Digital Dentistry for Complete Dentures
A review of digital dentistry versus conventional approaches to complete dentures.
Complete edentulism is a debilitating condition that negatively affects a person’s well-being. Associated with a diminished quality of life and health challenges — including comorbidities, such as malnutrition and obesity — it affects professional opportunities, as well as social and personal relationships.1,2 Although the incidence of complete edentulism has decreased in recent decades, the growth and aging of the population is expected to increase the number of edentulous patients from 33.6 million in 2016 to 37.9 million in 2020.2 Digital dentistry and dental implants have revolutionized treatment for completely and partially edentulous patients, but not everyone is a candidate or can afford implants. As a high number of individuals affected by this condition are from a lower socioeconomic background, with limited access to care, cost effective and efficient treatment in the realm of complete edentulism is becoming increasingly necessary.3
There is a wide array of treatments for complete edentulism, and each option has its advantages and drawbacks. In a nutshell, treatment of the edentulous patient can be divided into fixed and removable prostheses. A fixed prosthesis, either cement- or screw-retained, involves four or more implants, while removable treatment consists of conventional complete dentures and overdentures supported by teeth, solitary implant attachments, or implant-supported bars. This article will focus on removable prostheses.
For close to a century, polymethyl methacrylate has been used in the fabrication of dentures. Polymerization is catalyzed by heat or chemical reaction and, over the years, numerous techniques have been developed. Recently, computer aided design/computer aided manufacturing (CAD/CAM) technology has been used to design and fabricate complete dentures. This article briefly covers advances in digital dentures.
Digital design and manufacturing was introduced to dentistry by Andersson, who developed the Procera system in 1983, and Mörmann, who introduced the CEREC system in 1985.4 Earlier CAD/CAM innovations were mostly geared toward indirect, tooth-borne restorations. The first report of CAD/CAM use for dentures is attributed to Maeda et al,5 who, in 1994, employed additive manufacturing technology.
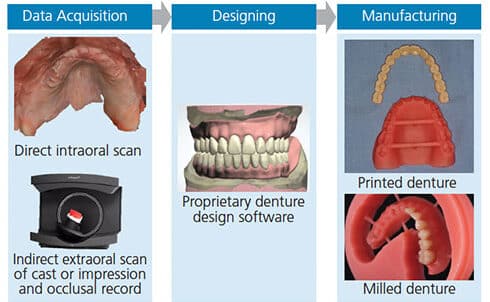
As seen in Figure 1, the three components of using CAD/CAM technology for digital dentures are:
- Data acquisition
- Prosthesis design
- Manufacturing
DATA ACQUISITION
With the conventional complete denture process, master casts are obtained by border molding a custom tray and using an elastomeric impression material. Similarly, in the CAD/CAM process, the initial step requires the acquisition of data. Two options are available: direct intraoral scanning, or making a conventional impression that can be scanned with a desktop scanner or poured in gypsum to obtain the master casts that, in turn, are scanned.
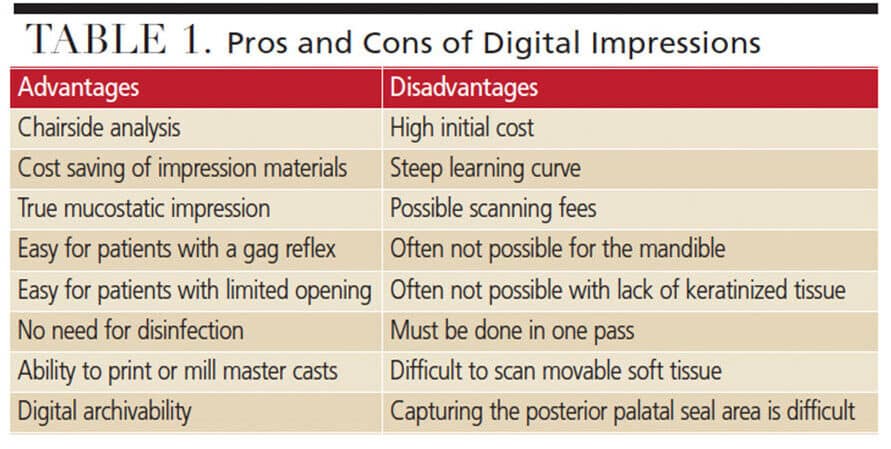
Advantages: In general, taking a digital impression has many advantages, including the possibility of performing an immediate chairside analysis (e.g., to evaluate the anatomy, residual ridges, presence of undercuts, or necessity of preprosthetic surgery). This approach saves on impression material, and can be quicker than a conventional impression (two minutes for the maxilla, and five minutes for the mandible when possible). In addition, it is convenient in cases involving patients with a gag reflex or limited opening. It is a true mucostatic impression; in addition, there is no need for disinfection, it has a faster turnaround time, and the data can be archived for future use without occupying physical space.6
Disadvantages: This technology has some challenges, such as the initial high cost, learning curve, and possible subscription fees for the equipment and software. Clinically, using an intraoral scanner for edentulous patients can be tricky. The posterior palatal seal in the maxilla and complicated floor of the mouth anatomy — with interference from the tongue and saliva in the mandible — can be difficult to capture. In cases with a limited amount of keratinized tissue, the mucosa is more movable and needs to be recorded in one pass since returning later over a missed area results in a different position of the soft tissue, leading to an error in the digital impression.6
Hence, it is advisable to make a conventional impression and scan the impression or master cast. Table 1 summarizes the advantages and disadvantages of scanning technology.
PROSTHESIS DESIGN
Denture-designing software offers a powerful tool that lets clinicians select molds from a library of teeth to generate the tooth arrangement automatically — although it is still possible to customize the tooth setup. It is the authors’ opinion that use of CAD technology for complete dentures can be a great teaching tool for students, as it can show them the proper positioning of the denture teeth in terms of esthetics, relationship to the residual ridge, location of the occlusal plane, and occlusal relationship.
MANUFACTURING TECHNOLOGIES
Since the introduction of polymethyl methacrylate by Wright in 1936, many issues of conventional complete denture materials have been associated with polymerization shrinkage, leading to issues of fit, strength, and also release of monomer.7,8 With CAD/CAM technology, two types of fabrication methods can be used to overcome these shortcomings.
Subtractive manufacturing (milling): In the subtractive approach, a puck (block) of material is milled by automated control of specialized cutting tools that receive information from a computer algorithm known as computer numerical control technology.
As the block of acrylic resin comes prepolymerized, there are no shrinkage issues. Also, as the puck is prepolymerized under high temperature and pressure, there may be less monomer release, which, in turn, reduces irritation to the soft tissues. The precision of milling is directly related to the milling unit’s number of axes and size of the burs. The reported precision is between 5 and 25 microns.9,10
Additive manufacturing (three-dimensional printing): In this method, material is stacked layer by layer, one over the other, to create a three-dimensional structure. Furthermore, additive manufacturing offers the ability to produce structures with complex geometries. It also reduces material waste by 40% and allows finer detail compared to subtractive technology9
Compared to conventional fabrication methods, delivering complete dentures with CAD/CAM technology requires fewer appointments (two to three visits), saving chairtime. This can be beneficial for older adults (Table 2).11,12 The two-visit procedure generally skips the try-in appointment — although the authors highly recommend this step. One advantage of a try-in prosthesis is that the patient can take it home for a few weeks to evaluate function and esthetics, which is not possible with traditional wax try-in setups.
The following case report demonstrates the use of this CAD/CAM technology wherein the surgical guide was used for the mandibular implant placement, and also served as a custom tray, record base, and artificial tooth arrangement guide.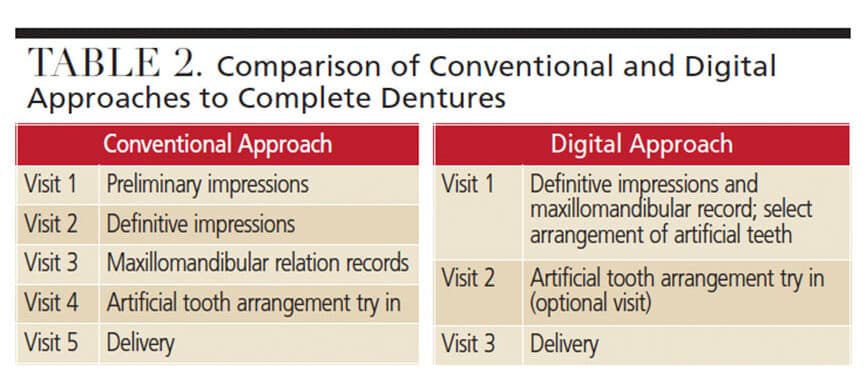
CASE REPORT
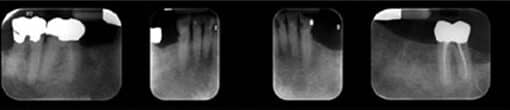
A 75-year-old male presented with a chief concern that his mandibular teeth were sensitive and breaking down (Figure 2). His medical history was unremarkable, although he complained of mild xerostomia. The patient had a maxillary complete denture that was recently made and that he was satisfied with. On the mandibular arch, the patient had a history of failing restorations, primary and secondary caries, and an ill-fitting mandibular removable partial denture. After a thorough discussion of his treatment options, the patient decided to receive a two-implant-retained overdenture.
Extraoral, intraoral, oral cancer screening and occlusal examinations were performed. Diagnostic casts were obtained, mounted and evaluated. An alginate impression was made of the maxillary prosthesis to serve as the opposing cast, and a vinyl polysiloxane (VPS) impression in a stock tray was made of the mandibular arch. Maxillomandibular relation records were obtained and an artificial tooth arrangement was set up for a mandibular immediate complete denture. Once the immediate denture was processed and finished, it was duplicated in clear acrylic resin to serve as a surgical/radiographic guide. All the mandibular teeth were extracted uneventfully under local anesthesia and the mandibular immediate denture delivered. After two months, the surgical/radiographic guide was placed on the mandibular arch, and a cone beam computed tomography (CBCT) scan was taken to plan the implant positions. Two implants were placed in sites #22 and 27 and buried for three months.
DEFINITIVE PROSTHESIS
With the immediate complete dentures, the patient’s existing occlusal vertical dimension (OVD) was evaluated using phonetics, facial profile and esthetics. It was recorded for future reference by measuring the distance between two marked reference points: one on the tip of the patient’s nose, and the other on the most anterior point of the chin. The healing abutments were removed and the gingival cuff height was measured to select the appropriate attachment system abutments, which were installed per the manufacturer’s recommendations (Figure 3).
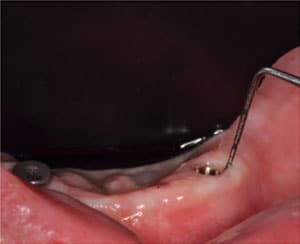
Next, abutment level impression copings were placed and the surgical guide seated and modified to provide at least 5 mm of clearance around the impression copings (Figure 4). The access openings in the surgical guide were covered with a light-polymerizing material (Figure 5).
The surgical guide was used as a custom tray and relieved appropriately on the intaglio surface and borders to ensure passive seating with 1 mm of space for the impression material. The OVD was reevaluated with the surgical guide based on the previously recorded measurements (Figure 6).
A VPS interocclusal material was used to record the maxillo-mandibular relationship. Tray adhesive was applied on the intaglio surface of the surgical guide, and the definitive impression was made using heavy body VPS around the impression copings and medium body VPS for all other areas. Once the tray was placed in the oral cavity, border molding movements were performed and the patient was asked to close down into the interocclusal record that was previously obtained. The OVD and centric relation were reverified and held steady until the impression material set (Figure 7).
The definitive abutment level impression that was made with the surgical guide, along with the interocclusal record and opposing cast, were sent to the laboratory, where the items were scanned. Instructions were given regarding the shade and midline. The mold characteristics could be identified from the intact denture teeth on the surgical guide. The occlusal scheme was specified for bilateral balanced occlusion. Denture designing software was used to design the teeth and denture base according to the work authorization, and a digitally designed preview file was sent to the clinician for approval. Once approved, the milling process was initiated and completed (Figure 8).

The mandibular overdenture (which was made using a monolithic dual-shaded block with the teeth and denture base together) was milled in one piece and returned finished. The prosthesis was tried in, adjustments were made for fit and comfort, and the occlusion was verified. As the master cast incorporated abutment analogues, the attachment housing could be picked up in the laboratory or returned to the clinician to perform an intraoral pickup procedure. Alternatively, the impression can be made without abutment level impression copings directly over the abutments provided there is sufficient clearance made for the impression material. In this situation, the primary author decided to perform an intraoral pickup of the housings and, as the recesses were already created by the CAM process, minimal modifications were done to the denture. Once the patient and clinician were satisfied with the prosthesis, the next step of connecting the denture to the implant abutments was performed, as per the manufacturer’s instructions (Figure 9). Next, home care instructions and follow-up appointments were made (Figure 10).
This clinical treatment highlights the versatile use of the surgical guide as a custom tray, record base, and denture tooth mold selection guide. This helps eliminate additional patient visits, reduces costs associated with additional laboratory procedures, and produces a high-quality prosthesis.

DISCUSSION
The use of CAD/CAM in digital dentistry remains an exciting topic with tremendous growth potential. However, challenges can be encountered, as well. With the subtractive method, denture teeth often need to be placed into the dedicated sockets, which can lead to deviations from planned arrangement, and the strength of the bond still needs to be assessed.13 These complications could be overcome by milling one-piece monolithic dentures, as shown in the above case report. Using additive or subtractive manufacturing, dentures can be fabricated with a combination of methods. These include fabricating a milled denture base or a printed denture base, with prefabricated denture teeth bonded into the sockets. However, denture teeth can also be milled or printed separately and bonded to a milled or printed denture base (Figure 11).
Milling technology has been used for a longer period and therefore is supported by more research, especially regarding material properties. Although additive manufacturing is fast catching up, clinicians need to be cautious when making choices regarding materials for printed dentures. In the near future, multi-material printing will become available that will allow clinicians to print monolithic dentures with different material properties within the same denture.14 This denture technology has many additional advantages, such as the ability to superimpose images from preoperative facial scans, digital photographs, smile design programs, or CBCT images. With advanced software features, these overlays can be toggled on or off, depending on what the dentist or technician would like to accomplish.
CONCLUSION
Digital denture technology has simplified the designing and manufacturing process for complete dentures, and produces better-adapted prostheses with superior material properties. However, as of today, this technology does not compensate for poor diagnosis or the inability to make adequate conventional impressions and establish proper jaw relation records.
KEY TAKEAWAYS
- The growth and aging of the population is expected to increase the number of edentulous patients from 33.6 million in 2016 to 37.9 million in 2020.2
- As such, cost effective and efficient treatment in the realm of complete edentulism is becoming increasingly necessary.3
- Compared to conventional fabrication methods, delivering complete dentures with computer aided design/computer aided manufacturing technology requires fewer appointments (two to three visits), saving chairtime.
- Digital denture technology has simplified the designing and manufacturing process for complete dentures, and produces better-adapted prostheses with superior material properties.
REFERENCES
- Slade GD, Akinkugbe AA, Sanders AE. Projections of U.S. edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93:959–965.
- Felton DA. Complete edentulism and comorbid diseases: an update. J Prosthodont. 2016;25:5–20.
- Lee DJ, Saponaro PC. Management of edentulous patients. Dent Clin North Am. 2019;6:249–261.
- Goodacre CJ, Garbacea A, Naylor WP, Daher T, Marchack CB, Lowry J. CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent. 2012;107:34–46.
- Maeda Y, Minoura M, Tsutsumi S, Okada M, Nokubi T. A CAD/CAM system for removable denture. Part I: fabrication of complete dentures. Int J Prosthodont. 1994;7:17–21.
- Goodacre BJ, Goodacre CJ, Baba NZ. Using intraoral scanning to capture complete denture Impressions, tooth positions, and centric relation records. Int J Prosthodont. 2018;31:377–381.
- Steinmassl PA, Wiedemair V, Huck C, et al. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin Oral Investig. 2017;21:1697–1705.
- Bidra AS, Taylor TD, Agar JR. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives. J Prosthet Dent. 2013;109:361–366.
- Alharbi N, Wismeijer D, Osman RB. Additive manufacturing techniques in prosthodontics: where do we currently stand? A critical review. Int J Prosthodont. 2017;30:474–484.
- Alghazzawi TF. Advancements in CAD/CAM technology: options for practical implementation. J Prosthodont Res. 2016;60:72–84.
- Janeva NM, Kovacevska G, Elencevski S, Panchevska S, Mijoska A, Lazarevska B. Advantages of CAD/CAM versus conventional complete dentures — a review. Open Access Maced J Med Sci. 2018;4:1498–1502.
- Kattadiyil MT, AlHelal A. An update on computer-engineered complete dentures: a systematic review on clinical outcomes. J Prosthet Dent. 2017;117:478–485.
- Wimmer T, Eichberger M, Lümkemann N, Stawarczyk B. Accuracy of digitally fabricated trial dentures. J Prosthet Dent. 2018;119:942–947.
- Stapleton C. Multimedia Printing: On the Horizon? Available at: https://www.aegisdentalnetwork.com/idt/2020/06/multimaterial-printing-on-the-horizon. Accessed July 27, 2020.
From Decisions in Dentistry. September 2020;6(8):12-14,16.