Oral Care for Patients With Type 2 Diabetes
An examination of the pathophysiology and characteristics of Type 2 diabetes mellitus, as well as its systemic and oral health manifestations.
This course was published in the May 2023 issue and expires May 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the prevalence and risk factors for type 2 diabetes mellitus (T2DM).
- Explain treatment options for T2DM.
- Identify the oral manifestations of this metabolic disorder, as well as patient management strategies in the dental setting.
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder and leading health concern in the United States due to its growing prevalence and associated health issues.1 Diabetes can cause complications throughout the body, including the oral cavity.2–4 In order to provide optimal care, dental professionals should be knowledgeable about T2DM’s pathophysiology, characteristics, and systemic and oral health manifestations, as this understanding will help shape management strategies when treating this patient cohort.
In health, beta cells in the pancreas produce insulin, which allows glucose uptake by the cells. From a pathophysiological perspective, T2DM is characterized by the inability to appropriately use insulin (insulin resistance), and the compromised ability of pancreatic beta cells to secrete enough insulin, leading to elevated blood glucose (hyperglycemia).5 The hormone insulin is responsible for using glucose to produce energy in cells and glucose conversion into glycogen for storage.5,6 Adipose tissue also contributes to insulin resistance.3,5
Accounting for 90% to 95% of all diabetes cases, T2DM is influenced by age, race, ethnicity, socioeconomic status, diet, and physical activity level.5–7 In the United States, 34.1 million or 13% of adults age 18 and older have diabetes, with approximately 7.3 million or 2.8% remaining undiagnosed.7 The prevalence of diabetes increases with age. An additional 88 million adults are prediabetic, which is a risk factor for developing T2DM.7
Genetic factors — such as ethnicity, family history and genetic predispositions — may influence the likelihood of developing T2DM; however, studies show a strong correlation between improvements of modifiable risk factors and disease prevention.5 Environmental factors, such as a sedentary lifestyle, reduced sleep, obstructive sleep apnea, endocrine disruptors, and the gut microbiota, also correlate with diabetes risk.6 Risk factors for developing T2DM include low amounts of physical activity, increased body mass index, smoking, a history of gestational diabetes or other metabolic disorders, hypertension, systemic inflammation, and older age.8
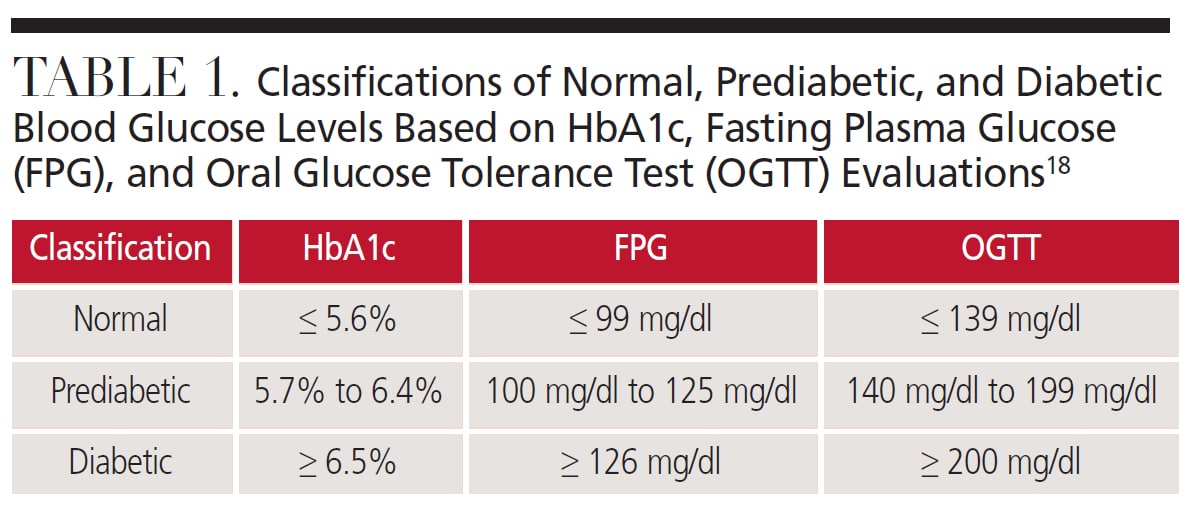
DIAGNOSIS AND CHARACTERISTICS
The diagnosis of T2DM requires a blood test (Table 1). The hemoglobin A1C (HbA1c) test measures the average blood glucose level over the past two to three months; a result of 6.5% or higher indicates diabetes. The fasting plasma glucose test requires eight hours of fasting; a result of 126 mg/dl or higher indicates diabetes.
Hyperglycemia causes narrowing of blood vessels, impeding blood flow and damaging organs, such as the eyes and kidneys, as well as the integumentary, nervous, circulatory and immune systems.2,5 Chronic high blood glucose can lead to an impaired immune system. Common symptoms of T2DM include polyuria (increased urination), polyphagia (increased hunger), and polydipsia (excessive thirst). Other symptoms include weight loss, fatigue, recurrent infections, and dark patches on the skin of the neck, underarms and groin.9
Compared to healthy individuals, patients with T2DM are at higher risk for developing kidney disease and cardiovascular disease, including myocardial infarction, stroke, hypertension and atherosclerosis.1–3,5,10,11
This patient cohort is also more likely to experience hearing impairment and diabetic retinopathy.11–13 Hearing impairment may be caused by hyperglycemia, which weakens the nerves and blood vessels in the inner ear. Diabetic retinopathy is the most common complication of diabetes13 and occurs when hyperglycemia causes blood vessels in the retina to expand and discharge fluid into the eye. Eventually, the retina can detach from the underlying tissue, causing blindness.
Skin complications may be the first sign of diabetes, including diabetic dermopathy (small lesions and spots on bony parts of the body), necrobiosis lipoidica diabeticorum (skin rashes that mostly affect the shin area in women), diabetic blisters, eruptive xanthomatosis (small yellow-red raised lesions anywhere on the body), and bacterial and fungal infections.14
Nerve damage, or neuropathy, is another complication of T2DM; it can occur anywhere in the body, but frequently impacts the feet.11,15,16 In addition to poor circulation, neuropathy in the feet may raise the risk of infection and ulcerations — and, in severe cases, may lead to amputation.15,16
TREATMENT
Treatment of T2DM involves managing blood glucose levels, which is typically done with medications, routine blood glucose monitoring, and changes in diet and physical activity.17 Patients should self-monitor blood glucose regularly and have their HbA1c levels checked every three to six months. For those taking insulin, self-monitoring of blood glucose may be needed several times a day. Additionally, people with diabetes should aim for an HbA1c of less than 7%.18
Patient education can help with medication and treatment compliance. In general, patients with T2DM should practice good oral and skin hygiene, use stress management strategies, eat a balanced diet, exercise regularly, avoid smoking, monitor blood glucose regularly, and keep routine visits with an endocrinologist. Although there is currently no cure for T2DM, pharmacological therapies can effectively help manage the disease.17
Metformin is the primary medication used to manage T2DM. It works by reducing the amount of glucose the body produces and helping move glucose from the blood into cells.17 For more advanced T2DM, an insulin pump may be necessary. While insulin pumps were first introduced to treat Type 1 diabetes, they are also used for patients with T2DM. Insulin pumps can deliver continuous amounts of insulin throughout the day to better regulate blood glucose levels.19 Additionally, bariatric surgeries may be recommended for patients with T2DM if they have a body mass index of 35 or more.20,21
ORAL MANIFESTATIONS
Diabetes often causes oral manifestations, which can be challenging to manage (Table 2). Routine preventive oral hygiene services are particularly important for patients with T2DM. Xerostomia is a common oral complication of T2DM.4 This association may be related to changes in the salivary glands leading to decreased salivary flow or a side effect of medication prescribed for diabetes. While the range is quite broad, studies show that 4% to 51% of individuals with diabetes report xerostomia.22–27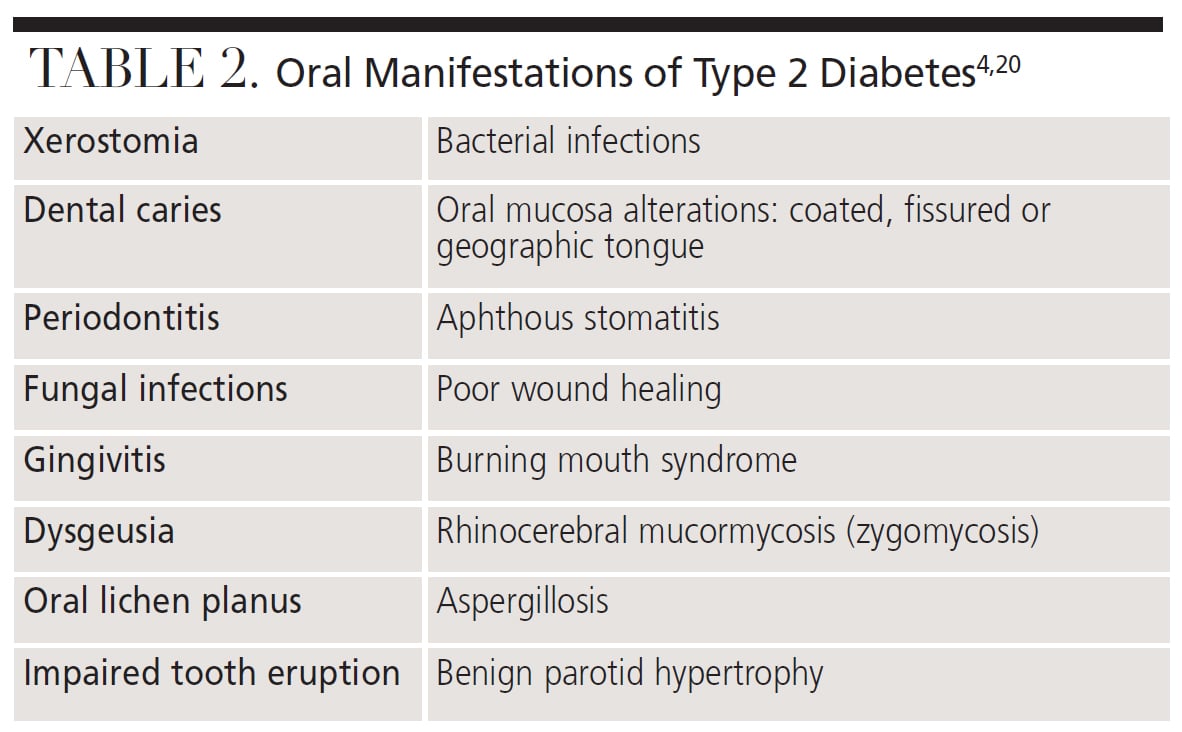
Dental caries risk is also increased among patients with T2DM.22,28,29 One study found those with diabetes had lower mean salivary pH compared to subjects without diabetes (4.83 versus 5.90) and lower mean salivary calcium levels than people without diabetes (0.74 mmol/L versus 5.58 mmol/L). These lower levels create a more conducive environment for demineralization and caries formation.29
Fungal infections, such as oral candidiasis, are another common oral manifestation of T2DM due to reduced salivary flow, hyperglycemia, and impaired immune function. Other risk factors for fungal infections include smoking, wearing dentures, and HbA1c levels more than 12%.30 Studies show between 2% and 24.3% of patients with T2DM experience oral candidiasis.26,27,31
Diabetes and periodontitis are both chronic inflammatory diseases with a bidirectional relationship.32 Studies show between 45.3% and 58% of patients with T2DM develop periodontitis.24–26 Blood glucose levels influence the severity of periodontitis and periodontal therapies have shown short-term improvements in patients’ HbA1c levels.22,32,33 Poor glycemic control is correlated with the development and progression of periodontal disease.22,32 In addition, periodontitis and diabetes share common risk factors, such as older age, male gender, minority race/ethnicity, low socioeconomic status, genetic predisposition, smoking, obesity, low activity level, and poor diet.32
PATIENT MANAGEMENT
Assessment is the first step in effective management of individuals with T2DM and it begins as soon as patients enter the dental office. A patient who is limping may be experiencing neuropathy or a skin/foot complication. Alternatively, a patient wearing open footwear may display obvious signs of infection on his or her feet. Due to the millions of people with undiagnosed diabetes, it is important for oral health professionals to assess for diabetes risk factors. Specifically, dental teams can perform chairside HbA1c testing to screen for T2DM and, if diabetes is suspected, refer patients to their primary care physician for a definitive diagnosis.
An interdisciplinary approach to T2DM will help clinicians create comprehensive treatment plans that meet patients’ systemic and oral health needs. Prophylactic antibiotics for routine dental procedures are not typically recommended when diabetes is the only risk factor.34 However, for patients with uncontrolled diabetes, medical clearance from the patient’s endocrinologist or primary care provider may be prudent prior to dental care.35
The patient’s medical history should be updated at every appointment. This should document whether the patient recently ate, and also note the individual’s current blood glucose level, latest HbA1c number, and medication usage — along with an assessment of the oral implications of the drug regimen. The most accurate way to measure blood glucose control is with an HbA1c test.34 Due to the strong association between diabetes and cardiovascular disease, including hypertension, blood pressure should be documented in the medical history at every visit for patients with T2DM.
Oral health professionals should be cognizant of extraoral and intraoral manifestations of T2DM, such as dark patches of skin on the neck, oral lichen planus, fissured tongue, geographic tongue, aphthous stomatitis, oral candidiasis and xerostomia. If the patient has oral candidiasis, antifungal medications, such as nystatin, miconazole or oral fluconazole, may be prescribed.36 If a mucosal infection is evident, the patient’s primary care physician should be consulted to see if it is related to blood glucose levels. If the oral mucosa or tongue appear dry or the patient reports xerostomia, he or she should be advised to avoid smoking and alcohol, stay hydrated, utilize saliva substitutes and products that contain fluoride and xylitol, and consider prescription medications.
Due to the high caries risk in patients with T2DM, education on biofilm control is imperative. Fluoride varnish should be considered for this patient population, perhaps as frequently as every three to six months. Prescription-strength fluoride products might also be recommended.37 Discussing how biofilm and fermentable carbohydrates contribute to caries risk is important for patient compliance. Referring patients to a registered dietitian for nutritional therapy may be beneficial for improving the patient’s HbA1c number.38 In fact, a systematic review of the literature showed that individuals with T2DM who apply healthy behavior interventions recommended by a registered dietitian improved their glycemic control.37
Uncontrolled diabetes can result in higher rates of alveolar bone destruction, soft tissue destruction and tooth loss. Similarly, periodontitis is correlated to higher blood glucose levels and an increase in incidence of T2DM.39 In 2017, a new classification system for periodontal disease was developed to include a system for staging and grading a patient with periodontitis. The grading component is intended to assess the rate of disease progression, the patient’s ability to respond appropriately to therapy, and the potential impact on overall health. Periodontitis grading is dependent on the amount of radiographic bone loss or clinical attachment loss, percent of bone loss divided by age, and amount of biofilm present. Grade modifiers are risk factors, such as cigarette smoking and diabetes that affect the rate of progression. Grades consist of Grade A: slow rate; Grade B: moderate rate; and Grade C: rapid rate.40
All patients with T2DM and periodontitis are initially a Grade B. Patients with diabetes and an HbA1c under 7% will remain at Grade B if no factors related to Grade C are present; however, an HbA1c of 7% or higher may result in a Grade C classification.38 Affected individuals should be educated on how their HbA1c could impact future attachment loss and response to periodontal therapy. Additionally, invasive procedures, such as periodontal scaling and root planing, should be planned carefully due to T2DM impacting the immune system and impairing wound healing. Individuals with diabetes may need more frequent recare appointments, especially if they have periodontitis.
Patients with diabetes should have dental appointments in the morning, after they normally eat breakfast and take their medications. However, patients may not eat prior to their dental appointment and unintentionally administer too much insulin, resulting in a hypoglycemic incident (i.e., a blood glucose concentration < 70 mg/dl) with rapid progression and little forewarning. The patient may exhibit signs and symptoms, including cold, clammy skin, nausea, irregular speech patterns, tachycardia and confusion. If not addressed immediately, the patient’s blood pressure can drop, resulting in unconsciousness, seizures, and even death. Administration of any high-sugar-containing food or beverage, such as fruit juices or candy, can help. If the patient does not improve within minutes, emergency medical services should be contacted.34,41
CONCLUSION
As noted at the outset, T2DM is a chronic metabolic disorder that impacts the entire body. Common oral manifestations include xerostomia, caries, oral candidiasis and periodontal disease. Oral health professionals should be prepared to recognize the intraoral and extraoral signs and symptoms of T2DM, and, using an interdisciplinary approach, respond with appropriate patient management strategies and oral self-care recommendations.
REFERENCES
- Schmidt A. Highlighting diabetes mellitus: the epidemic continues. Arterioscler Thromb Vasc Biol. 2018;38:e1–e8.
- Leite R, Marlow N, Fernandes J. Oral health and type 2 diabetes. Am J Med Sci. 2013;345:271–273.
- Kanter JE, Bornfeldt KE. Impact of diabetes mellitus. Arterioscler Thromb Vasc Biol. 2016;36:1049–1053.
- Mauri-Obradors E, Estrugo-Devesa A, Jané-Salas E, Viñas M, López-López J. Oral manifestations of diabetes mellitus. A systematic review. Med Oral Patol Oral Cir Bucal. 2017;22:e586–e594.
- Galicia-Garcia U, Benito-Vicente A, Jebari S, et al. Pathophysiology of type 2 diabetes mellitus. Int J Mol Sci. 2020;21:6275.
- Skyler JS, Bakris GL, Bonifacio E, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. 2017;66:241–255.
- U.S. Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020. Available at: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed April 6, 2023.
- Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13:e0194127.
- Ramachandran A. Know the signs and symptoms of diabetes. Indian J Med Res. 2014;140:579–581.
- Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol. 2018;17:57.
- Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013;93:137–188.
- Samocha-Bonet D, Wu B, Ryugo DK. Diabetes mellitus and hearing loss: a review. Ageing Res Rev. 2021;71:101423.
- Simó-Servat O, Hernández C, Simó R. Diabetic retinopathy in the context of patients with diabetes. Ophthalmic Res. 2019;62:211–217.
- Sanches MM, Roda Â, Pimenta R, Filipe PL, Freitas JP. Cutaneous manifestations of diabetes mellitus and prediabetes. Acta Med Port. 2019;32:459–465.
- Dong J, Chen L, Zhang Y, et al. Mast cells in diabetes and diabetic wound healing. Adv Ther. 2020;37:4519–4537.
- Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep. 2019;19:86.
- Artasensi A, Pedretti A, Vistoli G, Fumagalli L. Type 2 diabetes mellitus: a review of multi-target drugs. Molecules. 2020;25:1987.
- American Diabetes Association. Understanding A1C. Available at: https://diabetes.org/ diabetes/a1c. Accessed April 6, 2023.
- Landau Z, Raz I, Wainstein J, Bar-Dayan Y, Cahn A. The role of insulin pump therapy for type 2 diabetes mellitus. Diabetes Metab Res Rev. 2017;33:1002.
- Celio AC, Pories WJ. A history of bariatric surgery: the maturation of a medical discipline. Surg Clin North Am. 2016;96:655–667.
- Affinati AH, Esfandiari NH, Oral EA, Kraftson AT. Bariatric surgery in the treatment of type 2 diabetes. Curr Diab Rep. 2019;19:156.
- Rohani B. Oral manifestations in patients with diabetes mellitus. World J Diabetes. 2019;10:485–489.
- Lessa LS, Pires PD, Ceretta RA, et al. Meta-analysis of prevalence of xerostomia in diabetes mellitus. Int Arch Med. 2015;8:1–13.
- Choudhary A, Sharma H, Choudhary H. Prevalence of oral manifestations in diabetic patients. Int J Community Health Med Res. 2019;5:89–91.
- Kathiresan TS, Masthan KMK, Sarangarajan R, Babu A, Kumar P. A study of diabetes associated oral manifestations. J Pharm Bioallied Sci. 2017;9(Suppl 1):S211–S216.
- Ghadiri-Anari A, Kheirollahi K, Hazar N, et al. Frequency of oral manifestations in diabetic patients in Yazd 2016–2017. Iranian J Diabetes Obesity. 2020;12(2):63–68.
- Bangash RY, Khan AU, Tariq KH, Yousaf A. Oral aspects and complications in type 2 diabetes mellitus: a study. Pakistan Oral Dent J. 2012;32(2):296–299.
- Singh I, Singh P, Singh A, Singh T, Kour R. Diabetes an inducing factor for dental caries: a case control analysis in Jammu. J Int Soc Prev Community Dent. 2016;6:125–129.
- Singh A, Thomas S, Dagli RJ, Kaţ R, Solanki J, Bhateja GA. To access the effects of salivary factors on dental caries among diabetic patients and non diabetic patients in Jodhpur City. J Adv Oral Res. 2014;5:10–14.
- Ahmad P, Akhtar U, Chaudhry A, Rahid U, Sail S, Asil JA. Repercussion of diabetes mellitus on the oral cavity. Eur J Gen Dent. 2019;8:55–62.
- Moosa Y, Shahzad M, Shaikh AA, Matloob SA, Khalid AM. Influence of diabetes mellitus on oral health. Pakistan Oral Dent J. 2018;38(1):67–70.
- Kocher T, König J, Borgnakke WS, Pink C, Meisel P. Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontol 2000. 2018;78:59–97.
- Sanz M, Ceriello A, Buysschaert M, et al. Scientific evidence on the links between periodontal diseases and diabetes: Consensus report and guidelines of the Joint Workshop on Periodontal Diseases and Diabetes by the International Diabetes Federation and the European Federation of Periodontology. J Clin Periodontol. 2018;45:138–149.
- Haveles EB. Applied Pharmacology for the Dental Hygienist. 7th ed. St. Louis: Elsevier Mosby; 2016.
- Miller A, Ouanounou A. Diagnosis, management, and dental considerations for the diabetic patient. J Can Dent Assoc. 2020;86:k8.
- Quindós G, Gil-Alonso S, Marcos-Arias C, et al. Therapeutic tools for oral candidiasis: current and new antifungal drugs. Med Oral Patol Oral Cir Buccal. 2019;24:e172–e180.
- Weyant RJ, Tracy SL, Anselmo TT, et al. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2013;144:1279–1291.
- Dobrow L, Estrada I, Burkholder-Cooley N, Miklavcic J. Potential effectiveness of registered dietitian nutritionists in healthy behavior interventions for managing type 2 diabetes in older adults: a systematic review. Front Nutr. 2022;8:737410.
- Barutta F, Bellini S, Durazzo M, Gruden G. Novel insight into the mechanisms of the bidirectional relationship between diabetes and periodontitis. Biomedicines. 2022;10:178.
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–S172.
- Grimes EB. Medical Emergencies: Essentials for the Dental Professional. 2nd ed. London: Pearson; 2014.
From Decisions in Dentistry. May 2023;9(5):40-43.