Managing Patients With CREST Syndrome
An increased risk for oral pathologies in this population means that clinicians must take a proactive approach to help these patients maintain optimum oral health.
This course was published in the April 2016 issue and expires 04/30/19. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Define CREST syndrome.
- Discuss what the current research reflects about etiology, characterizations, diagnosis and treatment of this disease.
- Identify the treatment considerations for patients with CREST syndrome.
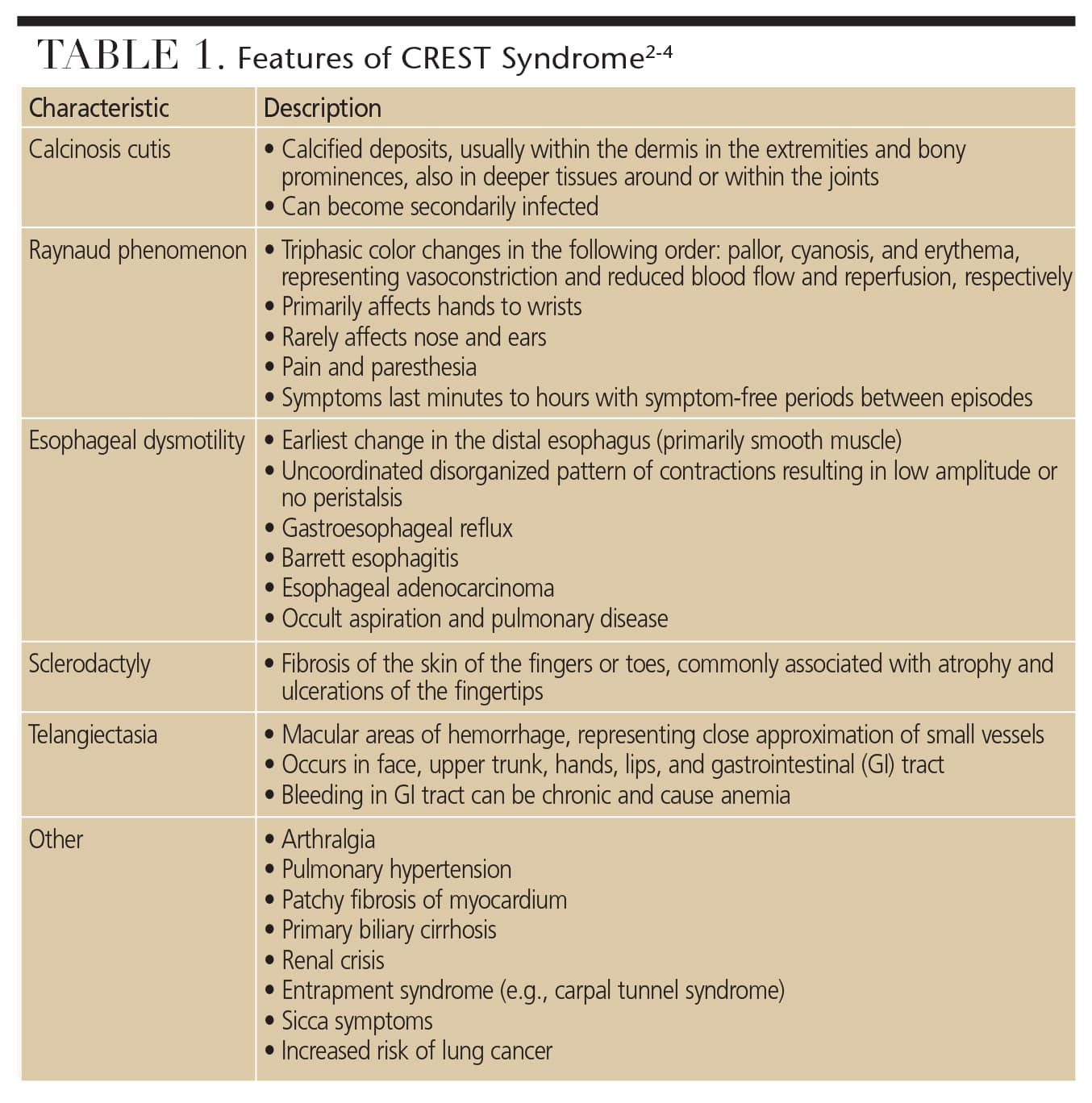
CREST syndrome is an autoimmune disorder that is a localized variant of systemic scleroderma, a chronic connective tissue disease.1,2 It is characterized by the combination of five autoimmune conditions: calcinosis cutis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly and telangiectasia (Table 1).1–4 A slowly progressing disease, CREST syndrome primarily affects middle-aged women, with 55 being the mean age of onset.1,5 Approximately 21 new cases of CREST syndrome are diagnosed per 1 million adults in the United States.6 While there is no known definitive cause of CREST, proposed etiological factors include genetics, exposure to environmental or infectious agents, and graft-versus-host reactions.7
There is controversy in the literature regarding how CREST is diagnosed. According to Lauritano et al, CREST is diagnosed by a blood test and the presentation of any three of the five defined characteristics.3 By comparison, the International Scleroderma Network says it takes presentation of only two of the five symptoms for a CREST diagnosis.8 A new classification system, developed by the American College of Rheumatology and European League Against Rheumatism, has determined that a diagnosis of scleroderma is dependent upon a point system. Various presentations (including the presence of the anticentromere antibody) are assigned a point value, with a score of nine or more classified as scleroderma.9 Anticentromere antibodies are found in approximately 82% to 96% of patients with CREST.4,10 Imaging studies used to aid in the diagnosis of the syndrome include film radiographs (versus digital radiographs), cone beam computed tomography, bone scanning, Doppler ultrasonography, radiologic barium studies, esophageal transit time with fluoroscopy, esophageal manometry and transthoracic echocardiography. These modalities are useful for identifying the extent and progression of the disease.4 Making a differential diagnosis can be difficult because it mimics other conditions, such as mixed connective-tissue disease, amyloidosis, silica exposure, vinyl chloride disease, eosinophilic fasciitis, scleromyxedema, chronic graft-versus-host disease, systemic lupus erythematosus, rheumatoid arthritis, systemic vasculitis and reflex sympathetic dystrophy.4
Regardless of its etiology, CREST is a debilitating and incurable disease that affects the entire body. Survival rates decrease substantially, ranging from 78% at five years to 27% at 20 years.6 The hardening of tissues associated with calcinosis cutis affects the internal organs, leading to serious health complications, such as restrictive lung disease, primary biliary cirrhosis of the liver, and vascular dementia.1–3,11,12 Renal involvement is associated with half of all scleroderma-related deaths in patients with significantly involved skin changes.4 In addition to systemic complications, the head and neck are susceptible to effects of gastroesophageal reflux disease (GERD), vasoconstriction, fibrosis, hemorrhage, limited mouth opening (microstomia), increased incidence of periodontal disease, and xerostomia.1,2 Because CREST manifests in orofacial signs and symptoms, dental professionals are in a unique position to serve this patient population.
LITERATURE REVIEW
CREST syndrome is also identified in the literature as limited cutaneous systemic scleroderma. It is characterized by slow onset and variable presentation, making study of its epidemiological features difficult. Previously, there has been a lack of uniformity in diagnostic criteria. A systematic literature review found that in 50% of cases, Raynaud phenomenon was the first symptom that appeared, and, in many cases, years before diagnosis. Raynaud phenomenon, however, is also common in other connective-tissue diseases, which may explain why some cases of CREST are misdiagnosed. A better diagnostic model for CREST was needed.13
The American College of Rheumatology and European League Against Rheumatism classification criteria for systemic sclerosis have improved sensitivity and specificity, especially among those with early, mild, or limited disease such as CREST.9 The ability to classify CREST at an earlier stage might provide the opportunity to prevent the disease from progressing.9 A recent study investigated how many patients who presented with Raynaud phenomenon and who had not been classified as systemic sclerosis would be reclassified as having scleroderma under the new classification criteria. Investigators found that 26.5% of the patients who presented with Raynaud phenomenon, but who did not fulfill the 1980 American College of Rheumatology classification criteria (n=64), were newly classified with scleroderma. Furthermore, the study showed that sclerodactyly, telangiectasia and the presence of anticentromere antibody had independent predictive value for reclassifying patients with Raynaud phenomenon with scleroderma.14
To improve detection and follow up of patients presenting with different manifestations of this syndrome, an interdisciplinary registry was founded. The registry allows clinicians to document the occurrence of symptoms, age of onset, and the progression of the disease. In compiling these data, researchers hope to provide a large patient base from which to recruit participants for clinical studies. Additionally, there is hope that patients with CREST syndrome overlap, and those in the earliest stages of the disease can be more readily identified.5
TREATING SYMPTOMS
Treatment of CREST has been primarily focused on treating the symptoms associated with each of the five conditions. Fibrosis/calcinosis is irreversible, but the goal of current therapies is to slow disease progression. Medication therapies include D-penicillamine and cyclophosemide, with D-penicillamine showing the most promising results.2 Raynaud phenomenon can be treated with calcium channel blockers (such as nifedipine); prazosin; prosta-glandin derivatives (such as prostaglandin E1); aspirin; and topical nitrates.2,15 The Cochrane Collaboration undertook a meta-analysis to determine the efficacy of prazosin for the treatment of Raynaud phenomenon.16 Prazosin was found to be more effective than a placebo, but the response to the medication was modest and side effects were common. As a symptom of CREST, GERD is managed with antacids, H2 blockers, proton-pump inhibitors, prokinetic agents and laxatives; in addition, consuming small meals may prove beneficial in this patient group.16 In extreme cases, patients with CREST might also benefit from physical therapy or surgery.2 Facial telangiectasia has been treated successfully with pulsed-dye laser treatment, while symptomatic gastrointestinal telangiectasia has been managed with estrogen-progesterone or desmopressin, laser ablation or sclerotherapy.4
While little information specific to CREST is available in the dental literature, a cross-sectional study of patients with systemic scleroderma and gingivitis concluded that dental professionals must take a patient’s manual dexterity into account when providing patient education.17 Available research focuses on the pathogenesis and treatment of CREST, and includes oral manifestations.1,18 Currently, most pharmacological interventions are aimed at suppressing the immune system, dilating blood vessels and increasing blood flow, in addition to treating individual organ problems. The most frequent oral finding to precede systemic involvement appears to be trigeminal neuropathy, followed by enlargement of the periodontal ligament (PDL) space.18 These findings are significant for the dentist, who can refer patients to medical specialists based on oral signs and symptoms.
Due to the numerous vascular, inflammatory and fibrotic changes associated with CREST, these patients are prone to oral disease, and a proactive approach is necessary to prevent complications due to this increased risk for oral pathologies. CREST involves the entire orofacial complex, and a multidisciplinary approach is necessary to ensure that patient needs are met.19
CLINICAL IMPLICATIONS
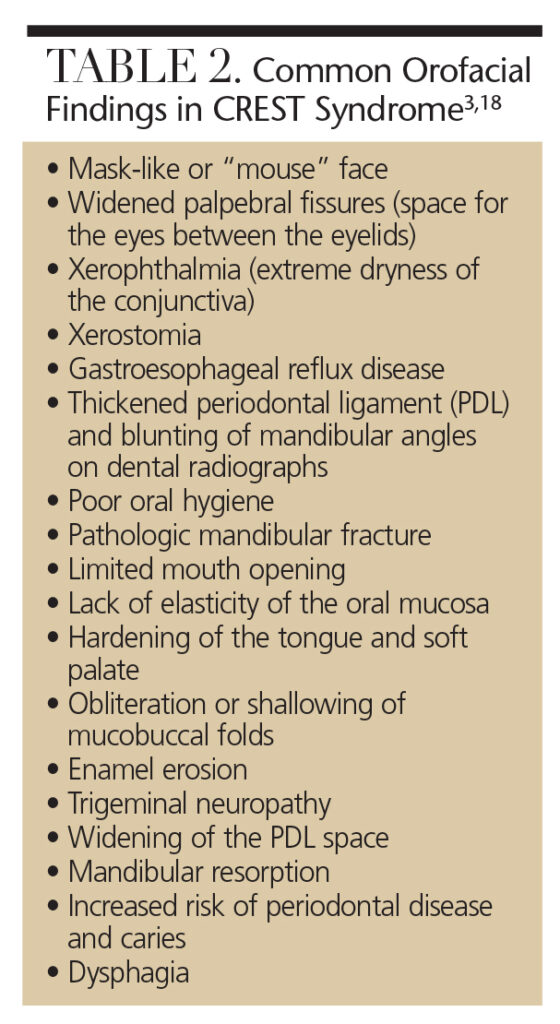 Table 2 provides a list of common orofacial findings in patients with the syndrome. Dental professionals should be alert for signs and symptoms indicative of CREST, and refer patients to a rheumatology specialist for evaluation. Patients might first present with persistent GERD, resulting in acid erosion, dentinal hypersensitivity and mucogingival paresthesia.2,19 Trigeminal neuropathy with no clinical cause is often an early sign of CREST.18 Due to fibrosis of the salivary glands, xerostomia, increased caries risk and candida infections are common in this patient population.20 Xerostomia combined with tongue rigidity, tissue atrophy and bone resorption may make patients with CREST poor candidates for prosthodontics or implants.20
Table 2 provides a list of common orofacial findings in patients with the syndrome. Dental professionals should be alert for signs and symptoms indicative of CREST, and refer patients to a rheumatology specialist for evaluation. Patients might first present with persistent GERD, resulting in acid erosion, dentinal hypersensitivity and mucogingival paresthesia.2,19 Trigeminal neuropathy with no clinical cause is often an early sign of CREST.18 Due to fibrosis of the salivary glands, xerostomia, increased caries risk and candida infections are common in this patient population.20 Xerostomia combined with tongue rigidity, tissue atrophy and bone resorption may make patients with CREST poor candidates for prosthodontics or implants.20
Radiographically, CREST might manifest with generalized widening of the PDL spaces, increased thickening of the lamina dura around posterior teeth, and bone resorption of the angle of the mandible.18,20 Bone resorption is thought to result from the pressure exerted by an increased tightening of the facial structures due to fibrosis, in combination with hypovascularization. This often results in temporomandibular joint (TMJ) pain and dysfunction.18–20 In this instance, the clinician might note crepitus, popping and clicking of the TMJ.20 These manifestations often affect the patient’s ability to chew and swallow effectively.19
The tightening of the skin around the hands and orofacial structures impact oral self-care and movement of oral structures, and also contributes to an increased risk of oral disease.18,21 Due to the loss of elasticity and subsequent microstomia, both self-care and professional care can be challenging.18,21 Fibrotic changes can cause mucosal tissues to appear thin, pale and tight, and tissue hardening may also be evident in the tongue and soft palate.20 Mucosal fibrosis can also cause gingival recession and stripping of the attached gingiva.20 The lack of sufficient self-care, limited mouth opening, and decreased vascularization are implicated in an increased incidence and risk of periodontitis in patients with CREST.19
TREATMENT CONSIDERATIONS
CREST syndrome has many complicating factors, and these patients are at high risk for dental caries, gingivitis and advanced periodontal disease.22 There are practical ways, however, for oral health professionals to successfully treat this population. A two-month or three-month recare interval is essential to stabilize and maintain oral health.18,20 As more than 75% of patients with CREST on a calcium channel blocker regimen develop gingival hyperplasia, dentists need to identify this side effect and refer patients to a periodontist for gingival reduction surgery.15,22,23 Recurrence of gingival hyperplasia is likely as long as patients remain on calcium channel blockers; consequently, dentists should consider consulting with the prescribing physician to determine alternative medications.23 Additionally, regular, thorough oral cancer screenings are of increased importance due to the elevated risk of squamous cell carcinoma of the tongue and pharynx among patients with CREST.18,20
The complications of scleroderma lead to fibrosis and tightening of facial skin, which, in turn, causes microstomia.17,24 Mouth stretching and oral augmentation exercises have been successful in increasing the opening of the oral cavity by 3 mm to 5 mm.20,21 Instructing patients in simple stretching exercises can increase flexibility of the face and mouth.18,21
For the management of xerostomia, pharmaceutical agents, such as pilocarpine and cevimeline, may help stimulate salivary flow.20 Xylitol-containing lozenges or mints and saliva substitutes may improve patient comfort.2,18,20
Caries prevention requires a combination of in-office and at-home fluoride treatments. Limited opening of the oral cavity may make the use of custom trays impossible.18 Fluoride varnish is easily applied with a small brush and can be placed at each recare visit.18,25 Fluoride gels can be brushed on the teeth with a child-size toothbrush and left overnight.18,25 Patients should avoid sugar consumption due to increased caries risk.2,18
The dental operatory can be adjusted to address the needs of patients with CREST. In order to avoid a vascular crisis in patients subject to vasospasms, consider keeping the dental operatory warm.2,18 Providing blankets or gloves will aid in temperature control. A humidifier in the operatory might be helpful as the hydration may ease skin tension.18 Patients should be scheduled in the morning for brief appointments.2,18,20 Nitrous oxide can be used to treat patient anxiety, and oxygen should be available for those with restrictive lung diseases.2
PREVENTIVE OBJECTIVES
Preventing periodontitis is critical for patients with CREST. Biofilm management techniques for self-care must consider limitations caused by symptoms of the disease, and self-care instructions need to be adapted as conditions progress. Mental health status is also a factor to consider when educating patients about oral hygiene techniques, as depression is common in these patients and can affect self-care motivation. When patients exhibit signs of depression, referrals should be made to mental health professionals for further evaluation and treatment.24
Frequent brushing is key for effective biofilm management.24 A small, child-size toothbrush head is recommended due to limited mouth opening, and end-tuft toothbrushes can be utilized in cases of severe microstomia.17,18 Chlorhexidine is also helpful for reducing overall bacterial levels, treating gingival inflammation, and preventing root caries and candida.15 Power toothbrushes and handled interdental aides can help promote biofilm control in patients with limited dexterity.17,18,22,24 In fact, a multifaceted oral health intervention — including use of a power toothbrush, adapted flosser and orofacial exercise — has been shown to be superior to standard self-care devices in improving gingival health.22 Flossing or interdental cleaning in the evening has been shown to decrease gingival inflammation in affected patients.17,24
Specific treatments are contraindicated when performing dental prophylaxis on patients with CREST. Air polishers and ultrasonic scalers should not be used due to the risk of aspiration when fibrosis of the soft palate and dysphagia are present. High-volume suction is mandatory owing to aspiration risks.18 Additionally, four-handed dentistry is recommended for ease of treatment. A dental assistant can aid in the retraction of oral tissues in areas of increased fibrosis. Epinephrine is contraindicated due to limited vascularization, therefore, a 3% local anesthetic solution is recommended.19 Surgical procedures should be avoided when possible due to reduced healing capacity and risk of postoperative complications.20
CONCLUSION
Ultimately, the most important consideration is to understand patients’ limitations and to help them adapt. Dental professionals play an important role by assisting patients in maintaining oral hygiene, identifying oral manifestations, and modifying treatment to ensure effective care.18 As the disease progresses, it may be necessary to initiate routine oral care plans with a caregiver by providing instructions for daily biofilm management and a self-exercise program that facilitates the delivery of preventive care.
As the oral cavity is often an indicator of systemic health, dental professionals are uniquely positioned to note the first signs of CREST syndrome.26 A persistent complaint of GERD, xerostomia, and limited mouth opening may alert practitioners to its possible presence. Effective oral hygiene instruction, along with frequent assessment and periodontal management, are essential to preserve the oral health of patients with CREST syndrome.
References
- Chaffee NR. CREST syndrome: clinical manifestations and dental management. J Prosthodont. 1998;7:155–160.
- Albilia JB, Lam DK, Blanas N, Clokie CM, Sándor GK. Small mouths…big problems? A review of scleroderma and its oral health implications. J Can Dent Assoc. 2007;73:831–838.
- Lauritano D, Bussolati A, Baldoni M, Leonida A. Scleroderma and CREST syndrome: a case report in dentistry. Minerva Stomatol. 2011;60:443–465.
- Yoon JC. CREST syndrome. Available at: emedicine.medscape.com/article/1064663-overview. Accessed February 29, 2016.
- Hunzelmann N, Genth E, Krieg T, et al. The registry of the German Network for Systemic Scleroderma: frequency of disease subsets and patterns of organ involvement. Rheumatology (Oxford). 2008;47:1185–1192.
- Mayes M, Lacey JV Jr, Beebe-Dimmer J, et al. Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large U.S. population. Arthritis Rheum. 2003;48:2246–2255.
- Jimenez SA, Derk CT. Following the molecular pathways toward an understanding of the pathogenesis of systemic sclerosis. Ann Intern Med. 2004;140:37–50.
- International Scleroderma Network. Sclerodactyly and scleroderma. Available at: http://www.sclero.org/scleroderma/symptoms/skin/sclerodactyly/a-to-z.html. Accessed February 29, 2016.
- Johnson, S. R. New ACR EULAR guidelines for systemic sclerosis classification. Current Rheumatology Reports. 2015;17(5):1–8.
- Ganda K. Dentist’s Guide to Medical Conditions and Complications. 2nd ed. Hoboken, New Jersey: John Wiley & Sons; 2013:589–623.
- Ito M, Kojima T, Miyata M, et al. Primary biliary cirrhosis (PBC)-CREST (calcinosis, Raynaud’s phenomenon, esophageal dysfunction, sclerodactyly and telangiectasia) overlap syndrome complicated by Sjögren’s syndrome and arthritis. Intern Med. 1995;34:451–454.
- McNair S, Hategan A, Bourgeois JA, Losier B. Neuropsychiatric symptoms in scleroderma. Psychosomatics. 2013;54:382–386.
- Chifflot H, Fautrel B, Sordet C, Chatelus E, Sibilia J. Incidence and prevalence of systemic sclerosis: a systematic literature review. Semin Arthritis Rheum.2008;37:223–235.
- Park JS, Park MC, Song JJ, Park YB, Lee SK Lee SW. Application of the 2013 ACR/EULAR classification criteria for systemic sclerosis to patients with Raynaud’s phenomenon. Arthritis Res Ther. 2015;17:77.
- Alpert MA, Pressly TA, Mukerji V, et al. Acute and long-term effects of nifedipine on pulmonary and systemic hemodynamics in patients with pulmonary/ hypertension associated with diffuse systemic sclerosis, the CREST syndrome and mixed connective tissue disease. Am J Cardiol. 1991;68:1687–1691.
- Pope J, Fenlon D, Thompson A, et al. Prazosin for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev. 2000;2:CD000956.
- Yuen HK, Weng Y, Reed SG, Summerlin LM, Silver RM. Factors associated with gingival inflammation among adults with systemic sclerosis. Int J Dent Hyg. 2014;12:55–61.
- Tolle SL. Scleroderma: considerations for dental hygienists. Int J Dent Hyg. 2008;6:77–83.
- Alantar A, Cabane J, Hachulla E, et al. Recommendations for the care of oral involvement in patients with systemic sclerosis. Arthritis Care Res (Hoboken). 2011;63:1126–1133.
- Fischer DJ, Patton LL. Scleroderma: oral manifestations and treatment challenges. Spec Care Dentist. 2000;20:240–244.
- Pizzo G, Scardina GA, Messina P. Effects of a nonsurgical exercise program on the decreased mouth opening in patients with systemic scleroderma. Clin Oral Investig. 2003;7:175–178.
- Yuen HK, Weng Y, Bandyopadhyay D, Reed SG, Leite RS, Silver RM. Effect of a multifaceted intervention on gingival health among adults with systemic sclerosis. Clin Exp Rheumatol. 2011;29(2 Suppl 65):S26.
- Fardal O, Lygre H. Management of periodontal disease in patients using calcium channel blockers: Gingival overgrowth, prescribed medications, treatment responses and added treatment costs. J Clin Periodontol. 2015;42:640–646.
- Yuen HK, Hant FN, Hatfield C, Summerlin LM, Smith EA, Silver RM. Factors associated with oral hygiene practices among adults with systemic sclerosis. Int J Dent Hyg. 2014;12:180–186.
- Poulsen S. Fluoride-containing gels, mouth rinses, and varnishes: An update of evidence of efficacy. Eur Arch Paediatr Dent. 2009;10:157–161.
- National Institute of Dental and Craniofacial Research. Oral Health in America: A Report of the Surgeon General. Available at: nidcr.nih.gov/DataStatistics/ SurgeonGeneral/Report/ExecutiveSummary.htm. Accessed February 29, 2016.





I just finished reading your article on ” A case for hospital hygienists “, in RDH, 12/2016.
I agree with you that having one or more hygienists on the staff of an acute hospital and rehabilitation facilities would be and is much needed.
I am RN and a RDH. Got my RN in 1968 and my RDH in 1975. I was a surgical tech. in the Army in the early 60’s.
The reason I went into dental hygiene is that I saw many patients while doing nursing who had terrible oral hygiene and how it was affecting their general health.
So, I educate my clients on the importance of their oral health and how it is associated with their general health and how we even share whats in our months with others. Showing ,via mirror, how to properly use floss and tooth brush; many hygienist only tell their clients to ” do a better job”, but do not actually show them how. Believe me!
I have mentioned the need for hygienists to be in hospital for years, but nothing is ever do about it.