RAWPIXEL / ISTOCK / GETTY IMAGES PLUS
RAWPIXEL / ISTOCK / GETTY IMAGES PLUS
Interprofessional Approach to Xerostomia Treatment
Collaboration is key when managing this common oral health condition.
This course was published in the May 2023 issue and expires May 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the prevalence of xerostomia, along with considerations related to behavioral health that contribute to this condition.
- Explain the role of medications in xerostomia, as well as strategies for managing drug regimens for affected patients.
- Discuss oral healthcare considerations and the need for interprofessional collaboration when treating patients with dry mouth.
Affecting upwards of 29% of patients, xerostomia, or the subjective feeling of dry mouth, is associated with a variety of etiologies.1–3 Oral health professionals are at the forefront of care for patients with xerostomia and all clinical staff members should be knowledgeable of common signs, symptoms and management. While dental providers play a key role in identifying and treating xerostomia, nondental factors may also be related. Thus, an interprofessional approach involving the patient’s extended healthcare team can optimize care and address the potential behavioral and systemic components related to xerostomia.
Behavioral health factors, such as stress, depression and anxiety, play a significant role in xerostomia, specifically through the decrease of salivary flow rates and increase of subjective oral dryness.4,5 Approximately 50 million Americans experienced a mental illness prior to the COVID-19 pandemic.6 Mood disorders directly affect the subjective feelings of dry mouth by stimulating anticholinergic mechanisms and impacting the autonomic nervous system (ANS).2,7 Additionally, high stress levels increase salivary cortisol levels, creating changes in the composition of saliva.7 Patients with psychiatric disorders also show higher rates of xerostomia when compared to the general population.8
Patients with xerostomia and high stress levels and/or mental health conditions face additional challenges when working with oral health professionals to identify the most appropriate treatment plan. Many patients find that though psychotropic medications are effective treatments for mental health conditions, they contribute to subjective dry mouth and decreased salivary flow rates.5 The rates of mental health conditions and stress co-occurring with substance misuse continue to grow.9 Substance use at any level is strongly associated with xerostomia, including drug, alcohol and tobacco use.10–15 Though e-cigarettes are growing in popularity, there is no current evidence suggesting an association with xerostomia.11
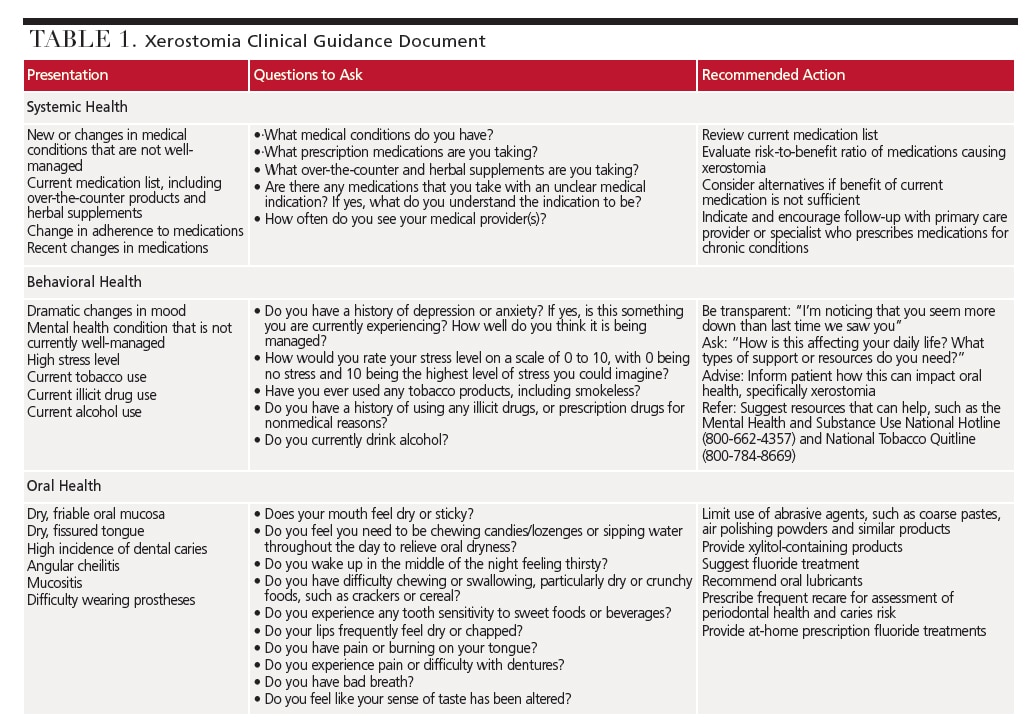
Associations between behavioral health factors and xerostomia underscore the importance of consistently addressing a patient’s oral health in a person-centered way in order to identify all factors impacting oral health. This process should include the use of screening questions at every visit to assess for stress, mental health conditions, and substance use. Gathering a comprehensive understanding of a patient’s medical and social history is essential to providing appropriate care. Table 1 provides signs and symptoms to look for in patients, as well as questions to consider asking in order to initiate conversations about behavioral health concerns.16,17
PHARMACOLOGICAL EFFECTS
A significant factor to consider in xerostomia is the patient’s medication usage.3 Older adults tend to experience xerostomia more frequently than the general population due to the higher likelihood of taking multiple medications.18,19 Various measures are available to evaluate instances in which a patient experiences dry mouth (e.g., while eating) and to determine salivary flow rate.20–22 A thorough assessment is necessary to determine the degree to which a patient experiences xerostomia.
When evaluating a patient’s medication list, the mechanisms by which certain classes of medications may impact saliva production should be reviewed. While the known mechanisms primarily impact the ANS that stimulates salivary glands, mechanisms can also be due to medications or conditions that impact the central nervous system (CNS).18,19,23–25 The two main mechanisms in the ANS are blocking stimulation of the parasympathetic nerves and mimicking stimulation of the sympathetic nervous system. Both lead to reduced fluid volume and increased viscosity of saliva. Medication classes that block parasympathetic nerve stimulation include anticholinergics, antidepressants, antiemetics, antihistamines, antihypertensives, antimigraine, antiparkinsonian drugs, antipsychotics, anti-epileptics, antispasmodics, muscle relaxants, sedatives and anxiolytics. Amphetamines, appetite suppressants, bronchodilators and decongestants are common sympathomimetics.18,19,23–25
Medications that have mechanisms in the CNS impact neural effects on adrenoreceptors, inhibiting salivary nuclei (opioids, for example). In addition, some medications produce symptoms of dryness without decreasing salivary flow, including inhalers and antihypertensives (specifically diuretics). Lastly, other medications have unique xerostomia-related mechanisms, such as anti-infective agents, antineoplastic/cytotoxic agents, narcotic analgesics, and proton-pump inhibitors.19,23–25
Treatment of xerostomia includes evaluating the medications causing or exacerbating xerostomia, determining the risk-to-benefit ratio, and providing treatment recommendations to soothe symptoms.19,22,26 Interprofessional collaboration between dental professionals and medical providers and pharmacists is essential to address a patient’s chronic dryness. Table 1 suggests ways in which to ask patients specific questions about their medical conditions and medications that may impact oral health; it also lists clinical strategies to help manage xerostomia. Sometimes patients may be switched to an alternative medication that reduces dry mouth symptoms or reduces the additive impact of medications contributing to xerostomia. Even if alternative medications are not possible, adjunctive treatments may help ease symptoms. Mechanical stimulation methods, saliva substitutes/oral lubricants, and prescription medications (pilocarpine and cevimeline) are available.19,26,27
REVIEW OF A CASE PRESENTATION
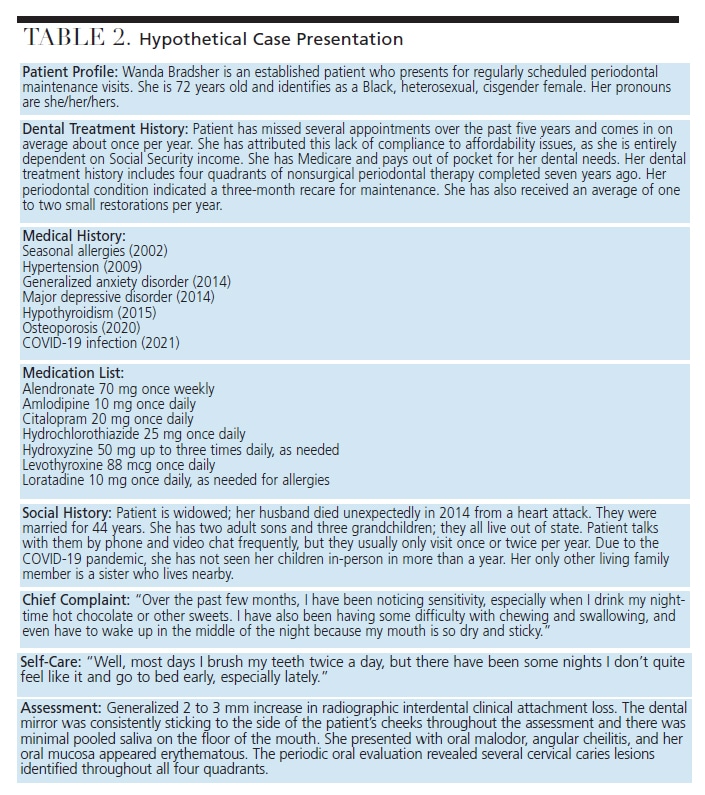
Table 2 presents a hypothetical case about a fictitious patient, Wanda Bradsher. The case explores the patient’s oral health-related factors, assessment findings, and her medical and social histories in support of a holistic approach to care. In reviewing this case, several oral health considerations associated with xerostomia are noted. These are evident in her history of periodontal disease and chief complaint of sensitivity to sweets, difficulty with chewing and swallowing, and the feeling of dryness and stickiness at nighttime.
Although dental team members may be attuned to the oral health manifestations of xerostomia, the nondental aspects of the case should also be considered. Clinicians may use a checklist of questions to evaluate patients from an oral health, behavioral health, and systemic health perspective. Using a checklist can further identify opportunities to collaborate with other healthcare professionals.
From a behavioral health perspective, multiple psychosocial factors that could contribute to the patient’s xerostomia are present. Most notably, the patient has a history of generalized anxiety disorder and major depressive disorder, for which she was diagnosed following the death of her husband nine years ago. She has also experienced a recent increase in social isolation due to the COVID-19 pandemic and lives on a fixed income. The patient is underinsured for dental needs and must pay out of pocket for dental care. She also reports going to bed early more frequently and sometimes neglects her typical self-care routine. Considering the correlation of xerostomia with stress, depression and anxiety, this should be an area of emphasis during the patient history-taking.5
Additionally, an important part of this patient’s xerostomia management would be to explore how the patient manages these various psychosocial factors and connect her with community support to help decrease her stress, anxiety and depression.
Pharmacologically, the most notable factors include the patient’s diagnosis of generalized anxiety disorder and major depressive disorder, for which she is prescribed citalopram and hydroxyzine. Both are antidepressant and anti-anxiety medications that contribute to xerostomia. Additionally, she has hypertension and her thiazide diuretic, hydrochlorothiazide, may impact her fluid status. She takes an antihistamine that contributes to xerostomia. Lastly, the patient has hypothyroidism. While the thyroid hormone supplement does not directly cause xerostomia, if it is not optimized, it could result in uncontrolled hypothyroidism that contributes to symptoms of dryness and xerostomia.23 An important part of the patient’s medication management would be to explore how well the current drug regimen is working, provide recommendations about supplemental products for managing her xerostomia symptoms, and encourage follow-up with her medical providers to explore alternative agents, as warranted.
SUMMARY
As this hypothetical case illustrates, interprofessional considerations should be factored in when providing oral care to patients presenting with xerostomia. While dental practitioners often take the lead in identifying and managing dry mouth, the possibility of nondental aspects contributing to this condition underscores the importance of working closely with the patient’s extended healthcare team.
Adopting an interprofessional approach can optimize care and address the potential behavioral and systemic components related to xerostomia. By collaborating with medical providers and pharmacists, dental team members can identify all factors impacting oral, systemic and mental health. Managing xerostomia through this lens will help support individualized, whole-person-centered care.
REFERENCES
- American Dental Association. Xerostomia (Dry Mouth). Available at: https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/xerostomia. Accessed April 13, 2023.
- Plemons JM, Al-Hashimi I, Marek CL. Managing xerostomia and salivary gland hypofunction: a report of the ADA Council on Scientific Affairs. J Am Dent Assoc. 2014;145:867–873.
- Guggenheimer J, Moore PA. Xerostomia: etiology, recognition, and treatment. J Am Dent Assoc. 2003;134:61–69.
- U.S. Centers for Medicare and Medicaid Services. Behavioral Health. Available at: https://www.cms.gov/outreach-education/american-indianalaska-native/aian-behavioral-health. Accessed April 13, 2023.
- Borahan M, Pekiner F, Atalay T. Evaluation of effects of the psychological factors on saliva. MUSBED. 2012;2:S8–S14.
- Mental Health America. The State of Mental Health in America. Available at: https://mhanational.org/issues/state-mental-health-america. Accessed April 13, 2023.
- Gholami N, Hosseini Sabzvari B, Razzaghi A, Salah S. Effect of stress, anxiety and depression on unstimulated salivary flow rate and xerostomia. J Dent Res Dent Clin Dent Prospects. 2017;11:247–252.
- Veerabhadrappa S, Chandrappa P, Patil S, Roodmal S, Kumarswamy A, Chappi M. Evaluation of xerostomia in different psychological disorders: an observational study. J Clin Diagn Res. 2016;10:ZC24–ZC27.
- Iqbal MN, Levin CJ, Levin FR. Treatment for substance use disorder with co-occurring mental illness. Focus. 2019;17:88–97.
- Arora G, Freeman R. Oral health and addiction: Consequences of substance use. In: el-Guebaly N, Carrà G, Galanter M, Baldacchino AM, eds. Textbook of Addiction Treatment. New York: Springer, Cham; 2020.
- Chaffee B, Halpern-Felsher B, Cheng J. E-cigarette, cannabis and combustible tobacco use: associations with xerostomia among California adolescents. Community Dent Oral Epidemiol. 2021;10:1111.
- Cuberos M, Chatah E, Baquerizo H. Dental management of patients with substance use disorder. Clin Dent Rev. 2020;4:1–8.
- Billings R, Proskin H, Moss M. Xerostomia and associated factors in a community-dwelling adult population. Community Dent Oral Epidemiol. 1996;24:312–316.
- Cassolato S, Turnbull R. Xerostomia: clinical aspects and treatment. Gerodontology. 2003;20:64–77.
- Dyasanoor S, Saddu SC. Association of xerostomia and assessment of salivary flow using modified Schirmer test among smokers and healthy individuals: a preliminary study. J Clin Diagn Res. 2014;8:211–213.
- The Substance Abuse and Mental Health Services Administration. SAMHSA’s National Helpline. Available at: https://www.samhsa.gov/find-help/national-helpline. Accessed April 13, 2023.
- U.S. Centers for Disease Control and Prevention. Smoking and Tobacco Use — National Quitline Data Warehouse. Available at: https://www.cdc.gov/tobacco/quit_smoking/cessation/nqdw/index.htm. Accessed April 13, 2023.
- Thomson WM, Smith MB, Ferguson CA, Moses G. The challenge of medication-induced dry mouth in residential aged care. Pharmacy (Basel). 2021;9:162.
- Gil-Montoya JA, Silvestre FJ, Barrios R, Silvestre-Rangil J. Treatment of xerostomia and hyposalivation in the elderly: a systematic review. Med Oral Patol Oral Cir Bucal. 2016;21:e355–e366.
- Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The xerostomia inventory: a multi-item approach to measuring dry mouth. Community Dent Health. 1999;16:12–17.
- Thomson WM, van der Putten GJ, de Baat C, et al. Shortening the xerostomia inventory. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:322–327.
- Fornari CB, Bergonci D, Stein CB, Agostini BA, Rigo L. Prevalence of xerostomia and its association with systemic diseases and medications in the elderly: a cross-sectional study. Sao Paulo Med J. 2021;139:380–387.
- Tanasiewicz M, Hildebrandt T, Obersztyn I. Xerostomia of various etiologies: a review of the literature. Adv Clin Exp Med. 2016;25:199–206.
- Wolff A, Joshi RK, Ekström J, et al. A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective sialorrhea: a systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R D. 2017;17:1–28.
- Spolarich AE. Medication use and xerostomia. Dimensions of Dental Hygiene. 2005;3(7):22–24.
- Turner MD. Hyposalivation and xerostomia: etiology, complications, and medical management. Dent Clin North Am. 2016;60:435–443.
- Barbe AG. Medication-induced xerostomia and hyposalivation in the elderly: culprits, complications, and management. Drugs Aging. 2018;35:877–885.
From Decisions in Dentistry. May 2023;9(5):34-36, 39.