 SEB_RA/ISTOCK/GETTY IMAGES PLUS
SEB_RA/ISTOCK/GETTY IMAGES PLUS
Original Research: Antibiotic Prescribing Trends Among Dentists
Research into antibiotic scripts from dental providers shows declines in the rate of prescribing per patient encounter.
This course was published in the May 2021 issue and expires May 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain antibiotic prescribing trends in healthcare, particularly dentistry.
- Describe some of the effects associated with antibiotics, and concerns surrounding antibiotic use.
- Discuss dental indications for antibiotic prescriptions, and what dental teams can do to promote the responsible use of this class of drugs.
Antibiotics are used to treat infections caused by bacteria that attack the wall or coating of the microorganism, interfering with reproduction or blocking protein production.1
The U.S. Centers for Disease Control and Prevention (CDC) provides annual antibiotic prescription reports, which show that from 2011 to 2017 antibiotic prescriptions have decreased across the disciplines of primary care physicians, emergency medicine, dermatology, gynecology and the surgery specialties.2 In contrast, nationwide rates of prescribing by dentists, physician assistants and nurse practitioners have increased over that same time span. While scope of practice and the number of physician assistants3 and nurse practitioners4 have risen, there have been no large-scale structural changes in the role or number of dentists. Within this context, our research group conducted a trends analysis of the last decade to understand changes to the dental rate of prescribing per patient encounter. We also examined this trend in terms of the number of antibiotic pills prescribed.
Antibiotics make up the majority of medications prescribed by dentists.5 Additionally, previous research has shown that antibiotic prescription alone was the most frequent emergency department treatment that dental patients received.6 Additionally, during emergency department treatment, the most common dental diagnoses for all ages were unspecified disorders of the teeth and supporting structures (44%), periapical abscess without sinus involvement (21%), and caries (18%).6 Dental procedures — rather than antibiotics — are the recommended treatment for cases like these. The American Dental Association (ADA) has guidelines for antibiotic prescribing that recommend against using antibiotics for most pulpal and periapical conditions, and instead suggest the use of definitive dental treatment.7
One of the risks of high levels of antibiotic prescribing is that it causes disturbances to the body’s microbiomes, specifically, the gastrointestinal region.5 In one study, a single dose of clindamycin was given to mice and, after four weeks, there was an 87% loss of gut microbiome species.8 Antibiotic resistance has been a topic of special concern,9 as various pathogens are developing resistance to multiple types of antibiotics, while some are immune to all antibiotics, making them extremely difficult to treat. Although resistance develops via mutations, which are random events, any rise in antibiotic prescribing frequency increases the risk of these events.
According to the CDC, one-third of antibiotic prescriptions in hospitals involve potential prescribing problems, such as giving an antibiotic without proper testing or evaluation, prescribing an antibiotic when it is not needed, or giving an antibiotic for too long.10 The National Action Plan for Combating Antibiotic-Resistant Bacteria set a goal that all hospitals should have an antibiotic stewardship program to reduce inappropriate antibiotic prescriptions by 20% by 2020.8 Experts have warned the rate at which pathogens are growing resistant to antibiotics is bringing us close to a post-antibiotic world.11 In 2016, a woman in Nevada died of an infection that could fend off every antibiotic (26 different drugs) available in the U.S.12 Prior to the introduction of antibiotics, many deaths resulted from bacterial infections,13 and a transition to a post-antibiotic world has the potential of regressing us back to this reality. Experts predict that by 2050 approximately 10 million people a year will die of antibiotic-resistant infections.14
Research suggests that while most healthcare prescribers are reducing their antibiotic scripts, the oral healthcare profession has not cut back to the same extent as other disciplines.2 To gain further understanding of trends in dental antibiotic scripts, our research group studied antibiotic prescribing from 2013 to 2020 using data from the University of Michigan School of Dentistry’s (UMSOD) electronic health record system Axium.
METHODS
Paper prescriptions were completely phased out at UMSOD on December 31, 2012, and our study period began January 1, 2013. We extracted data on antibiotic prescribing for the period spanning 2013 to 2020. Our team studied the trend of the quotient of unique antibiotic prescriptions and unique patient encounters over the study period, as well as trends in the number of antibiotic pills prescribed.
Simple descriptive data is used to describe the dataset. Since this was a quality assurance project of aggregate data, there was no informed consent required, and no patient identifying information was studied. The Committee on Human Subjects research evaluated the research proposal and deemed this study as IRB exempt (HUM00177280).
RESULTS
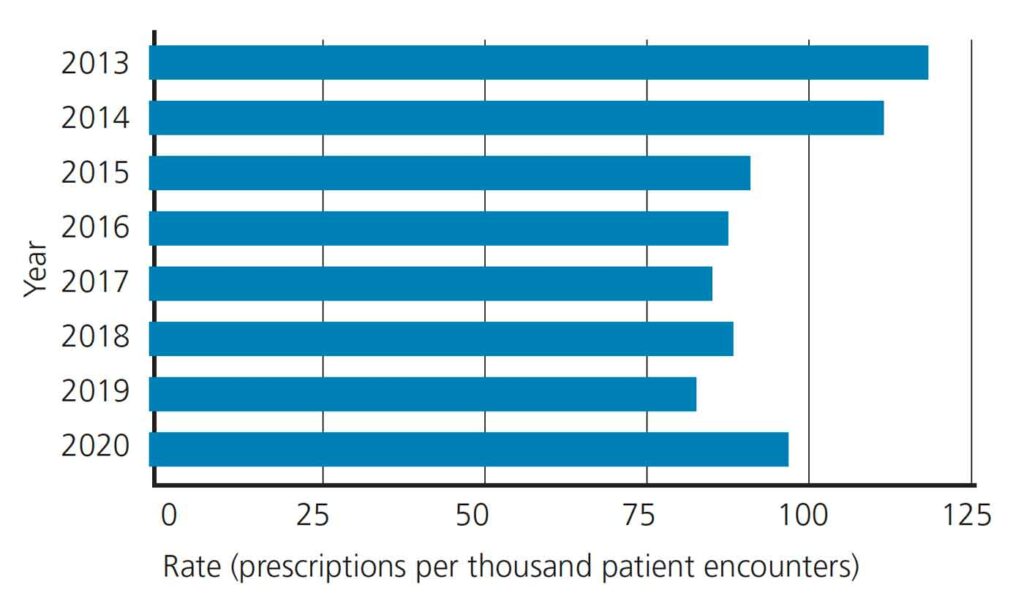
We summed the total number of dentist-only antibiotic prescriptions and patient visits per year at UMSOD, and calculated the rate of antibiotic prescription per patient encounter. In general, there has been a downward trend from 2013 to 2019, as shown in Figure 1, but the rate of antibiotics per patient encounter increased in 2020 during the COVID-19 pandemic. In 2013, there were 119.7 antibiotic prescriptions per thousand patient encounters, which was reduced to 84 prescriptions per thousand patient encounters by 2019. In 2020, there were 98.8 prescriptions per thousand patient encounters, which represents a 17.69% increase from 2019. While the rate still remains lower than in 2013 (119.7) and 2014 (113.5), it was higher than during other years in the study period.
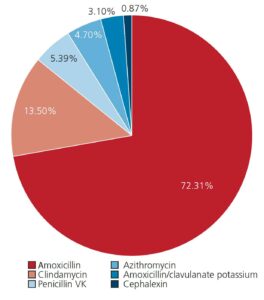
As Figure 2 shows, our research into prescribing patterns at UMSOD reveals that amoxicillin was the most common antibiotic prescription in 2020, accounting for 72.31% of all antibiotic scripts. The average number of amoxicillin pills prescribed was 23. This trend has persisted since 2013, as the average number of pills has ranged from 20 to 23 over the study period. In 2020, clindamycin was the second most common antibiotic agent, followed by penicillin VK.
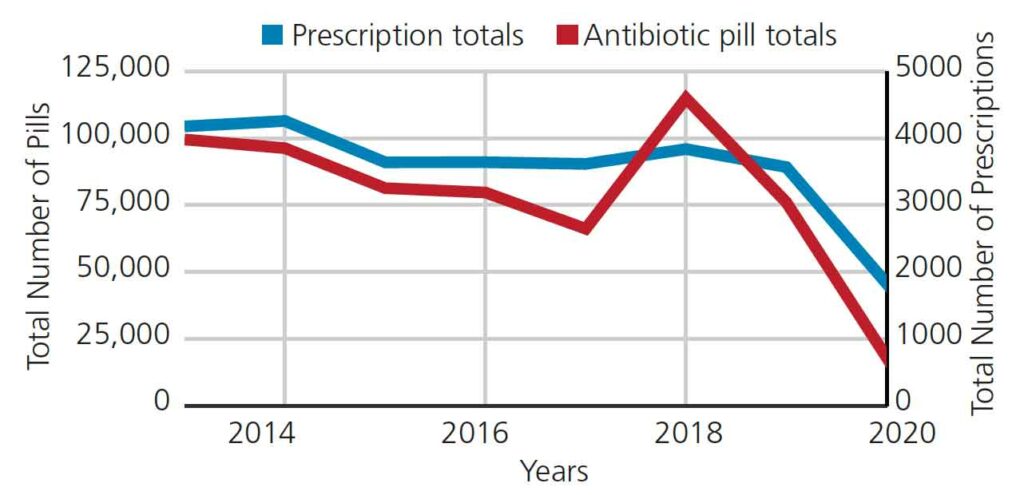
Figure 3 shows the trend in the number of antibiotic pills prescribed (left X-axis) and number of antibiotic prescriptions (right X-axis) from 2013 to 2020 at UMSOD. Both trend lines show a steady number of prescriptions and pills until the pandemic began in 2020.
DISCUSSION
In dentistry, there are few indications for the use of systemic antibiotics because a majority of oral conditions can be managed with operative interventions and oral hygiene procedures.5 The ADA recommends antibiotics in patients with systemic involvement (e.g., malaise or fever) due to dental conditions when the risk of systemic involvement is high or when a patient may lack immediate access to care.15 In 2020, the National Dental Practice-Based Research Network concluded that indications for antibiotic prophylaxis use are a frequent clinical issue encountered by dentists.16 Another survey of dentists found that 70% reported inappropriate prescription of prophylactic antibiotics prior to dental procedures.17 Our study revealed that in 2013 there were 119.7 dentist-only antibiotic prescriptions per thousand patient encounters at UMSOD, which was higher than the national norm for all dentists (prescribing rate of 77.5 prescriptions per thousand encounters).18 It is possible this academic dental center saw a larger proportion of complex infections and individuals with comorbidities than an average dental office.
Previous research has shown that antibiotic prophylaxis was prescribed in more than 168,000 dental visits from 2011 to 2015, and that 90% of these visits would only require antibiotic prescriptions in the case of cardiac patients who are considered at high risk for secondary infections.19 A 2013 study on dentists’ antibiotic prescribing patterns in the U.S. observed that in the Midwest region, general dentists prescribed antibiotics at a rate of 22.1% and 80.3 antibiotic prescriptions per thousand patient encounters.18 In 2014, the CDC stated that among healthcare providers, general dentists prescribed about 9% of all antibiotic prescriptions (approximately 24.9 million prescriptions).20 Our institutional data show a small decrease in dentist antibiotic prescribing at UMSOD from 2013 to 2014 — from 119.7 to 113.5 antibiotic prescriptions per thousand patient encounters, respectively.
During the study period, amoxicillin was the most commonly prescribed antibiotic at UMSOD, and clindamycin came in second. A 2013 study found the most commonly prescribed antibiotic agent was amoxicillin, with clindamycin coming in second, representing 56% and 14.4% of all antibiotic scripts, respectively.18 Dentists seem to be the highest prescribers of clindamycin, despite the relationship between clindamycin and Clostridium difficile, a potentially life-threatening condition.8,21 Researchers at the University of Minnesota reported that between 2009 and 2015, 15% of patients were diagnosed with C. difficile infections and had received an antibiotic prescription from their dentist prior to developing the infection, and at least half of those prescriptions were for clindamycin.22
In 2015, trends in antibiotic prescriptions at UMSOD showed a dramatic decrease compared to 2014, when there were 113.5 antibiotic prescriptions per thousand patient encounters. In 2015, that dropped to 92.3 per thousand patient encounters. Multiple factors could have influenced this trend. In 2015, the White House hosted the Forum on Antibiotic Stewardship, which resulted in more than 100 organizations (including the ADA)23 committing to reducing antibiotic prescribing over the next five years.24 In October 2015, UMSOD hosted a continuing education program for its faculty and clinical staff about antibiotic prescribing. In 2015, the ADA updated its clinical guidelines, stating that prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection in patients with prosthetic joint implants.25 One study assessed the effect on prescribing following provider education and use of a prescribing tool. The researchers found a substantial reduction (44.6%) in the number of inappropriate antibiotics prescriptions after the intervention, plus a 40.5% decrease in the total number of antibiotics.26
Complementary and alternative medicine (CAM), as described by Baars et al,27 focuses more on health promotion strategies, whereas conventional medicine focuses primarily on fighting disease. Based on lifestyle and medical changes and interactions, the CAM approach includes use of probiotics, changes in diet, and meditation. The study shows that doctors who implement both CAM and conventional strategies have much lower antibiotic prescribing rates than doctors who solely focus on conventional strategies.27
EFFECTS OF COVID-19
Since the COVID-19 pandemic began, the data show an increase from recent years in antibiotic prescriptions at UMSOD (98.8 prescriptions per thousand patient encounters in 2020). Similar trends were reported in England.28 The CDC released interim guidelines for patients who tested positive for COVID-19 and needed immediate dental care; it suggested that analgesics and antibiotics were the first line of treatment for these patients.29 Despite low bacterial and fungal coinfection rates for patients with COVID-19, clinical evidence suggests antibiotic prescribing remains high.30 A study reported that 72% of COVID-19 patients received antibiotics, even when not clinically indicated.31 More than 2.8 million antibiotic-resistant infections occur in the U.S. each year, and more than 35,000 people die.32 Reduced prescribing by dentists will help prevent the development of antibiotic resistance, which has the potential to worsen under the COVID-19 pandemic.31 Variations in antibiotic use by dentists may not be due to a lack of knowledge; rather, they may be explained by variations in dental training and implementation of various guidelines globally.33
CONCLUSION
Though our research showed a general downward trend in antibiotic prescribing from 2013 to 2019 at UMSOD, with restricted access to dental care due to COVID-19, there was an increase in antibiotic scripts in 2020. At the point we enter the post-pandemic era, dentists need to readjust and again pursue cautious antibiotic prescribing to reduce the risk posed by antimicrobial resistance.
There are no formal antimicrobial stewardship programs across the dental profession. The ADA, state dental societies, and both large and small practices should consider developing prescribing principles applicable across all dental disciplines. Furthermore, as part of patient education efforts, the entire dental team should present a consistent message about the appropriate use of antibiotics. The ultimate responsibility, of course, falls on the dentist, as every prescription should have clinical justification.
REFERENCES
- Healthline. How Do Antibiotics Work? Available at: https://www.healthline.com/health/how-do-antibiotics-work. Accessed March 27, 2021.
- U.S. Centers for Disease Control and Prevention. Outpatient Antibiotic Prescriptions — United States, 2017. Available at: https://www.cdc.gov/antibiotic-use/community/programs-measurement/state-local-activities/outpatient-antibiotic-prescriptions-US-2017.html. Accessed March 27, 2021.
- Finnegan J. Physician Assistant Workforce Is on the Rise Along With an Increase in Salaries. Available at: https://www.fiercehealthcare.com/practices/physician-assistants-one-fastest-growing-professions-healthcare-as-numbers-and-salaries. Accessed March 27, 2021.
- Clarke M. The Number of Nurse Practitioners Is on the Rise. Available at: https://www.healthleadersmedia.com/nursing/number-nurse-practitioners-rise. Accessed March 27, 2021.
- Dar-Odeh NS, Abu-Hammad OA, Al-Omiri MK, Khraisat AS, Shehabi AA. Antibiotic prescribing practices by dentists: a review. Ther Clin Risk Manag. 2010;6:301–306.
- Roberts RM, Hersh AL, Shapiro DJ, Fleming-Dutra KE, Hicks LA. Antibiotic prescriptions associated with dental-related emergency department visits. Ann Emerg Med. 2019;74:45–49.
- American Dental Association. Antibiotic Use for the Urgent Management of Dental Pain and Intra-oral Swelling Clinical Practice Guideline. Available at: https://ebd.ada.org/en/evidence/guidelines/antibiotics-for-dental-pain-and-swelling?utm_source=google. Accessed March 27, 2021.
- Buffie CG, Jarchum I, Equinda M, et al. Profound alterations of intestinal microbiota following a single dose of clindamycin results in sustained susceptibility to Clostridium difficile-induced colitis. Infect Immun. 2012;80:62–73.
- Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40:277–283.
- U.S. Centers for Disease Control and Prevention. Antibiotic Use in the United States, 2017: Progress and Opportunities. Available at: https://www.cdc.gov/antibiotic-use/stewardship-report/2017.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fantibiotic-use%2Fstewardship-report%2Fhospital.html. Accessed March 27, 2021.
- Johnson SR. ‘Post-Antibiotics’ World Is Here, Experts Say. Available at: https://www.modernhealthcare.com/safety-quality/post-antibiotics-world-here-experts-say. Accessed March 27, 2021.
- Minor L. Welcome To the Post-Antibiotic Era. Will We Save Ourselves in Time? Available at: https://scopeblog.stanford.edu/2019/12/06/welcome-to-the-post-antibiotic-era-will-we-save-ourselves-in-time/. Accessed March 27, 2021.
- Adedeji WA. The treasure called antibiotics. Ann Ib Postgrad Med. 2016;14:56–57.
- Cumper C. The Antibiotic Resistance Crisis. Available at: https://www.criver.com/eureka/the-antibiotic-resistance-crisis. Accessed March 27, 2021.
- Lockhart PB, Tampi MP, Abt E, et al. Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling: a report from the American Dental Association. J Am Dent Assoc. 2019;150:906–921.
- Lockhart PB, Thornhill MH, Zhao J, et al. Prophylactic antibiotic prescribing in dental practice: findings from a National Dental Practice-Based Research Network questionnaire. J Am Dent Assoc. 2020;151:770–781.
- Durkin MJ, Hsueh K, Sallah YH, et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc. 2017;148:878–886.
- Roberts RM, Bartoces M, Thompson SE, Hicks LA. Antibiotic prescribing by general dentists in the United States, 2013. J Am Dent Assoc. 2017;148:172–178.
- Dall C. Study Finds 81% of Dental Antibiotics Prescribing Not Needed. Available at: https://www.cidrap.umn.edu/news-perspective/2019/05/study-finds-81-dental-antibiotic-prescribing-not-needed. Accessed March 27, 2021.
- U.S. Centers for Disease Control and Prevention. Antibiotic Stewardship. Available at: https://www.cdc.gov/oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html. Accessed March 27, 2021.
- Bombassaro AM, Wetmore SJ, John MA. Clostridium difficile colitis following antibiotic prophylaxis for dental procedures. J Can Dent Assoc. 2001;67:20–22.
- Perry S. 80 Percent of Antibiotics Prescribed by Dentists Are Unnecessary, Study Finds. Available at: https://www.minnpost.com/second-opinion/2019/06/80-percent-of-antibiotics-prescribed-by-dentists-are-unnecessary-study-finds/. Accessed March 27, 2021.
- Fluent MT, Jacobsen PL, Hicks LA. Considerations for responsible antibiotic use in dentistry. J Am Dent Assoc. 2016;147:683–686.
- U.S. Centers for Disease Control and Prevention. U.S. Action to Combat Antibiotic Resistance. Available at: https://www.cdc.gov/drugresistance/us-activities.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdrugresistance%2Ffederal-engagement-in-ar%2Findex.html. Accessed March 27, 2021.
- American Dental Association. Oral Health Topics. Antibiotic Prophylaxis Prior to Dental Procedures. Available at: https://www.ada.org/en/member-center/oral-health-topics/antibiotic-prophylaxis. Accessed March 27, 2021.
- Teoh L, Stewart K, Marino RJ, McCullough MJ. Improvement of dental prescribing practices using education and a prescribing tool: a pilot intervention study. Br J Clin Pharma. 2020;87:152–162.
- Baars EW, Zoen EB, Breitkreuz T, et al. The contribution of complementary and alternative medicine to reduce antibiotic use: a narrative review of health concepts, prevention, and treatment strategies. Evid Based Complement Alternat Med. 2019;2019:5365608.
- Shah S, Wordley V, Thompson W. How did COVID-19 impact on dental antibiotic prescribing across England? Br Dent J. 2020;229:601–604.
- U.S. Centers for Disease Control and Prevention. Guidance for Dental Settings. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html. Accessed March 27, 2021.
- Nori P, Cowman K, Chen V, et al. Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect Control Hosp Epidemiol. 2020;42:84–88.
- Strathdee SA, Davies SC, Marcelin JR. Confronting antimicrobial resistance beyond the COVID-19 pandemic and the 2020 U.S. election. Lancet. 2020;396:1050–1053.
- U.S. Centers for Disease Control and Prevention. Biggest Threats and Data. Available at: https://www.cdc.gov/drugresistance/biggest-threats.html. Accessed March 27, 2021.
- Stein K, Farmer J, Singhal S, et al. The use and misuse of antibiotics in dentistry: a scoping review. J Am Dent Assoc. 2018;149:869–884.
From Decisions in Dentistry. May 2021;7(5)26-28,31.




