
Sequential Management of Complex Restorative Erosion
This case report demonstrates the use of a bonded functional esthetic prototype in a patient with generalized-severe erosion as a diagnostic aid to increase the vertical dimension of occlusion and preserve tooth structure prior to full mouth rehabilitation.
Gastroesophageal reflux disease (GERD) causes severe dental erosion. The pathognomonic signs include erosion of palatal/occlusal surfaces of maxillary teeth and occlusal/ buccal surfaces of mandibular teeth. Mandibular tooth erosion is specific to the molars and premolars. In contrast, GERD generally affects all teeth in the maxilla.1 The erosive process is caused by chronic regurgitation of gastric acids.2 This stomach acid is extremely low pH, with literature reporting a pH of 1.5 to 1.2.2,3 Enamel has been shown to dissolve in acidic environments with a pH of 5.5 or less.4 This pathological process is often asymptomatic, leading to late-stage advanced erosion.2 The anterior clinical erosive (ACE) classification has been developed to categorize patients’ erosion severity and provide guidelines for therapeutic options.5
With the exception of ACE classifications 1 and 2, teeth that present with erosion due to GERD cannot generally be restored without altering the vertical dimension of occlusion (VDO).5 Moreover, altering the VDO causes greater complexity in planning and providing dental care. As long as the VDO is not altered by more than 5 mm, the patient rapidly adapts to the new position with no temporomandibular disorder (TMD) symptoms.6 Poyser et al7 demonstrated an efficient and simple method for altering the VDO through direct composite restorations. Specifically, both minimal tooth preparations and high patient satisfaction were reported.7 Furthermore, Vailati et al8 have demonstrated the use of composite in their so-called “three-step technique” to accurately transfer a diagnostic wax-up to a patient mouth using a clear polyvinyl siloxane (PVS) matrix. This method has been reported for lingual composite veneers, long-term full mouth provisionalization, and bonded functional prototypes (BFP).9–11 For example, Romero et al12 demonstrated that a BFP can be utilized not only as a diagnostic aid for alteration of the VDO, it can also be used as a preparation guide, reducing the amount of tooth structure removal and serving as a surgical template in cases that require gingivoplasty. Conservative tooth removal is imperative for patients with severe erosion. Therefore, this case report demonstrates the use of a bonded functional esthetic prototype in a patient with generalized-severe erosion as a diagnostic aid to increase VDO and preserve tooth structure prior to full mouth rehabilitation.

CASE REPORT
A 63-year-old male presented to the general practice residency program at the Dental College of Georgia at Augusta University with a chief complaint of “I am worried about my teeth breaking down more if I don’t get things fixed.” The reported medical history was significant for GERD. The patient had received GERD-related proton-pump inhibitor therapy with esomeprazole. No other significant medical history was reported. A comprehensive oral exam was performed and no signs of pathology were observed. His temporomandibular joints were asymptomatic, with no clinically detectable clicking or popping noted during mandibular translation, depression and elevation; similarly, no mandibular deviation or deflection were observed.

has a low smile line and visible incisal edge
wear, with a discrepancy of incisal position.
Radiographic examination and interpretation included a full mouth series, panoramic radiograph, and cone beam computed tomography. A lower left periapical radiograph revealed a radiolucent lesion around the root apices of tooth #19; however, #19 had recently received root canal therapy. Severe occlusal and lingual wear was observed on teeth #6, 7, 10, 11, 12, 13, 14 and 15. Lingual wear with close pulpal proximity was observed on teeth #6, 7, 10 and 11; additionally, teeth #30 and 31 were missing (Figure 1 and Figure 2). No pulpal sensitivity was reported for any teeth. There was no observed pathology with teeth #8 and 9. The existing maxillomandibular relationship demonstrated a collapsed VDO, with a lack of restorative space. This is evident in the preoperative image (Figure 3) that displays intact facial symmetry, with reduced lower facial-third and exaggerated marionette lines, suggesting a collapsed VDO. Therefore, the patient was diagnosed with ACE Classification 3,2,7 and his physician was consulted about the genesis of the patient’s GERD.

Dental treatment options that included the risks, benefits, prognosis, progression, time and costs were presented, and the patient agreed to a comprehensive plan. Photographs and study models were obtained, and a centric relation bite record and facebow were taken. The diagnostic casts were mounted on a semi-adjustable articulator. Due to the patient’s pulpal proximity on the lingual surfaces of the maxillary anterior teeth, it was determined this VDO increase would be sufficient to allow adequate restorative space. Periodontal evaluation indicated adequate gingival zenith levels, and no further periodontal surgery to correct super-eruption was necessary.



Through esthetic evaluation, the patient had satisfactory midline location and tooth display at full smile. The patient denied orthodontic treatment. The diagnostic wax-up was completed with a 4 mm increase in the VDO. Within the designed wax-up, mutually protected occlusion with ideal canine guidance was established and maintained throughout case progression. According to the BFP technique described by McLaren,13 a visible light-cured resin tray with clear PVS was utilized to accurately record the wax-up (Figure 4). Sharp edges were removed from the resin tray with a polishing bur. Using the clear PVS impression and tray, the posterior teeth were etched, primed, bonded and restored at the new VDO using a microhybrid composite.

Once this first step was complete, bimanual manipulation was used to verify centric occlusion. Adjustments were made as needed to remove any occlusal prematurities, heavy contacts, or nonworking contacts while the patient was deprogrammed. Four weeks later, the anterior teeth were restored following the same protocol previously described. The patient’s new occlusion was checked at 30 and 60 days postoperatively, with no signs or symptoms of discomfort reported (Figure 5, Figure 6 and Figure 7). During this trial period, implants were placed to replace teeth #30 and 31. It was decided that four months of healing would be sufficient for the implants and would also provide enough time to adjust to the new VDO. In order to accurately maintain VDO, crown preparations and cementation were divided into four stages:
- Stage 1: Maxillary posterior teeth
- Stage 2: Mandibular posterior teeth
- Stage 3: Mandibular incisors
- Stage 4: Maxillary incisors
A final impression was obtained at each stage, and temporaries were fabricated using the same matrices that were used for the prototypes. Upon receiving the completed full contour monolithic zirconia restorations, verification of marginal adaptation was checked, along with interproximal contacts and occlusion. During each individual stage, the crowns were air-abraded with alumina-oxide (50-um particle size), and their intaglio surfaces cleaned for 20 seconds and primed, which was left undisturbed for 60 seconds, per the manufacturer’s instructions. All restorations were bonded in the self-etch mode. After polymerization, occlusion was verified, adjusted as needed, and the restorations polished. For implants at sites #30 and 31, an implant-level impression was made with all other natural teeth during Stage 3, and screw-retained full contour zirconia crowns were delivered.



Upon delivery of the crowns during Stage 4, a final occlusal exam and adjustments were completed using a high-speed handpiece with a fine-grit diamond and copious amounts of water, making sure a mutually protected occlusion was in place (Figure 8 through Figure 12). After PVS impressions were obtained, new casts were mounted and an occlusal guard was fabricated. The guard was adjusted to allow canine guidance with posterior disocclusion during excursive movements. A follow-up appointment at four weeks was completed to verify esthetics and function (Figure 13). Minor occlusal adjustments were needed to address working side interferences, but, overall, the patient was satisfied with the outcome.
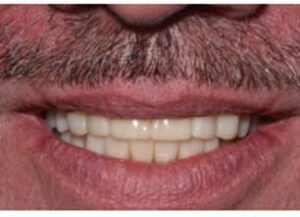
smile view postoperative of full contour
zirconia crowns.
DISCUSSION
In complex restorative cases with a loss of vertical dimension, one reliable way to determine the correct VDO is through prototype restorations.14 Metal onlays and occlusal TMD splints are one of many options to evaluate VDO and the necessary restorative space change. While these diagnostic options are conservative and require no additional mouth preparations, esthetics and patient compliance are among the many concerns with these techniques.15 The use of a silicone impression of the patient’s wax-up is a quick and reliable technique for restoring these patients at the correct diagnostic VDO, while providing the patient with a mock-up of the final restorations.12 A resin composite provisional allows the dentist to alter the VDO in a more conservative manner. Adding and removing composite is a short procedure that can be completed without any intraoral preparations. The bonded prototype allows the patient to function and evaluate esthetics over a period of time to ensure the final definitive treatment will satisfy the patient’s needs.

with full contour zirconia crowns.
After the patient has adapted to the new vertical position, the selection of a final restorative material requires the clinician to consider the severity of tooth structure loss.5 In this case, the patient originally presented with erosion on the mandibular occlusal and lingual surfaces, as well as the maxillary palatal, occlusal and incisal edges. While many definitive restoration options were available, the patient’s remaining tooth structure, as well as his previous pathological wear and erosion, were two important factors to consider. Ideal retention and resistance form requires a minimum of 3 mm occluso-cervically for premolars and anterior teeth, and 4 mm occluso-cervically for molars.16 Furthermore, regardless of restoration type, increasing surface area increases retention and resistance.17 Based on these principles and the location and severity of erosion, full coverage crowns were indicated to achieve ideal retention and resistance form. Due to previous erosion, full coverage crowns were indicated in order to withstand high occlusal function. Alternative veneering techniques have been shown to have significantly lower load-bearing capacity.18 Additionally, full coverage crowns enhance esthetics, with restorative margins unrecognizable during a full smile. Due to the patient’s previous erosive process, full coverage crowns protect all surfaces from future erosion. This definitive treatment option provides restorations that can withstand high occlusal forces and provide ideal retention and resistance form, while delivering an exceptional esthetic result.
Due to the patient’s pathological erosive process and remaining tooth structure, all crowns were delivered with self-etching resin cement. Resin cements have been shown to offer greater fracture resistance when compared to conventional glass ionomer luting cements and resin-modified glass ionomer luting cements.19 Research has shown that mechanical air abrasion, paired with ceramic primers, can support a durable bond to zirconia.20,21 Pulpal proximity was a significant concern when determining which adhesive system to select for this complex case. When comparing self-etch resin cements to etch-and-rinse resin cements, there are no significant differences in bond strength. However, self-etching resin cements minimize postoperative sensitivity due to the remaining dissolved calcium phosphates that are not present in etch-and-rinse systems. This self-etching system reduces the changes of collagen degradation and subsequent bond stability over time.22,23
At the day of delivery, significant time was dedicated to achieving the desired occlusion for the patient. A long-term BFP allowed the patient to be restored to mutually protected occlusion. During function, anterior guidance disoccludes posterior teeth and protects them from undesirable contacts.24 The patient could function on provisional restorations over time and provide feedback to the clinical team to help achieve an ideal occlusal scheme. This occlusal relationship was maintained during the delivery of the final crowns. Uniform contacts on all teeth in the arch ensure that no tooth receives excessive occlusal force; it also protects each tooth from any further occlusal damage, with force along each tooth’s long axis.24 This ideal occlusion scheme is even more important for the mandibular posterior dental implants. The patient’s previously damaged dentition will be protected with mutually protected occlusion and an occlusal splint.
CONCLUSION
This case report demonstrates the use of a BFP in a patient with generalized-severe erosion as a diagnostic aid to increase the VDO prior to full mouth rehabilitation. Through the use of a BFP, a reliable and repeatable VDO can be achieved and transitioned to a definitive full mouth rehabilitation.
KEY TAKEAWAYS
- The anterior clinical erosive (ACE) classification has been developed to categorize patients’ erosion severity and provide guidelines for therapeutic options.5
- With the exception of ACE classifications 1 and 2, teeth that present with erosion due to gastroesophageal reflux disease cannot generally be restored without altering the vertical dimension of occlusion (VDO).5
- Poyser et al7 proposed an efficient and simple method for altering the VDO through direct composite restorations.
- Furthermore, Vailati et al8 reported the successful use of composite to accurately transfer a diagnostic wax-up to a patient mouth using a clear polyvinyl siloxane matrix.
- Romero et al12 demonstrated that a bonded functional prototype can be utilized not only as a diagnostic aid for alteration of the VDO, it can also be used as a preparation guide, reducing the amount of tooth structure removal and serving as a surgical template in cases that require gingivoplasty.
- The bonded prototype allows the patient to function and evaluate esthetics over a period of time to ensure the final definitive treatment will satisfy the patient’s needs.
REFERENCES
- Imfeld T. Dental erosion. Definition, classification and links. EuJ J Oral Sci. 1996;104(Pt 2):151–155.
- Raibrown A, Giblin LJ, Boyd LD, Perry K. Gastroesophageal reflux disease symptom screening in a dental setting. J Dent Hyg. 2017;91:44–48.
- Beasley DE, Koltz AM, Lambert JE, Fierer N, Dunn RR. The evolution of stomach acidity and its relevance to the human picrobiome. PLoS One. 2015;10:e0134116.
- Lussi A, Schlueter N, Rakhmatullina E, Ganss C. Dental erosion — an overview with emphasis on chemical and histopathological aspects. Caries Res. 2011;45;(Suppl 1):2–12.
- Vailati F, Belser UC. Classification and treatment of the anterior maxillary dentition affected by dental erosion: the ACE classification. Int J Periodontics Restorative Dent. 2010;30:559–571.
- Moreno-Hay I, Okeson JP. Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J Oral Rehabil. 2015;42:875–882.
- Poyser NJ, Briggs PF, Chana HS, Kelleher MG, Porter RW, Patel MM. The evaluation of direct composite restorations for the worn mandibular anterior dentition — clinical performance and patient satisfaction. J Oral Rehabil. 2007;34:361–376.
- Vailati F, Vaglio G, Belser UC. Full-mouth minimally invasive adhesive rehabilitation to treat severe dental erosion: a case report. J Adhes Dent. 2012;14:83–92.
- Vailati F, Belser UC. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 3. Eur J Esthet Dent. 2008;3:236–257.
- Vailati F, Belser UC. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 2. Eur J Esthet Dent. 2008;3:128–146.
- Vailati F, Belser UC. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 1. Eur J Esthet Dent. 2008;3:30–44.
- Romero MF, Babb CS, Johnson B, Arce RM. Bonded functional esthetic prototypes as a diagnostic aid. Decisions in Dentistry. 2018;4(7):8–10,12
- McLaren EA. Bonded functional esthetic prototype: an alternative pre-treatment mock-up technique and cost-effective medium-term esthetic solution. Compend Contin Educ Dent. 2013;34:596–607.
- Turner KA, Missirlian DM. Restoration of the extremely worn dentition. J Prosthet Dent. 1984;52:467–474.
- Prasad S, Kuracina J, Monaco EA Jr. Altering occlusal vertical dimension provisionally with base metal onlays: a clinical report. J Prosthet Dent. 2008;100:338–342.
- Goodacre CJ, Campagni WV, Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 2001;85:363–376.
- Gilboe DB, Teteruck WR. Fundamentals of extracoronal tooth preparation. Part I. Retention and resistance form. 1974. J Prosthet Dent. 2005;94:105–107.
- Beuer F, Stimmelmayr M, Gueth JF, Edelhoff D, Naumann M. In vitro performance of full-contour zirconia single crowns. Dent Mater. 2012;28:449–456.
- Mitchell CA, Douglas WH, Cheng YS. Fracture toughness of conventional, resin-modified glass-ionomer and composite luting cements. Dent Mater. 1999;15:7–13.
- Inokoshi M, Kameyama A, Munck JD, Minakuchi S, Meerbeek BV. Durable bonding to mechanically and/or chemically pre-treated dental zirconia. J Dent. 2013;41:170–179.
- Zandparsa R, Talua NA, Finkelman MD, Schaus SE. An in vitro comparison of shear bond strength of zirconia to enamel using different surface treatments. J Prosthodont. 2014;23:117–123.
- da Rosa WL, Piva E, da Silva AF. Bond strength of universal adhesives: a systematic review and meta-analysis. J Dent. 2015;43:765–776.
- Saad Del D, Atta O, El-Mowafy O. The postoperative sensitivity of fixed partial dentures cemented with self-adhesive resin cements: a clinical study. J Am Dent Assoc. 2010;141:1459–1466.
- Dawson PE. Functional Occlusion: From TMJ to Smile Design. Edinburgh: Elsevier Mosby; 2006.
The authors have no commercial conflicts of interest to disclose.
From Decisions in Dentistry. February 2021;7(2):10–12,14.



