BRUNORBS/ISTOCK/GETTY IMAGES PLUS
BRUNORBS/ISTOCK/GETTY IMAGES PLUS
Alternative Method for Occlusal Guard Fabrication
This direct, intraoral method of occlusal guard fabrication eliminates the use of impressions or commercial laboratory involvement
Occlusal guards, also commonly referred to as splints, have been used for years in a variety of dental applications. They have been used to stabilize the maxilla or mandible after trauma or surgery, and are one of many modalities utilized in treating temporomandibular disorders (TMD). These appliances have also been used to control the adverse effects of bruxism. The Glossary of Prosthodontic Terms defines bruxism as: “1. The parafunctional grinding of teeth; 2. an oral habit consisting of involuntary rhythmic or spasmodic nonfunctional gnashing, grinding, or clenching of teeth, in other than chewing movements of the mandible, which may lead to occlusal trauma.”1 Stedman’s Medical Dictionary 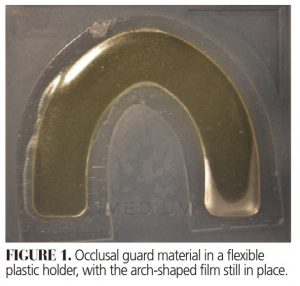 further states, “Grinding the teeth during sleep is a pathologic condition.”2 Nocturnal bruxing can lead to a host of oral health conditions, including excessive tooth wear, fractured teeth and/or restorations, temporomandibular joint soreness, localized muscle soreness, and headaches. This article will describe a method of creating an occlusal guard intraorally, without use of impressions or commercial laboratory fabrication.
further states, “Grinding the teeth during sleep is a pathologic condition.”2 Nocturnal bruxing can lead to a host of oral health conditions, including excessive tooth wear, fractured teeth and/or restorations, temporomandibular joint soreness, localized muscle soreness, and headaches. This article will describe a method of creating an occlusal guard intraorally, without use of impressions or commercial laboratory fabrication.
Clinicians can choose from a variety of occlusal guard designs based on the goals and philosophies of treatment. Variations include flat plane splints, anterior repositioning splints, anterior bite planes, posterior bite planes, pivot appliances, Lucia jigs, hydrostatic appliances, and the mandibular orthopedic repositioning appliance. They can be fabricated out of soft or hard acrylic, and some may include a soft vinyl liner.
The use of occlusal guards is effective in preventing destructive wear patterns associated with nocturnal bruxism. Although the occlusal guard does not prevent the patient from grinding, the acrylic serves to absorb the destructive forces rather than the enamel.1 Occlusal guards are often effective in controlling muscle and joint soreness associated with bruxing. This is due to decreased loading of the joint itself, as well as reduced muscular contractive forces. Splints protect muscles and the joint by ensuring that centric relation (CR) equals maximum intercuspation. This will help position the condyle in the most superior anterior position with minimal load, and reduce the occurrence of muscle engrams. The flat occlusal surface of an occlusal guard offers less resistance than the occlusal surfaces of teeth — essentially making this a much less efficient chewing appliance — which is the goal. Okeson’s3 text mentions at least eight considerations as to why occlusal guards are effective in treating symptoms associated with TMD.

DAYTIME INDICATIONS
Commonly known as night guards, occlusal guards are often used to control the harmful effects of daytime clenching. The destructive effects of daytime clenching frequently manifest as muscle or joint soreness. Patients will tend to subconsciously clench during waking hours, often while focused on other tasks. With an occlusal guard, patients will have less tendency to brux or grind significantly, as the proprioceptive receptors in the teeth and periodontal ligaments will exert a protective response. The occlusal guard serves two functions in these cases. While the teeth need less protection than the muscles and joint in these situations, the isometric contraction of the muscles can cause significant muscle soreness, headaches and joint pain. Compared to natural teeth, the occlusal guard will allow less contractive force against the occlusal guard itself. More importantly, the occlusal guard acts much like the habit-breaker appliances used in pediatric dentistry. Once the patient clenches against the smooth surface of the occlusal guard, instead of a comfortable maximum intercuspation, the subconscious habit now becomes conscious. It helps remind the patient there should always be space between the teeth while at rest.
The treatment of TMD is complicated by a wide range of opinions and philosophies — and these discussions are well beyond the scope of this paper. That noted, the method of controlling symptoms associated with TMD by using a flat-plane splint falls well within the philosophy espousing conservative, reversible treatment. A systematic review published in the Journal of the American Dental Association supports the use of occlusal guard therapy as effective in reducing pain associated with TMD.4 In these cases, the occlusal guards are more commonly referred to occlusal orthotic devices.
ALTERNATIVE FABRICATION METHOD
While fabrication of an occlusal guard will depend on the specific type of guard being made, it often must include maxillary and mandibular casts, a CR record, and perhaps a facebow transfer. Fabrication can be accomplished in-office or by a dental laboratory. Many clinicians opt for commercial laboratory fabrication. Upon return from the lab, the occlusal guard is tried intraorally and adjusted for fit, which allows the clinician to refine the occlusal scheme. This can also be accomplished in-office via the technique described here. Following occlusal guard fabrication and adjustment, the patient is given instructions on how often to wear the appliance, as well as home care instructions, and scheduled for follow-up appointments, as needed.
As previously stated, this article will describe a method of creating an occlusal guard intraorally. This direct intraoral technique involves a moldable sheet of resin that is utilized intraorally without the need for impressions or commercial laboratory fabrication. Once adapted to the teeth, it is tack cured intraorally and bench cured following removal from the mouth. The technique is as follows.
![occlusal figure]() Remove the resin occlusal guard material from the packaging, leaving the flexible film covering the material (Figure 1).
Remove the resin occlusal guard material from the packaging, leaving the flexible film covering the material (Figure 1).- Place the wafer of resin over the teeth with finger pressure (Figure 2).
- Wrap the resin onto the buccal and lingual surfaces of the teeth with finger pressure, engaging the interproximal areas and extending the material as far gingivally as possible.
- Have the patient occlude lightly into the resin, and, if possible, into the lateral excursions.
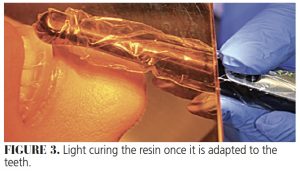
- Light cure the resin on the facial, occlusal and lingual aspects for at least 60 seconds each (Figure 3).
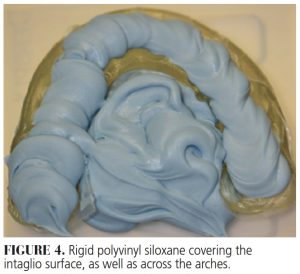
- Carefully remove the occlusal guard and fill the intaglio surface with a rigid polyvinyl siloxane (PVS) material. Although clinicians are advised to fill only the intaglio surface, the material can also be extruded from one side of the arch to the other for added cross-arch stabilization to prevent shrinkage during curing (Figure 4).
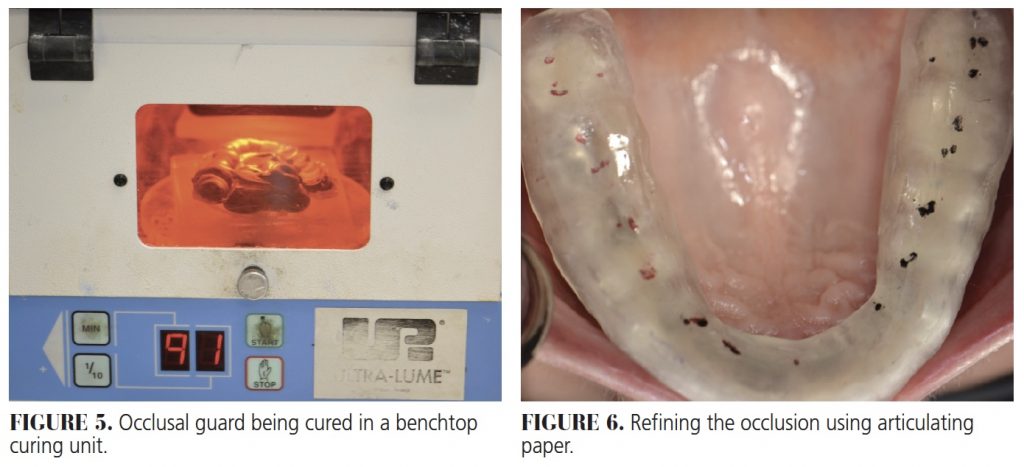
- The occlusal guard can be cured in a benchtop curing unit. Curing time varies according to the specific unit, but can vary between 10 and 20 minutes (Figure 5).
- Remove the occlusal guard from the curing unit and the PVS from the intaglio surface. Start the initial adjustment extraorally with an acrylic bur, removing all of the indentations on the occlusal surface and leaving a small occlusal contact for each opposing tooth.
- Try the occlusal guard in the mouth. Adjustments to the intaglio surface are usually minimal, but some adjustment may be needed if there is a large amount of material expressed into the interdental areas or moderate undercuts.
- Refine the occlusion using articulating paper (Figure 6).
- Polish extraorally (Figure 7).
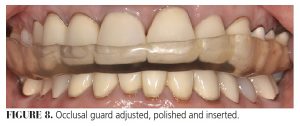
- Give the patient the occlusal guard with home care instructions and schedule routine follow-up appointments (Figure 8).
![occlusal figure]() DISCUSSION
DISCUSSION
Advantages — This technique has a number of advantages over conventional laboratory fabrication. It eliminates many of the steps involved with most other techniques, including the need for maxillary and mandibular impressions, casts and intraoral records. It also eliminates involvement with a commercial laboratory, saving considerable time and expense. The patient is able to leave with the appliance the same day, which allows the patient to start wearing it immediately for quicker resolution of symptoms.
 Another advantage of this technique is ease of repair. If a piece fractures off, or if the occlusal guard was thinned through overaggressive occlusal adjustment, material can simply be added to the roughened surface, light cured intraorally, and bench cured as was done initially.
Another advantage of this technique is ease of repair. If a piece fractures off, or if the occlusal guard was thinned through overaggressive occlusal adjustment, material can simply be added to the roughened surface, light cured intraorally, and bench cured as was done initially.
Disadvantages — This technique is not without challenges. The most important disadvantage is the inability to obtain a CR record using a leaf gauge and identifying areas of centric occlusion interference. This provides a challenge to developing a mutually protected occlusal scheme. The use of bimanual manipulation to find CR is therefore critical, and the occlusal scheme has to be developed in the cured splint material. Care must also be taken not to engage large undercuts in the existing dentition. It can be challenging to develop much of an excursive occlusion in the soft resin prior to curing, as the material can easily displace or distort. Care must be taken so the patient does not occlude too heavily into the uncured resin.
There is also lost time waiting for the material to cure in the benchtop unit. Additional time is needed to accomplish the initial occlusal adjustment extraorally to flatten the indentations. Accuracy in the initial occlusal registration will save chairtime as the final occlusal adjustments are made.
![occlusal figure]() CLINICAL TIPS
CLINICAL TIPS
This technique can be used to fabricate either a maxillary or mandibular occlusal guard. Mandibular occlusal guards can provide a challenge if the teeth have a significant lingual inclination. Whereas this could be blocked out on a working cast, that option is not feasible with the direct method.
It helps if the practitioner lubricates his or her fingers when adapting the material to the teeth in Step 2. In addition, it helps lubricate the opposing teeth and any teeth the occlusal guard will cover that have existing composite restorations to prevent inadvertent bonding.
The opposing occlusion is best registered with just the tips of the opposing cusps into resin, using the best bimanual manipulation method to get into CR (if possible).
CONCLUSION
Occlusal guards are an effective way to control the effects of bruxism, as well as many symptoms associated with TMD. This treatment is conservative, reversible, and, while not 100% effective, it remains effective enough to be considered when evaluating a patient presenting with these issues. This treatment clearly aligns with recommendations published in the Journal of the American College of Dentists that discuss the ethical considerations for treating TMD patients and promote reversible techniques that are effective in most cases.5
This article describes one approach to same-day intraoral fabrication of an occlusal guard. The technique is relatively simple, saves time and money, and the occlusal guard is ready for use the same day the patient presents for evaluation.
Key Takeaways
- Whether fabricated out of soft or hard acrylic, occlusal guards are available in a variety of designs based on the goals and philosophies of treatment.
- This article describes a method of creating an occlusal guard intraorally, without the use of impressions or commercial laboratory fabrication.
- Clinically efficient, this approach eliminates many of the steps involved with most other techniques — including the need for casts and intraoral records — saving practitioners and patients time and expense.
- Besides ease of repair, one of the chief benefits of this approach is that clinicians can deliver the appliance the same day, which allows the patient to start wearing it immediately for quicker resolution of symptoms.
References
- The Glossary of Prosthodontic Terms. Ninth Edition. Available at: https://www.academyofprosthodontics.org/_Library/ap_articles_download/GPT9.pdf. Accessed October 12, 2020.
- Stedmans’s Medical Dictionary. 22nd ed. Baltimore: Williams and Wilkins Co; 1974:181.
- Okeson JP. Management of Temporomandibular Disorders and Occlusion. 7th ed. St. Louis: Elsevier Mosby; 2013:395–396.
- Ebrahim S, Montoya L, Busse JW, Carrasco-Labra A, Guyatt GH. The effectiveness of splint therapy in patients with temporomandibular disorders, a systematic review and meta-analysis. J Am Dent Assoc. 2012;143:847–857.
- Brown RS, Greene CS. Ethical considerations in the management of temporomandibular disorders. J Am Coll Dentists. 2017;84:28–35.
From Decisions in Dentistry. November 2020;6(10):14-16.