YVDAVYD/ISTOCK/GETTY IMAGES PLUS
YVDAVYD/ISTOCK/GETTY IMAGES PLUS
Childhood Obesity Screening and Education in Dental Practice
Although there are many causes of childhood obesity, oral health professionals can help manage this public health issue by providing screening and education based on individual risk factors.
This course was published in the April 2020 issue and expires April 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define obesity and identify its prevalence among American children and adolescents.
- Discuss the causes of obesity among children and adolescents.
- Explain the relationship between obesity and oral health, and note possible interventions.
Childhood obesity is one of the most significant public health challenges of the 21st century, both in the United States and globally.1,2 Childhood obesity is a multifactorial disease with risk factors related to genetics, development and the environment.3 Regardless of the causes of childhood obesity, these children are more likely to become obese adults, and are at risk for developing additional chronic medical conditions, such as dyslipidemia, hypertension, type 2 diabetes or obstructive sleep apnea.4–6 Childhood obesity is also related to depression, anxiety, low self-esteem and social problems, such as bullying.5 The persistence of these comorbid conditions into adulthood is not only costly to personal health, it presents an economic burden on society, as well.6 With one in three children in the United States overweight or obese, early identification and intervention are critical.4 Fortunately, dental teams can help manage this public health issue by providing patient screening and education based on individual risk factors.
Obesity is defined as an excess of body fat.7 The most common methods to measure body fat in the clinical environment are body mass index (BMI), skin-fold thickness and waist circumference.7 It is important to realize BMI is not a direct measure of body fat, but an alternative measure reflecting weight as related to height (weight/height²).8 The U.S. Centers for Disease Control and Prevention (CDC) considers this method sufficient for screening purposes, as it is an easy and quick calculation.9 More accurate direct measurements include bioelectric impedance analysis, dual energy X-ray absorptiometry, densitometry, hydrometry and magnetic resonance imaging.8 The CDC defines obesity in children and young people (ages 2 to 20) as having a BMI at or above the 95th percentile for children and young people of the same age and sex.10 This use of an age- and sex-specific percentile differs from calculating BMI for adults, and is necessary for children and teens, as body composition varies with age and gender.7,10 Some suggest the BMI calculator potentially exaggerates obesity rates for muscular children, as it does not distinguish fat from fat-free mass (muscle and bone,) or account for differing maturation patterns between ethnic groups.7
PREVALENCE AND TRENDS
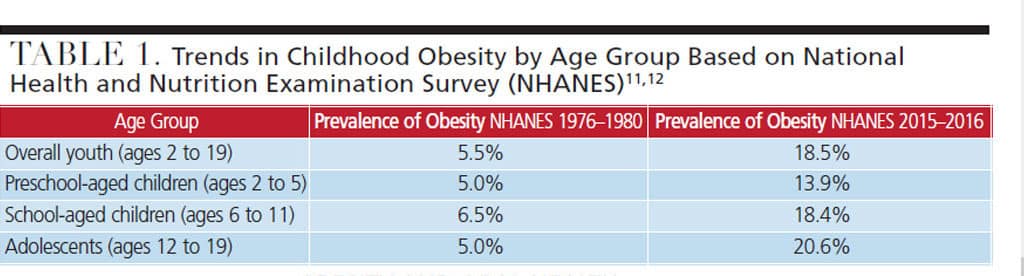
According to the most recent data from the 2015–2016 National Health and Nutrition Examination Survey (NHANES), prevalence of obesity among youth ages 2 to 19 in the United States was 18.5%, representing a significantly increasing trend.11 These rates have more than tripled since the 1976–1980 NHANES results of 5.5%.12 Table 1 compares results of the NHANES conducted in 1976–1980 and 2015–2016.11,12
According to the 2015–2016 NHANES, obesity rates differ significantly by race and ethnicity. Compared to white and Asian children, obesity rates were found to be higher among Latino and black children, with Latino boys and black girls most likely to be obese. In general, boys are slightly more likely to be obese than girls.12 On a global level, the World Health Organization estimates that from 1990 to 2016, the number of overweight or obese children younger than 5 increased from 32 million to 41 million; it also estimates this number will grow to 70 million by 2025.2
CAUSES OF CHILDHOOD OBESITY
The most common cause of childhood obesity is the consumption of more calories than a child or young person expends (known as a positive energy balance), in combination with being genetically predisposed to weight gain.4,5,7 Though genetic predisposition is a factor, it is not the single cause of obesity in most children.4 The majority of cases result from the interaction of multiple modifiable and nonmodifiable risk factors, including:
- Genetics
- Endocrine (hormonal)
- Nutrition: portion sizes and consumption of fast food and sugar-sweetened beverages (SSBs)
- Lack of physical activity (energy imbalance); high levels of television viewing/screen time
- Social and environmental factors
- Sleep duration and quality
- Race/ethnicity
- Socioeconomic status
- Psychosocial, cultural and community (neighborhood design and safety)3,5,6,13
In addition to familial and societal influence, evolution plays an important part in shaping children’s food preferences. Humans are biologically designed to prefer sweet and salty foods and avoid bitter tastes.3 These preferences that once served as a means to help detect energy-rich foods and avoid poisons are now a risk factor for obesity. They persist into adolescence, leaving children and young adults especially vulnerable to poor food choices. Flavor and food preferences can be modified early in life, though children must be repeatedly exposed to certain foods to learn to like them.3 Unfortunately, research statistics reveal the following:3
- Beginning at age 2, children are more likely to eat a manufactured sweet than a fruit or vegetable
- By age 4, 99% of children exceed the recommended sugar intake, while 92% do not eat the minimum recommended amount of vegetables
- On any given day, 20% to 35% of children 6 months and older do not eat fruit, and 30% to 40% of children do not eat vegetables
- Sweets and sweetened beverages make up more than one-third of the increase in calories from the ages of 6 months to 4 years
- The odds of consuming SSBs at age 6 is nearly doubled if they are consumed in infancy
OBESITY AND ORAL HEALTH
Many studies have attempted to establish a correlation between obesity and caries prevalence, with a focus on the consumption of SSBs or sugar-containing beverages (SCBs) by adolescents and adults. The latter include SSBs and other beverages, such as 100% fruit juice (which contains naturally occurring glucose and fructose).14 Findings specific to childhood obesity include a positive association between SCBs and the accumulation of fat in the lower torso around the abdominal area (central adiposity), and a direct association between caries and obesity.15–20
Other studies have noted an increased risk of caries in obese children, but do not identify a causative relationship between the two, suggesting common risk factors are most likely the reason for their coexistence.18,19 In general, consumption of SSBs/SCBs and other foods high in sugar is a risk factor for obesity, as well as caries.
The association between childhood obesity and periodontal disease has also been investigated, with results demonstrating a positive correlation.21 In addition to these evidentiary relationships, dental professionals should consider the impact of the oral health effects of potential sequelae from comorbidities, such as diabetes and obstructive sleep apnea.22
INTERVENTIONS IN THE DENTAL SETTING
While multiple factors contribute to the chronic diseases of obesity and caries, both have dietary components — with a key risk factor being the consumption of SSBs/SCBs.14,23 The majority of children and adolescents in the United States consume 270 calories/68 g of sugar from SSBs on a daily basis, exceeding the daily intake recommended by the American Heart Association (25 g) and World Health Organization (less than 5% to 10% of total energy intake, equivalent to 25 g to 50 g).24,25
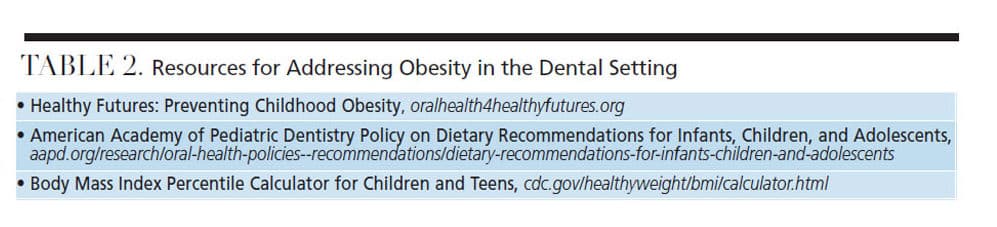
Due to the nature of the dental setting, oral health professionals are in a unique position to identify children at risk for both diseases, promote healthy food choices, and provide referrals to specialists. As part of efforts to manage this public health issue, it is increasingly important to become part of the interprofessional team that includes physicians, registered dietitians and public health officials. Table 2 lists resources that dental teams can use to address obesity in practice.
Significant research has been conducted on the attitudes and beliefs held by oral health professionals about their role in screening for obesity and nutritional/lifestyle counseling. This research suggests 30% to 50% of dental professionals express discomfort with addressing adult or childhood obesity in the clinical setting. The reasons include:
- Belief that obesity is not directly related to oral health
- Fear of appearing judgmental or offensive
- Time constraints
- Lack of training in weight loss counseling
- Feeling unqualified to provide noncaries-related nutritional counseling
- Lack of patient interest/willingness
- Weight seen as a medical rather than an oral health issue
- Lack of reimbursement for services (such as screening/nutritional counseling)26–28
Other barriers include a lack of curriculum content addressing childhood obesity and nutritional intervention in dental education programs, and parental/caregiver perception of healthy weight.26–29 More than 50% of parents and caregivers of overweight/obese children underestimate their child’s weight.30
Research has also provided some hopeful data in the form of positive parental/caregiver attitudes toward weight screening and nutritional counseling in the dental setting. Not only did 95% of caregivers feel the dental office was an appropriate place to receive information about exercise and healthy eating habits, they also believe oral health professionals are well positioned to discuss healthy weight goals.26
The results of a pilot project employing a healthy weight intervention (HWI) protocol in a pediatric dental setting demonstrated positive results.31 The protocol implemented motivational interviewing, which is based on individuals setting behavioral goals they believe they can attain.31 The HWI provided health report cards, with health behavior modifications based on risk assessment (including nutrition, BMI and physical activity).31 From this report card, the child selected a goal to work on over the next six months, and children with a BMI greater than the 85th percentile were given a medical referral. The authors reported the HWI was well-accepted by clinicians and caregivers, with nearly all caregivers instituting dietary changes to help their children meet their goals.31
ORAL HEALTH PROFESSIONALS’ ROLE
Based on policies from the American Dental Association, American Dental Hygienists’ Association and American Academy of Pediatric Dentistry, nutritional counseling on healthy eating to reduce risk for caries and improve overall health is a component of preventive services.30 The overall role is to support healthy behaviors, rather than a focus on weight loss. Because weight loss is not always appropriate for children (it could impair growth), oral health professionals should focus on modifiable risk factors and support healthy behaviors, including:32
- Providing nutritional education for parents/caregivers and children
- Reducing sources of added sugars to aid in reducing caries risk and weight gain
- Following guidelines from the American Academy of Pediatrics on juice consumption, which suggest the following limits:14,33
— Ages 1 to 3: 4 ounces daily
— Ages 4 to 6 years: 4 to 6 ounces daily
— Ages 7 to 18: 8 ounces or 1 cup daily
- Consuming a diet high in fruits and vegetables
- Choosing whole grains
- Focusing on lean protein and low-fat milk
- Being active for at least 60 minutes per day
- Providing referrals to a primary care provider and/or registered dietitian when appropriate (e.g., if BMI screening indicates the child is overweight/obese, or the oral health professional believes there are concerns beyond their scope of practice)
Approaches to making healthy diet choices are available at choosemyplate.gov.32 Resources are available in English and Spanish and include games, activity sheets, videos and resources for parents/caregivers. In dental offices, the videos could be played during the child’s appointment. Resources could be posted to websites hosted by the practice or printed and provided to children. Other resources for parents/caregivers include recipes, cookbooks, snack tips, and recommendations to cut back on sweets, make better beverage choices, and more. The Academy of Nutrition and Dietetics (eatright.org/for-kids) also offers free resources designed to support a healthy weight.
CONCLUSION
Regardless of the causes of childhood obesity, it is a growing health concern and dental teams are well positioned to provide screening and education based on individual risk factors. On a clinical level, programs such as the HWI could be implemented and tailored to a specific practice or population. If clinicians are unable to move beyond perceived barriers, many of the tools outlined in this article could be presented as an educational handout. Taking small steps to include nutritional counseling in settings that are not already doing so may improve clinician comfort with the subject and open doors to more specific interventions in the future. At the very least, clinicians should educate their patients and parents/caregivers about current dietary guidelines, particularly those related to sugar intake.
Research has demonstrated the need for more specific education and training for dentists and dental hygienists in the area of childhood obesity and intervention.16,23 Oral health professionals should seek to become part of an interprofessional approach to this health crisis, taking action not only on the clinical, but also community level.22,25 For example, dental providers could serve on multidisciplinary teams working with community stakeholders to improve access to healthier foods choices in schools, remove SSBs from school meals and events, and create early intervention or wellness programs. Additionally, dental teams can act as advocates and influence public policy on a local, national or global level by working toward professional curriculum changes, supporting legislative changes to reduce consumption of SSBs, and advocating for regulations to improve access to healthier foods.
REFERENCES
- U.S. Centers for Disease Control and Prevention. Childhood Obesity Facts. Available at: cdc.gov/obesity/data/childhood.html. Accessed March 4, 2020.
- World Health Organization. Facts and figures on childhood obesity. Available at: who.int/end-childhood-obesity/facts/en/. Accessed March 4, 2020.
- National Academies of Sciences, Medicine. Obesity in the Early Childhood Years: State of the Science and Implementation of Promising Solutions: Workshop Summary (2016). Available at: nap.edu/catalog/23445/obesity-in-the-early-childhood-years-state-of-the-science. Accessed March 4, 2020.
- Kumar S, Kelly AS. Review of childhood obesity: From epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc. 2017;92:251–265.
- U.S. Centers for Disease Control and Prevention. Childhood Obesity Causes and Consequences. Available at: cdc.gov/obesity/childhood/causes.html. Accessed March 4, 2020.
- Vargas CM, Stines EM, Granado HS. Health-equity issues related to childhood obesity: A scoping review. J Public Health Dent. 2017;77:S32–S42.
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: Causes and consequences. J Fam Med Prim Care. 2015;4:187–192.
- Wells JCK, Fewtrell MS. Measuring body composition. Arch Dis Child. 2006;91:612–617.
- U.S. Centers for Disease Control and Prevention: About Child and Teen BMI. Available at: cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Accessed March 4, 2020.
- U.S. Centers for Disease Control and Prevention. Defining Childhood Obesity. Available at: cdc.gov/obesity/childhood/defining.html. Accessed March 4, 2020.
- National Health and Nutrition Examination Survey. NCHS Fact Sheet. Available at: cdc.gov/nchs/data/factsheets/factsheet_nhanes.htm. Accessed March 4, 2020.
- State of Childhood Obesity. Childhood Obesity Trends. Available at: stateofobesity.org/childhood-obesity-trends/. Accessed March 4, 2020.
- Chi DL, Luu M, Chu F. A scoping review of epidemiologic risk factors for pediatric obesity: Implications for future childhood obesity and dental caries prevention research. J Public Health Dent. 2017;77:S8–S31.
- American Academy of Pediatric Dentistry. Policy on Dietary Recommendations for Infants, Children, and Adolescents. Available at: aapd.org/research/oral-health-policies–recommendations/dietary-recommendations-for-infants-children-and-adolescents/. Accessed March 4, 2020.
- Frantsve-Hawley J, Bader JD, Welsh JA, Wright JT. A systematic review of the association between consumption of sugar-containing beverages and excess weight gain among children under age 12. J Public Health Dent. 2017;77:S43–S66.
- Costacurta M, DiRenzo L, Sicuro L, Gratteri S, De Lorenzo A, Docimo R. Dental caries and childhood obesity: Analysis of food intakes, lifestyle. Eur J Paediatr Dent. 2014;15:343–348.
- Alm A, Fåhraeus C, Wendt LK, Koch G, Andersson-Gäre B, Birkhed D. Body adiposity status in teenagers and snacking habits in early childhood in relation to approximal caries at 15 years of age. Int J Paediatr Dent. 2008;18:189–196.
- Hayden C, Bowler JO, Chambers S, et al. Obesity and dental caries in children: A systematic review and meta-analysis. Community Dent Oral Epidemiol. 2013;41:289–308.
- Garcia RI, Kleinman D, Holt K, et al. Healthy futures: engaging the oral health community in childhood obesity prevention — conference summary and recommendations. J Public Health Dent. 2017;77:S136–S140.
- Hilgers KK, Akridge M, Scheetz JP, Kinane DF. Childhood obesity and dental development. Pediatr Dent. 2006;28:18–22.
- Martens L, De Smet S, Yusof MYPM, Rajasekharan S. Association between overweight/obesity and periodontal disease in children and adolescents: A systematic review and meta-analysis. Eur Arch Paediatr Dent. 2017;18:69–82.
- Narang I, Mathew JL. Childhood obesity and obstructive sleep apnea. J Nutr Metab. 2012;2012:134202.
- Tinanoff N, Holt K. Introduction to proceedings of healthy futures: engaging the oral health community in childhood obesity prevention national conference. J Public Health Dent. 2017;77:S5–S7.
- American Heart Association. Sugar Recommendation Healthy Kids and Teens Infographic. Available at: https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/sugar/sugar-recommendation-healthy-kids-and-teens-infographic. Accessed March 4, 2020.
- World Health Organization. Healthy Diet. Available at: who.int/news-room/fact-sheets/detail/healthy-diet. Accessed March 4, 2020.
- Cole DD, Boyd LD, Vineyard J, Giblin-Scanlon LJ. Childhood obesity: dental hygienists’ beliefs attitudes and barriers to patient education. J Dent Hyg. 2018;92:38–49.
- Greenberg BL, Glick M, Tavares M. Addressing obesity in the dental setting: What can be learned from oral health care professionals’ efforts to screen for medical conditions. J Public Health Dent. 2017;77:S67–S78.
- Wright R, Casamassimo PS. Assessing attitudes and actions of pediatric dentists toward childhood obesity and sugar-sweetened beverages. J Public Health Dent. 2017;77:S79–S87.
- Divaris K, Bhaskar V, McGraw KA. Pediatric obesity-related curricular content and training in dental schools and dental hygiene programs: systematic review and recommendations. J Public Health Dent. 2017;77:S96–S103.
- American Dental Hygienists’ Association. Policy Manual. Available at: adha.org/resources-docs/7614_Policy_Manual.pdf. Accessed March 4, 2020.
- Tavares M, Chomitz V. A healthy weight intervention for children in a dental setting: a pilot study. J Am Dent Assoc. 2009;140:313–316.
- U.S Department of Agriculture. ChooseMyPlate: Become a MyPlate Champion. Available at: choosemyplate.gov/kids-become-myplate-champion. Accessed March 4, 2020.
- Heyman MB, Abrams SA. Fruit juice in infants, children, and adolescents: current recommendations. Pediatrics. 2017;139:e20170967.
From Decisions in Dentistry. April 2020;6(4):38–41.