Elimination. Available at: who.int/immunization/sage/meetings/2017/october/2._target_immunity_levels_FUNK.pdf20. Accessed September 26, 2019.
- National Vaccine Information Center. State Vaccine Exemptions. Available at: nvic.org/vaccine-laws/state-vaccine-requirements.aspx. Accessed September 26, 2019.
- Cacciatore MA, Nowak GJ, Evans NJ. It’s complicated: The 2014–2015 U.S. measles outbreak and parents’ vaccination beliefs, confidence, and intentions. Risk Analysis. 2018;38:2178–2192.
- U.S. Centers for Disease Control and Prevention. Contraindications and Precautions. Available at: cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html. Accessed September 26, 2019.
- Olive JK, Hotez PJ, Damania A, Nolan M. The state of the antivaccine movement in the united states: a focused examination of nonmedical exemptions in states and counties. PLOS Medicine. 2018;15:1–10.
- Institute of Medicine. Adverse effects of vaccines: Evidence and Causality. Available at: http://vaccine-safety-training.org/tl_files/vs/pdf/13164.pdf. Accessed September 26, 2019.
- Hviid A, Hansen JV, Frisch M, Melbye M. Measles, mumps, rubella vaccination and autism: a nationwide cohort study. Ann Intern Med. 2019;170:513–520.
- Gordon SC, MacDonald NE, OSAP, The Safest Dental Visit. Managing measles in dental practice: a forgotten foe makes a comeback. J Am Dent Assoc. 2015;146:558–560.
From Decisions in Dentistry. November/December 2019;5(10):46—49.




