Oral Health Implications of Antiresorptive Medications
Due to the potential adverse oral health effects associated with these drugs, special care is needed when treating this patient group.
This course was published in the April 2018 issue and expires April 2021. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
- Discuss the prevalence of osteoporosis, and the types and properties of drugs used to manage medication-related osteonecrosis of the jaw (MRONJ).
- Describe when MRONJ was first reported, the estimated incidence rate, and factors that contribute to this condition.
- Explain the oral anatomy most commonly affected, as well as clinical strategies for managing patients with MRONJ.
Osteoporosis can impact a patient’s quality of life due to the possibility of bone fractures. According to data from the National Health and Nutrition Examination Survey, the prevalence of osteoporosis in older U.S. adults ranges from 6% to 11%.1 Accordingly, antiresorptive medications — such as bisphosphonates and receptor activator of nuclear factor kappa-Β ligand (RANKL) inhibitors, which help in the management of osteoporosis — are commonly prescribed. These agents are also used to treat bone diseases, such as Paget’s disease, hyperparathyroidism and osteogenesis imperfecta, as well as primary bone malignancy or metastatic bone malignancy from various cancers.2 However, according to a survey by Tanna et al,3 while most dental practitioners were familiar with bisphosphonates, more than 90% were unaware of the other antiresorptive medications that can cause medication-related osteonecrosis of the jaw (MRONJ). Antiresorptive therapies for individuals with osteoporosis include five principal classes of agents: bisphosphonates, estrogens, selective estrogen receptor modulators, calcitonin, and monoclonal antibodies, such as denosumab. While each has the potential to cause osteonecrosis, bisphosphonates are the main focus of this article because they are the most commonly prescribed antiresorptive agents.4,5 As such, clinicians should be mindful of strategies that can help these patients maintain optimum oral health.
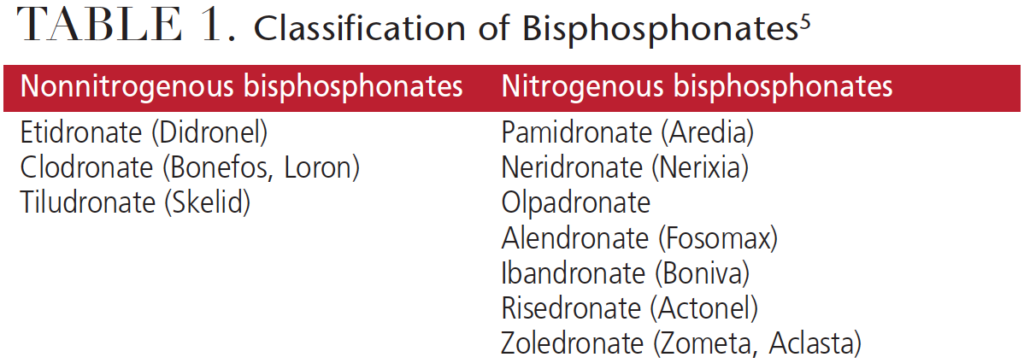
Chemically, bisphosphonates are analogs of pyrophosphates that bind selectively to bone minerals.4 Clinically, they have been shown to reduce bone pain and delay pathological skeletal events, including fractures.5 Differentiated by chemical structure, nonnitrogenous and nitrogenous bisphosphonates (Table 1) are deposited into the mineralized structures and lead to osteoclast death during resorption. Potency depends on the composition, with nitrogenous bisphosphonates being 10-fold to 100-fold more potent, and with a broader therapeutic window than nonnitrogenous bisphosphonates.6 Delivery can be oral or intravenous, although adverse effects on renal function have been reported when higher doses are infused intravenously.7
MECHANISM OF ACTION
Bisphosphonates inhibit osteoclastic bone resorption in a different fashion than other antiresorptive agents.8–10 They attach to hydroxyapatite binding sites on bony surfaces undergoing active resorption, where they impair the ability of the osteoclasts to form the ruffled border, adhere to the bony surface, and produce the protons necessary for continued bone resorption.8,9,11 They also reduce osteoclast activity by decreasing osteoclast progenitor development and recruitment, and by promoting osteoclast apoptosis.
The mechanism of RANKL inhibitors is to inhibit the osteoclastogenesis by interfering the binding of RANK on osteoclast precursors and RANKL from osteoblasts. Without activated osteoclasts, the metabolism of bone is affected.2
TERMINOLOGY
Of concern to the dental community are reports of bisphosphonate-related osteonecrosis of the jaw. However, it becomes confusing when multiple terms are used to refer to the same condition. Early reports mentioned a condition called “phossy jaw.”12 Subsequently, the terms osteonecrosis of the jaw, bisphosphonate-related osteonecrosis of the jaw (BRONJ), antiresorptive drug-related osteonecrosis of the jaw, and medication-related osteonecrosis of the jaw (MRONJ) were introduced; MRONJ replaced BRONJ in 2014 due to the growing number of osteonecrosis cases associated with other antiresorptive medications (Figure 1 and Figure 2).

Marx13 initially reported on MRONJ in 2003, and this research was followed by other clinical case reports that showed similar clinical patterns in patients who took bisphosphonates.12,14,15 These reports brought attention to the clinical outcome of atypical avascular jawbone necrosis. Initially, MRONJ was thought to be associated with the IV forms of nitrogen bisphosphonates; however, reports have since shown MRONJ is also associated with less potent oral bisphosphonates, though the incidence rate is reported to be low.6 The clinical presentation of MRONJ is similar to osteoradionecrosis of the jaw and osteomyelitis of the jaw.12,14,15 Retrospective studies and case reports have indicated the incidence rate of MRONJ to range from 0.8%% to 12.0%. It has mostly been found in the mandible, with fewer reports of occurrence in the maxilla or both jaws.5 In addition, research of various malignancies, such as multiple myeloma, breast cancer or prostate cancer, showed that subjects who were taking, or had taken, bisphosphonates had a higher incidence of MRONJ.16 A multicenter retrospective study by Abu-ID et al12 showed that MRONJ had 2% to 11% incidence in patients with multiple myeloma, 1% to 7% incidence in breast cancer patients, and 6% to 15% incidence in prostate cancer patients.
PATHOPHYSIOLOGY
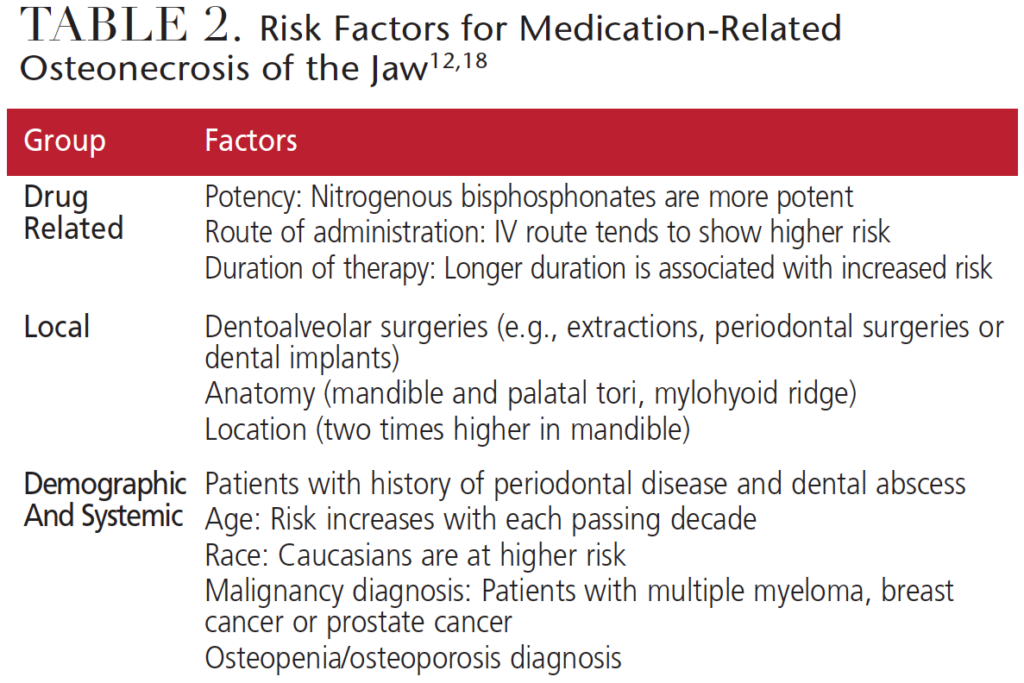
Mashiba et al17 proposed that through its antiresorptive properties, bisphosphonates inhibit natural bone remodeling, which eventually damages and reduces the mechanical properties of the bone. Marx et al6 indicated that local osteoporosis might lead to osteonecrosis of the jaw. Based on the literature, the American Association of Oral and Maxillofacial Surgeons (AAOMS) described risk factors that can lead to the development of MRONJ (Table 2).18 Other factors that might play a role in MRONJ include diabetes, smoking, alcohol use, poor oral hygiene and chemotherapeutic drugs.
STAGING AND TREATMENT
In defining the staging and treatment of MRONJ, the AAOMS task force classified patients into five categories,18 ranging from a patient presenting with no symptoms and needing no treatment interventions to individuals in stages 0, 1, 2 and 3. Various stages require different treatment strategies. For example, pain management and infection control are necessary for each stage, while surgical treatment is indicated for stages 2 and 3. Stage 3 will likely require surgical debridement, with possible resection of sites. However, studies have indicated that surgical procedures in stages 1 and 2 may help achieve optimal results.19,20
In addition, in 2014 Franco et al20 evaluated the outcomes of 266 MRONJ lesions using a new dimensional stage classification. Clinicians can also use this staging system to make treatment recommendation for patients presenting with MRONJ.
DISCONTINUATION OF BISPHOSPHONATES
The role of a “drug holiday” remains controversial. In 2009, the AAOMS recommended withholding oral bisphosphonates for up to three months before and after a surgical procedure.18 However, a recent study by Hasegawa et al21 did not support the effectiveness of a drug holiday on the outcome of MRONJ in patients taking oral bisphosphonates. For patient on IV bisphosphonates, short-term discontinuation might not allow for better outcomes, while long-term discontinuation might be beneficial in stabilizing established sites of MRONJ, reducing the risk of new site development, and reducing clinical symptoms.22 Based on the recommendation of McClung et al,23 the decision to discontinue antiresorptive medication relies on the patient’s fracture risk, T score and history of hip or spine fracture. Discussion with the patient’s physician regarding cessation of bisphosphonates is mandatory in MRONJ treatment.
MANAGEMENT STRATEGIES
It is important to establish and maintain good oral hygiene with regular dental visits for patients taking these drugs. Prior to starting bisphosphonate therapy, addressing existing dental issues is a best-practice strategy. Based on a study of 731 patients, Salgarello et al24 made the following recommendations:
- Finish all necessary dental procedures, such as tooth extractions, prior to bisphosphonate treatment, as extraction was the most frequent procedure associated with the development of MRONJ25
- Reevaluate oral and periodontal health every three to six months
- For patients already under bisphosphonate treatment, careful follow-up exams should be scheduled every three to six months.
- If dental surgery is performed, consider a drug holiday based on physician recommendations
In order to minimize surgical trauma:
- When possible, consider root canal treatment to save the tooth or teeth
- Reduce the level of inflammation in the surgical sites by completing anti-inflammatory treatment prior to dentoalveolar surgery
- If appropriate, consider atraumatic extraction using orthodontic elastics26 or careful elevation of the tooth
- Consider referring patients to surgical specialists with greater additional experience
- Prescribe an antibacterial rinse (e.g., chlorhexidine) prior to the procedure and during the postoperative phase
- Use antibiotics perioperatively18,27
DENTAL TREATMENT
Generally speaking, if routine dental treatment — such as prophylaxis, fluoride carriers, dental restorations or dentures — is indicated, no special precautions are required for these patients. However, if more invasive treatment is needed, such as extractions, periodontal surgery or surgical root canal treatment, use of bisphosphonates should be delayed for a month to allow sufficient time for bone recovery and healing.6
Restorative Dentistry: Because dental disease, such as caries leading to periapical infections and periodontitis, has been associated with bisphosphonate-related bone necrosis, patients taking these drugs should have a dental examination and address any dental conditions prior to starting the medication.28 Clinicians must be careful to avoid soft tissue trauma during restorative treatment. Additionally, removable prosthesis (e.g., partial or complete dentures) should be carefully inspected and adjusted to prevent soft tissue trauma.
Periodontal Treatment: The goal of periodontal therapy is to eliminate infection and to prevent the spread of infection to other areas of the oral cavity and body. Both periodontal disease and treatment pose a risk for MRONJ for patient taking bisphosphonates;6 therefore, when treating periodontal disease, clinicians should handle tissues carefully to minimize tissue trauma. Marx et al6 reported 11.2% of bisphosphonate-induced bone exposure was related to periodontal surgery. Bone necrosis after periodontal surgery and other surgical procedures might be due to the exposure of bone following flap replacement and a lack of normal healing of the bone and surrounding tissue due to low cellular proliferative capacity.29 Therefore, during periodontal surgery, primary closure of wounds should be attempted (when possible) to enhance tissue healing.

Orthodontic Therapy: Research into tooth movement in animals and humans using bisphosphonate medications reported no contraindications to orthodontic therapy.29 Although treatment for patients taking bisphosphonates is not contraindicated, clinicians should be cognizant and avoid potential soft tissue damage that can be caused by brackets and archwires.
Endodontics: No evidence has been reported to show an association between endodontic treatment and MRONJ in patients.30 It is recommended that nonsurgical endodontic treatment be rendered with the goal of avoiding soft tissue and periapical trauma.
Extractions/Dental Implants: Extractions and implants are considered as invasive osseous dental procedures that can trigger osteonecrosis of the jaw for patients taking bisphosphonates. These invasive procedures should be carefully planned; AAOMS recommendations include:2
For patients about to initiate bisphosphonate therapy:
- Only begin bisphosphonate therapy after optimum oral health is achieved.
- Nonrestorable teeth should be extracted at this time and other invasive procedures — including dental implants — should be done at this time.
- Bisphosphonate therapy can be initiated after optimum osseous healing is achieved. Maintenance of oral hygiene and follow-up are necessary.
For patients receiving bisphosphonate therapy:
- No strong evidence exists in support of, or as an alternative to, a drug holiday for patients taking bisphosphonates. The AAOMS recommends a two-month drug-free period to reduce bisphosphonate levels for an invasive procedure. This decision is made with the prescribing physician’s consult.
- When a patient is on oral bisphosphonates for less than four years and the clinical risk factors are at a minimum, extractions/dental implant procedure can be carried out, provided the patient is informed of the benefits and risks associated with the procedure. Informed consent is required.
- When a patient is on bisphosphonates for less than four years and is taking corticosteroids or anti-angiogenic medications, the prescribing doctor is contacted to consider a drug-holiday. Bisphosphonates can be restarted after optimum osseous healing is achieved. Corticosteroids or anti-angiogenic medications in combination with bisphosphonate therapy can increase the risk of MRONJ.
- When a patient is on bisphosphonates for more than four years, the prescribing physician should be contacted concerning a drug holiday. Bisphosphonates can be restarted after optimum osseous healing is achieved.
SUMMARY
Bisphosphonates are the most commonly prescribed antiresorptive agents1,2 and are first-line drugs for treating postmenopausal osteoporosis. Clinicians should be aware of the oral health effects associated with these medications, and use special care in treating these patients. When managing patients taking bisphosphonates or those presenting with signs of MRONJ, it is important to emphasize the need to maintain optimal oral hygiene and have regular follow-up care. When possible, and prior to starting these medications, addressing existing dental issues is a best-practice strategy.19 Finally, from a clinical perspective, it is incumbent on oral health professionals to be careful to avoid soft tissue trauma when performing dental treatment on this patient population.
CLINICAL CASE REPORT
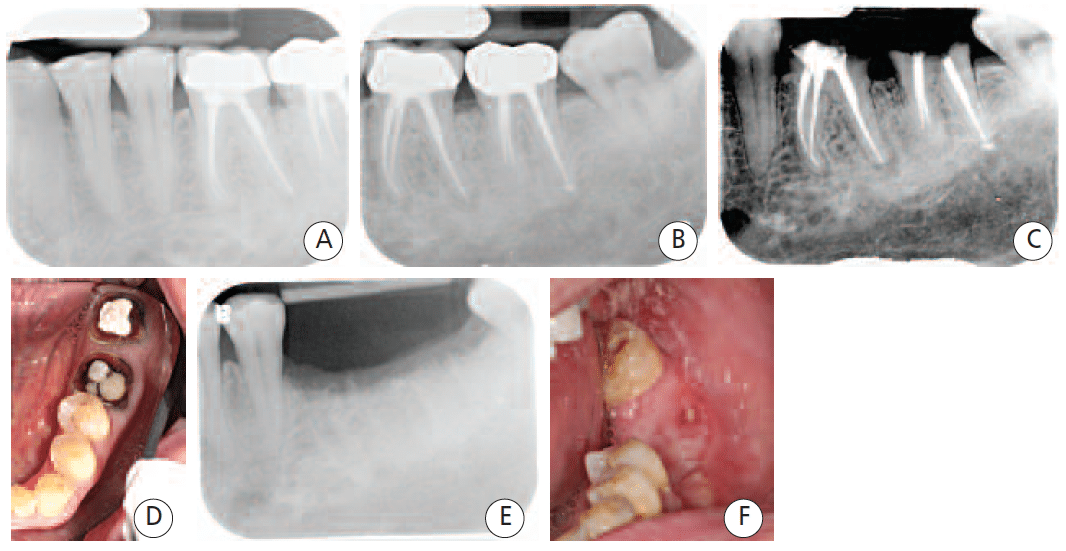
(Figures 3A through 3F): The patient was taking oral alendronate sodium (35 mg) once a week for osteoporosis. He presented to the dental clinic to replace the crowns on teeth #18 and #19. As the remaining tooth structure was inadequate, extraction and implant placement was suggested. Following surgical extraction, the socket was thoroughly debrided, grafted with freezedried bone allograft, and covered by a nonresorbable membrane and sutured. One month after surgery, the patient reported mild discomfort. Three months after surgery, the tissue healed well and without any bone exposure. The radiographic films showed bone fill on the extraction site. However, four months after surgery, a 4×1.5-mm asymptomatic area of exposed bone was found in the lower left quadrant. The patient was advised to stop taking bisphosphonate for at least three months to allow spontaneous tissue healing, and a medical consult form was sent to his physician addressing his medication. The patient was advised to clean this area with 0.12% chlorhexidine mouthrinse, but no antibiotic was prescribed. Six months after surgery, a 2×3-mm asymptomatic lesion still presented, and with no adjacent erythematic tissue. Two sessions of ozone therapy were provided, after which, healing proceeded uneventfully.
References
- Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA. Trends in osteoporosis and low bone mass in older US adults, 2005-2006 through 2013-2014. Osteoporo Int. 2017;28:1979–1988.
- Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw – 2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956.
- Tanna N, Steel C, Stagnell S, Bailey E. Awareness of medication related osteonecrosis of the jaws (MRONJ) amongst general dental practitioners. Br Dent J. 2017;222:121–125.
- Gutta R, Louis PJ. Bisphosphonates and osteonecrosis of the jaws: science and rationale. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:186–193.
- Siddiqi A, Payne AG, Zafar S. Bisphosphonate-induced osteonecrosis of the jaw: a medical enigma? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e1–e8.
- Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567–1575.
- Markowitz GS, Appel GB, Fine PL, et al. Collapsing focal segmental glomerulosclerosis following treatment with high-dose pamidronate. J Am Soc Nephrol. 2001;12:1164–1172.
- Rodan GA, Fleisch HA. Bisphosphonates: mechanisms of action. J Clin Invest. 1996;97:2692–2696.
- Sato M, Grasser W, Endo N, et al. Bisphosphonate action. Alendronate localization in rat bone and effects on osteoclast ultrastructure. J Clin Invest. 1991;88:2095–2105.
- Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev. 1998;19:80–100.
- Colucci S, Minielli V, Zambonin G, et al. Alendronate reduces adhesion of human osteoclast-like cells to bone and bone protein-coated surfaces. Calcif Tissue Int. 1998;63:230–235.
- Abu-Id MH, Warnke PH, Gottschalk J, et al. “Bis-phossy jaws” – high and low risk factors for bisphosphonate-induced osteonecrosis of the jaw. J Craniomaxillofac Surg. 2008;36:95–103.
- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–1117.
- Vieillard MH, Maes JM, Penel G, et al. Thirteen cases of jaw osteonecrosis in patients on bisphosphonate therapy. Joint Bone Spine. 2008;75:34–40.
- Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–534.
- Bamias A, Kastritis E, Bamia C, et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol. 2005;23:8580–8587.
- Mashiba T, Hirano T, Turner CH, Forwood MR, Johnston CC, Burr DB. Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res. 2000;15:613–620.
- Ruggiero SL, Dodson TB, Assael LA, et al. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws – 2009 update. J Oral Maxillofac Surg. 2009;67:2–12.
- Vescovi P, Manfredi M, Merigo E, Meleti M. Early surgical approach preferable to medical therapy for bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2008;66:831–832.
- Franco S, Miccoli S, Limongelli L, et al. New dimensional staging of bisphosphonate-related osteonecrosis of the jaw allowing a guided surgical treatment protocol: long-term follow-up of 266 lesions in neoplastic and osteoporotic patients from the University of Bari. Int J Dent. 2014;2014:935657.
- Hasegawa T, Kawakita A, Ueda N, et al. A multicenter retrospective study of the risk factors associated with medication-related osteonecrosis of the jaw after tooth extraction in patients receiving oral bisphosphonate therapy: can primary wound closure and a drug holiday really prevent MRONJ? Osteoporo Int. 2017;28:2465–2473.
- Ruggiero SL, Dodson TB, Landesberg R, Mehrotra B. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007;65:369-376.
- McClung M, Harris ST, Miller PD, et al. Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med. 2013;126:13–20.
- Salgarello S, Mensi M, Cella F, Stranieri F, Di Rosario F. BRONJ prevention: 9 years of clinical practice: Ann Stomatol (Roma). 2014;5(2 Suppl):39–40.
- Aljohani S, Fliefel R, Ihbe J, Kuhnisch J, Ehrenfeld M, Otto S. What is the effect of anti-resorptive drugs (ARDs) on the development of medication-related osteonecrosis of the jaw (MRONJ) in osteoporosis patients: A systematic review. J Craniomaxillofac Surg. 2017;45:1493–1502.
- Regev E, Lustmann J, Nashef R. Atraumatic teeth extraction in bisphosphonate-treated patients. J Oral Maxillofac Surg. 2008;66:1157–1161.
- Lodi G, Sardella A, Salis A, Demarosi F, Tarozzi M, Carrassi A. Tooth extraction in patients taking intravenous bisphosphonates: a preventive protocol and case series. J Oral Maxillofac Surg. 2010;68:107–110.
- Kos M. Association of dental and periodontal status with bisphosphonate-related osteonecrosis of the jaws. A retrospective case controlled study. Arch Med Sci. 2014;10:117–123.
- Consolaro A. The use of bisphosphonates does not contraindicate orthodontic and other types of treatment! Dental Press J Orthod. 2014;19:18–26.
- Moinzadeh AT, Shemesh H, Neirynck NA, Aubert C, Wesselink PR. Bisphosphonates and their clinical implications in endodontic therapy. Int Endod J. 2013;46:391–398.
Featured image COURTESY STEPHANIE STEELE, DDS
From Decisions in Dentistry. April 2018;4(4):45-48.