
Restorative Therapy With Fiber-Reinforced, Resin Composite Bonded Fixed Partial Dentures
This case report involves conservative treatment using a fiber-reinforced, resin composite bonded fixed partial denture to replace missing mandibular central incisors.
Fiber-reinforced composite fixed partial dentures (FPDs) have been shown to be a valid option for replacing missing teeth in a manner that is both predictable and conservative.1 For three-unit fiber-reinforced anterior FPDs, acceptable two-year success rates surpassing 90% have been reported.2,3 While there is an increased risk of debonding when compared to conventional FPDs, there are also advantages of minimizing loss of tooth structure, decreased cost, increased esthetics (when compared to porcelain-fused-to-metal resin-bonded FPDs), and high patient acceptance.4 Because this restoration can be fabricated in-office, laboratory costs are minimized and opportunities for immediate placement following extraction increase — which could reduce the time a patient has unrestored anterior edentulous spaces.
The patient in this case report desired a rapid long-term interim replacement for her mandibular centrals after extraction of tooth #25 rendered her existing Essix prosthesis unusable. A fiber-reinforced, resin composite bonded FPD restored the appearance of the mandibular anterior segment while the patient considered her options for mandibular reconstruction.
CLINICAL REPORT
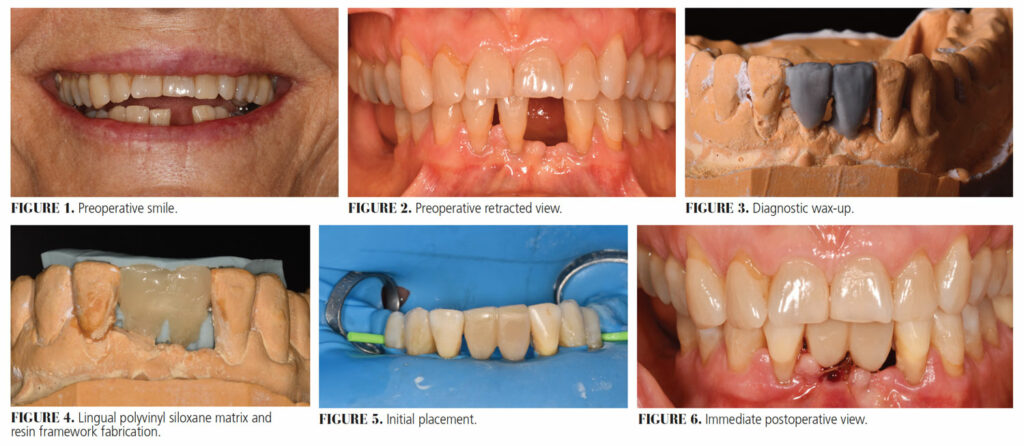
A 69-year-old female presented to the Advanced Education in General Dentistry clinic at the Dental College of Georgia at Augusta University with a chief complaint of, “I am missing a tooth and I dislike the removable temporary I am wearing” (Figure 1 and Figure 2). The medical history was noncontributory, with the patient taking daily pravastatin and aspirin. The patient was periodontally stable, but had a history of bone loss. She was missing teeth #24 and 30 to 32. Class III mobility was present on tooth #25, with class I mobility on teeth 23 and 26. The occlusion was stable and the patient was caries-free. She had an Essix retainer to cosmetically replace tooth #24, but she found the appliance uncomfortable and rarely wore it. The patient favored fixed prosthetics to replace teeth #24, 25 and 30, but was aware that considerable bone grafting would be necessary for implant placement in any of these sites; thus, she was willing to consider all options.
After evaluation, it was recommended the patient receive an immediate fiber-reinforced, resin composite bonded FPD as a long-term provisional replacement for her mandibular central incisors, which would restore her appearance and afford time to consider various periodontal and prosthetic options for definitive restoration of her mandibular dentition. The patient accepted this plan, which included extraction of tooth #25 and replacement of both mandibular central incisors with a fiber-reinforced, lab/chairside-fabricated resin-bonded FPD spanning teeth #22 to 27.
Alginate impressions, facebow and protrusive records were made. The two central incisors were waxed up on the patient’s mounted cast (Figure 3). A polyvinyl siloxane lingual matrix was fabricated based on this wax-up. The waxed-up cast was duplicated and a groove 1 mm deep and 3 mm wide (which allowed space for the reinforcing fiber) was prepared into the lingual surface of the cast of the two central incisors being replaced. Using this altered cast, a 3-mm-wide piece of polyethylene fiber of sufficient length to reach the canines was cut and placed in the groove. The fiber mesh was infiltrated with resin, adapted, and light cured. Next, this light-cured fiber matrix was transferred to a duplicate of the patient’s cast (from which both of central incisors had been removed). Using the lingual matrix fabricated from the wax-up, a lingual shell of composite was fabricated, attached to the fiber, and light cured (Figure 4).

Once the lab portion was completed, the patient was scheduled and tooth #25 was extracted. Sutures were placed and a rubber dam was used for isolation. A lab-fabricated FPD matrix was tried in, and then bonded using phosphoric acid etching, a compatible adhesive system and flowable resin composite (Figure 5). A shade A3.5 resin composite was used for the final facial layer of the pontics, which would match the adjacent teeth. Finishing and polishing were completed using finishing discs and rubber points (Figure 6).
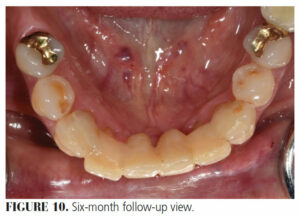
The patient returned after one week for suture removal, and again after three months (Figure 7 and Figure 8) and six months (Figure 9 and Figure 10) for follow-up. At six months, it was observed that the ridge at the #25 extraction site had receded further than expected and lacked contact with the pontic. The patient was pleased with both the function and esthetics of the prosthesis and with the overall function of her mandibular dentition. She declined the addition of resin to the pontics to restore ridge contact and stated that she was content to “wait and see” about the lifespan of this prosthesis before undertaking further mandibular restoration.
DISCUSSION
This technique of fabricating a framework in the laboratory allowed for reduced chairtime, as well as the ability to light cure the resin infiltrating the fiber without risk of salivary contamination of the fiber. The authors elected to custom fabricate the pontics using resin composite, believing the prosthesis would be stronger than if denture teeth were employed because of more effective copolymerization between the pontics and framework. Not fully fabricating the pontics in advance also allowed shade and contour matching intraorally.
A study by Kumbuloglu and Ozcan5 evaluated 175 indirect fiber-reinforced resin composite bonded FPDs for up to 58 months and found a 98% survival rate, with all but one failure readily repairable without replacement. Considering this restoration’s reliance on adhesive bonding, Malmstrom et al1 recommend rubber dam isolation, as well as cleaning the abutment teeth with plain pumice and microabrasion before a traditional etch-and-rinse bonding protocol is initiated. This level of isolation was particularly indicated for this case due to bleeding from the site of the same-day extraction of tooth #25.
This restoration also conformed to Vallittu’s6 recommendations of at least a 2.5 mm connector height and a 2 mm height of bonding area on anterior abutment teeth. The authors favorably noted that preparation of lingual surfaces was unnecessary for this mandibular FPD, since there were no concerns about occlusal clearance. The authors considered double abutting this FPD to be favorable, given the mobility of the adjacent lateral incisors — but whether a double-abutment design for this type of FPD in general is more favorable than single abutting has not been established in the extant literature.
The authors intend to evaluate the prosthesis yearly and expect that while minor repair may become necessary, the worst-case scenario of FPD loss is unlikely and can customarily be addressed through rebonding should it occur.
SUMMARY
The authors consider the indirect fiber-reinforced, resin bonded FPD presented here to be a conservative, esthetic and affordable restoration of a mandibular anterior edentulous space. Fabricating the framework in the laboratory and completing the restoration chairside allowed more control over shade and contour matching than fabricating the entire prosthesis indirectly.
KEY TAKEAWAYS
- Fiber-reinforced composite fixed partial dentures (FPDs) have been shown to be a valid option for replacing missing teeth in a manner that is both predictable and conservative.1
- While there is an increased risk of debonding when compared to conventional FPDs, there are also advantages of minimizing loss of tooth structure, decreased cost, increased esthetics when compared to porcelain-fused-to-metal resin-bonded FPDs, and high patient acceptance.4
- Because this restoration can be fabricated in-office, laboratory costs are minimized and opportunities for immediate placement following extraction increase — which could reduce the time a patient has unrestored anterior edentulous spaces.
- The technique of fabricating a framework in the laboratory allowed for reduced chairtime, as well as the ability to light cure the resin infiltrating the fiber without risk of salivary contamination of the fiber.
- Not fully fabricating the pontics in advance also allowed shade and contour matching intraorally.
- A study by Kumbuloglu and Ozcan5 evaluated 175 indirect fiber-reinforced resin composite bonded FPDs for up to 58 months and found a 98% survival rate, with all but one failure readily repairable without replacement.
- The authors of this report consider the indirect fiber-reinforced, resin bonded FPD — as presented in this case — to be a conservative, esthetic, and affordable restorative choice for a mandibular anterior edentulous space.
References
- Malmstrom H, Dellanzo-Savu A, Xiao J, et al. Success, clinical performance and patient satisfaction of direct fibre-reinforced composite fixed partial dentures — a two-year clinical study. J Oral Rehabil. 2015;42:906–913.
- van Heumen CC, van Dijken JW, Tanner J, et al. Five-year survival of 3-unit fiber-reinforced composite fixed partial dentures in the anterior area. Dent Mater. 2009;25:820–827.
- Vallittu PK, Sevelius C. Resin-bonded, glass fiber-reinforced composite fixed partial dentures: a clinical study. J Prosthet Dent. 2000;84:413–418.
- Burke FJ. Resin-retained bridges: fibre-reinforced versus metal. Dent Update. 2008;35:521–522,524–526.
- Kumbuloglu O, Ozcan M. Clinical survival of indirect, anterior 3-unit surface-retained fibre reinforced composite fixed dental prosthesis: Up to 7.5-years follow-up. J Dent. 2015;43:656–663.
- Vallittu PK. Survival rates of resin-bonded, glass fiber-reinforced composite fixed partial dentures with a mean follow-up of 42 months: a pilot study. J Prosthet Dent. 2004;91:241–246.
From Decisions in Dentistry. December 2021;7(11):8-10.


