 CHRISCHRISW/ISTOCK/GETTY IMAGES PLUS
CHRISCHRISW/ISTOCK/GETTY IMAGES PLUS
Oral Manifestations of Celiac Disease
Patients with this genetic autoimmune disorder are subject to significant oral health effects.
This course was published in the March 2020 issue and expires March 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define celiac disease (CD), its prevalence, and clinical signs.
- Describe the effect of CD on nutrient absorption.
- Identify the oral conditions that may serve as risk factors for CD.
Celiac disease (CD) is a hereditary, autoimmune disease induced by a reaction to gluten. Gluten is found in wheat (used in breads, soups, pastas, cereals, sauces and salad dressings); rye (rye breads and beer); and barley (malt products, food colorings, soups, beer and brewer’s yeast).1,2 Nonfood products that contain gluten — such as Play-Doh, cosmetics, skin and hair products, toothpaste and mouthrinse — may cause individuals to transfer gluten from the hands to the mouth.1,2
On a global scale, CD affects approximately one in 100 people internationally.3 The United States, Argentina, Italy, Germany, Denmark, and Finland have a higher prevalence of CD compared with other countries. Found more often in white females, CD is also hereditary. Those with a parent, child or sibling with CD are at a one in 10 risk of also receiving a CD diagnosis.4 Environmental factors — such as the introduction of gluten at an early age, absence of breastfeeding, and viral infections during infancy — may increase the risk of this disease.5,6
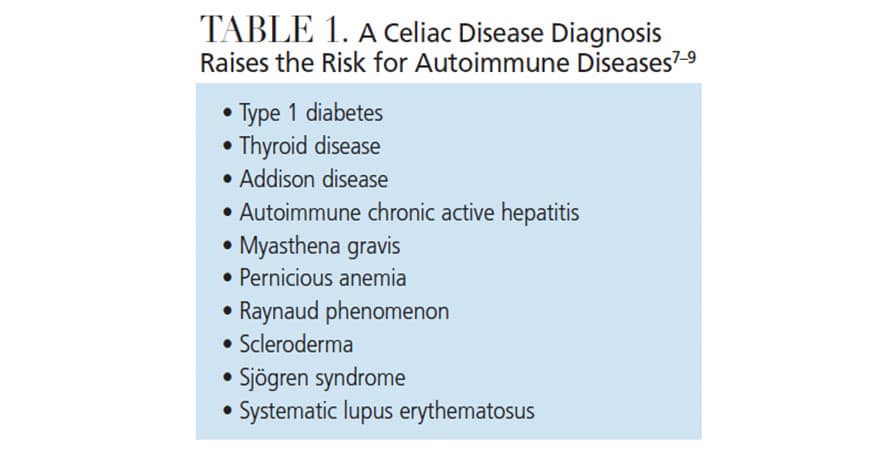
In the United States, 2.5 million individuals remain undiagnosed, which can lead to significant health problems ranging from iron-deficiency anemia to infertility, and miscarriage to neurological problems.4 The disease can appear at any age, and a diagnosis raises the risk for other autoimmune diseases that are genetically and immunologically linked to CD (Table 1).7–9
The clinical signs of CD differ between children and adults. Among children, CD may cause weight loss, delayed tooth eruption, stained, pocked and grooved enamel defects, and recurring aphthous ulcers. Signs of CD in adults may include abdominal discomfort, chronic diarrhea, bloating, weight loss, joint pain, muscle cramping, seizures, skin rashes, infertility, miscarriage, peripheral neuropathy, osteoporosis, atrophic glossitis, xerostomia and aphthous ulcers.10,11
NUTRIENT ABSORPTION
By damaging the villi of the small intestines, CD impedes the body’s ability to absorb nutrients (Figure 1). When individuals with the disease are exposed to alpha gliadin, a protein found in gluten, the body creates a T-cell-mediated inflammatory response in which IgA antitussive transglutaminase, antiendomysial and antigliadin antibodies are released. This reaction damages the brush border in the small intestine, which consists of folds of Kerckring that contain villi and microvilli used for nutrient absorption. Through the inflammatory response, the villi are flattened.
The decreased absorption of nutrients caused by CD includes those that play a key role in tooth development, such as the minerals calcium and fluoride.
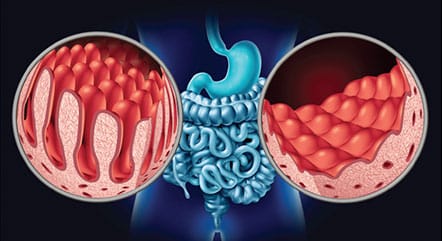
the villi of the small intestine. In this figure, healthy villi appear on the left,
while villi damaged by CD are shown at right. WILDPIXEL/ISTOCK/GETTY IMAGES PLUS
DIAGNOSIS
Early detection and diagnosis can be difficult because patients are frequently unaware of their risk for the disease. Finances may prohibit diagnosis when there is a lack of health insurance or financial ability to consult a primary physician. In addition, CD mimics irritable bowel syndrome and lactose intolerance, further increasing the challenges associated with diagnosis.
The following are part of a CD diagnosis:
- Presence of clinical signs, including rash, fullness in the abdomen, deformity of tooth enamel, and history of aphthous ulcers.
- Genetic blood tests (more than 40 genes are associated with CD; HLA-DQ2 and HLA-DQ8 are present in 85% of patients).
- Intestinal biopsy of the small intestine.
- Skin biopsy to check for antibodies if dermatitis herpetiformis is present.
ORAL SIGNS AND EFFECTS
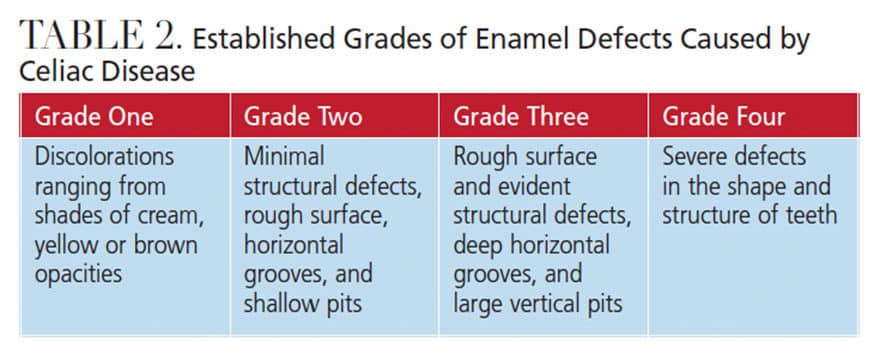
Oral health professionals should be aware of the signs of CD, including enamel deformity reported by established enamel grades of CD (Table 2) and history of recurring aphthous ulcers and dermatitis herpetiformis.12,13
Children with CD are at increased risk for dental caries.4 Delayed tooth eruption, mandibular jaw defects, enamel impairments, altered matrix formation, hypocalcification, and burning sensations in the oral cavity are other oral signs of CD. Patients who develop CD before age 7 are at greatest risk of negative effects in their permanent dentition. Dental defects can be used as a warning sign of CD in children and infants.14,15 Children with CD may develop patchy white-yellow colorations on their teeth, or enamel hypoplasia, which may cause the dentition to appear ridged and pitted. In some cases, the teeth may present with a distinct groove, a sign of a significant enamel impairment.16,17
Patients with CD are at increased risk for xerostomia, which increases the risk of caries, aphthous ulcers, aphthous stomatitis, atrophic glossitis, and, in some cases, oral cancer — especially squamous cell carcinoma of the oropharynx.4,7,18–21
IMPORTANCE OF INTERDISCIPLINARY COLLABORATION
When treating patients with CD, interdisciplinary collaboration and effective communication between the dentist, dental hygienist and all medical team members are imperative. The first step is to consult with the patient’s medical team prior to initiating dental treatment. The medical team will have a wide-range view of the patient’s current health status, and can provide guidance on the appropriateness of dental care.
In dental practice, dental hygienists are often the first point of contact with patients. As such, they must be aware of any dental products that contain gluten, such as prophy paste, toothpaste, and floss. Alternative products for patients with CD should be made available, and the practices’ dealer representatives should be able to suggest gluten-free products to stock.
Taking diagnostic radiographs, performing a thorough clinical assessment, and gathering a concise medical, dental and familial history are the foundations of a decisive and complete treatment plan.
Dental team members should be aware of the possible oral manifestations that can arise in patients with CD. Some adjustments in care may be needed to ensure patient comfort. For example, clinicians can recommend products to soothe aphthous ulcers, or suggest use of an extra-soft toothbrush, especially if there is irritation in the oral cavity. In addition, if the patient has xerostomia, moisturizing oral health products are recommended, as well as home fluoride treatment (with possible tray fabrication application). Fluoride varnish is helpful to reduce caries risk due to its viscosity and effective uptake within tooth structure.
Patients with CD will need preventive services on three- to four-month intervals in order to review and evaluate their oral health status. A thorough dietary analysis will prove helpful when educating patients about how to improve their nutritional intake, especially in regard to calcium and fluoride — which are imperative to optimal oral health. This analysis should be done in collaboration with the primary care physician and/or dietitian.
CASE STUDY 1
A 27-year-old woman presented to the dental office with concerns regarding the esthetics of her smile. She had red, ulcerated tissue and bleeding, with plaque and calculus irritating the marginal gingiva (Figure 2). The resulting pain interfered with her ability to brush regularly. Her medical history noted a diagnosis of CD; allergies to phenazopyridine hydrochloride, hydromorphone hydrochloride, penicillin and azithromycin; hypertension; chronic bronchitis and cough; sinus problems; allergy/hives; bruises easily; ulcers; syncope; and vertigo. She had a history of anemia and arthritis and was on a daily calcium supplement. Her medication regimen included hydrocodone 500 mg, three times daily; liquid lidocaine 2% viscous solution, 1 teaspoon every six to eight hours; and alprazolam, 5 mg daily.
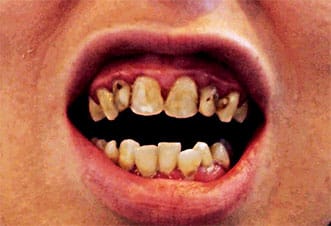
Tooth #16 was partially erupted with severe caries noted, and the crown was decayed to the gumline, with possible chronic periapical abscess present. The patient had severe caries throughout her dentition. Porcelain-fused-to-metal (PFM) crowns were needed on #6 to 11 due to severe caries. Teeth #15 and 16 mesial-occlusal-distal required extraction due to severe caries.
On the initial appointment, the dentist suggested the patient use prescription-strength fluoride gel in fabricated bleaching trays to wear once daily. Although referral to a specialist was recommended, the patient declined due to a lack of dental insurance and financial constraints.
The initial treatment plan was to place PFM crowns on #6 to 11. The dentist completed resin restorations on the #7, 10 and 11 facials due to severe caries and enamel breakdown on these surfaces, which was a temporary solution.
At another appointment, a resin-one surface posterior restoration was placed on #14 lingual. The next week, the patient reported losing the restoration on #14, accompanied by severe pain described as “fire ants continually biting.” The dentist suggested extraction by an oral surgeon. She was given a prescription for hydrocodone bitartrate/acetaminophen and zithromax/azithromycin for five days.
The following week, the patient reported no improvement and still had burning near the teeth that had recently been filled. She was given another prescription for hydrocodone bitartrate/acetaminophen and viscous lidocaine 100 ml for pain. The patient was unable to return to the dental practice for treatment and did not continue the treatment plan.
CASE STUDY 2
An 18-year-old woman with CD but no other health history concerns presented with generalized moderate-to-severe decalcification and recurrent caries (Figure 3). The dentist suggested wearing trays filled with casein phosphopeptide-amorphous calcium phosphate paste overnight. A review of acidity intake was performed and the patient’s consumption of diet soft drinks was discussed, with the recommendation to limit or eliminate such consumption. Fluoride varnish was applied at each preventive maintenance appointment. On two separate occasions, the patient was prescribed 21 pills of 500 mg amoxicillin (with no refills) for infection.

disease but no other health history concerns
presented with generalized moderate-to-severe decalcification and recurrent caries.
DISCUSSION
As these case studies demonstrate, CD can have a deleterious effect on oral health, especially for patients who have limited access to professional dental care. In terms of restorative treatment, patients with CD can be challenging to treat due to the fragility of their dentition. Each time a dentist prepares a tooth for composite restorations, more tooth structure is sacrificed and the strength of the restoration is diminished. In addition, some patients with CD have a tendency for diminished healing, hence, there is significant concern when extracting teeth.
Patients with CD may have no other choice than to have their teeth extracted. Decreased healing can affect the oral tissues and bone support; in addition, patients may struggle with wearing dentures due to the potential of ulcerative gingiva and increased inflammation on the ridges of bone. These patients should be educated about all aspects of treatment, and informed of the treatment goals and strategies designed specifically for their needs. Obtaining informed consent is of the utmost importance.
CONCLUSION
The prevalence of CD is growing, especially in the United States.22 Patients may seek dental care without knowledge of their condition. Fortunately, oral health professionals are trained to note the oral signs and symptoms of this disease. A thorough medical, familial and dental history will aid in proper diagnosis and treatment.
Oral health professionals who suspect CD should speak not only with the patient, but also with his or her physician and/or dietitian to determine an effective treatment strategy. This interdisciplinary approach will support the successful management of CD, as well as mitigate its effects on oral health.
REFERENCES
- Celiac Disease Foundation. The big 3: wheat, barley, rye. Available at: celiac.org/gluten-free-living/what-is-gluten/. Accessed February 3, 2020.
- Kelly CP, Bai JC, Liu E, Leffler DA. Advances in diagnosis and management of celiac disease. Gastroenterology. 2015;148:175–186.
- Singh P, Arora A, Strand TA, et al. Global prevalence of celiac disease: Systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16:823–836.
- Celiac Disease Foundation. Oral Health. Available at: https://celiac.org/about-celiac-disease/related-conditions/oral-health/. Accessed February 3, 2020.
- Nelms M, Sucher K, Lacey K, Roth SL. Nutrition Therapy and Pathophysiology. 3rd ed. Boston: Cengage Learning; 2019:405–406.
- Parzanese I, QehajaJ D, Patrinicola F, Aralica M, Chiriva-Internate M, Stifter S. Celiac disease: from pathophysiology to treatment. World J Gatrointest Pathophysiol. 2017;8:27–38.
- Celiac Disease Foundation. What Is Celiac disease? Available at: celiac.org/about-celiac-disease/what-is-celiac-disease/. Accessed February 3, 2020.
- Laurett E, Rodrigo L. Celiac disease and autoimmune-associated conditions. Biomed Res Int. 2013:127589.
- Gluten Intolerance Group. Associated Autoimmune Diseases. Available at: gluten.org/wp-content/uploads/2015/02/EDU_AssociatedAuto_5.12.14.pdf. Accessed February 3, 2020.
- Byrd-Bredbenner C, Moe G, Beshgetoor D, Berning J. Wardlaw’s Perspectives in Nutrition. 9th ed. New York: McGraw-Hill Co Inc; 2013:142–661.
- Vivas S, Vaquero L, Rodriguez-Martin L, Caminero A. Age-related differences in celiac disease: specific characteristics of adult presentation. World J Gastrointest Pharmacol Ther. 2015;6:207–212.
- Rashid M, Zarkadas M, Anca A, Limeback H. Oral manifestations of celiac disease: a clinical guide for dentists. J Can Dent Assoc. 2011;77:39.
- Amato M, Zingone F, Caggiano M, Iovino P, Bucci C, Ciacci C. Tooth wear is frequent in adult patients with celiac disease. Nutrients. 2017;9:1321.
- Zylberberg HM, Lebwohl B, RoyChoudhury A, Walker M, Green PH. Predictors of improvement in bone mineral density after celiac disease diagnosis. Endocrine. 2018;59:311–318.
- Al-Homaidhi M. The effect of celiac disease on the oral cavity. Available at: medcrave.com/articles/det/12437/ The-Effect-of-Celiac-Disease-on-the- Oral-Cavity-A-Review. Accessed February 3, 2020.
- Sheetal A, Hiremath VK, Patil AG, Sajjansetty S, Kumar SR. Malnutrition and its outcome-a review. J Clin Diagn Res. 2013;7:178–180.
- Anderson J. Effects of celiac disease on your teeth and gums. Available at: verywellhealth.com/effects-of-celiac-disease-on-dental-health-4115330. Accessed February 3, 2020.
- Drummond BK, Kilpatrick N. Planning and Care for Children and Adolescents With Dental Enamel Defects: Etiology, Research and Contemporary Management. Berlin: Springer; 2015:1–14.
- Dombrowski M. Celiac teeth: celiac disease and oral health. Available at: colgate.com/en-us/oral-health/conditions/gastrointestinal-disorders/celiac-teeth-celiac-disease-oral-health-0715. Accessed February 3, 2020.
- Saccucci M, DiCarlo G, Bossu M, Giovarruscio F, Salucci A, Polimeni A. Autoimmune diseases and their manifestations on oral cavity: Diagnosis and clinical management. J Immunol Res. 2018;2018:6061825.
- Lewis MA, Wilson NH. Oral ulceration: causes and management. The Pharmaceutical Journal. 2019;302(7923):e10.
- Offord C. The Celiac Surge. Available at: https://www.the-scientist.com/features/the-celiac-surge-31438. Accessed February 3, 2020.
From Decisions in Dentistry. March 2020;6(3):36–39.