Managing Burnout and Perfectionism in Dentistry
An examination of the signs and symptoms of burnout, the role perfectionism may play, and mitigation strategies for oral health professionals.
This course was published in the May 2021 issue and expires May 2024. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- List trends in burnout affecting healthcare professionals, as well as means for diagnosing workplace burnout.
- Describe concepts and factors associated with perfectionism and burnout in dentistry, and the potential ramifications for clinical practice.
- Discuss strategies for managing stress that can contribute to professional burnout.
Burnout in healthcare is on the rise.1 In 2022, the World Health Organization will embark on the development of evidence-based guidelines on mental well-being and will list burnout in the upcoming revision of the International Classification of Diseases as a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is not classified as a medical condition, however.2
Burnout is a psychological syndrome earmarked by the three components most commonly used to help diagnose burnout in the workplace, including dentistry. Maslach developed the Maslach burnout inventory; easy to administer, it yields reliable and valid information with which to evaluate and diagnose workplace burnout.3 This syndrome is characterized by three dimensions: feelings of energy depletion or exhaustion (emotional exhaustion); increased mental distance from one’s job or feelings of negativism or cynicism related to one’s job (depersonalization); and reduced professional efficacy (reduced personal accomplishment). The fallout from burnout may affect other dental team members, patients, colleagues, friends and family.3
Emotional exhaustion, due to chronic exposure to unmitigated stress, makes clinicians feel emotionally, physically and spiritually drained. This may result in affected individuals not feeling they can effectively give of themselves anymore. Often, they report being worn out, with loss of energy, depletion, debilitation and fatigue.3 This may lead to depersonalization, which is earmarked with negative or inappropriate attitudes, sarcasm and cynicism directed at others. Affected individuals may also experience irritability, loss of idealism and withdrawal.3
Depersonalization and emotional exhaustion are closely associated, and the results may be a dental provider conveying the message that he or she does not care about the patient’s concerns or needs. The term compassion fatigue is associated with burnout because it expresses the fatigue and exhaustion a person can experience when dealing with difficult or unreasonable people. Compassion fatigue has been described as the convergence of secondary traumatic stress and cumulative burnout, a state of physical and mental exhaustion caused by a depleted ability to cope with one’s everyday environment.4 A third aspect of burnout syndrome, reduced personal accomplishment, results in a tendency for people to demonstrate an inability to cope; they may have a negative impression of themselves and dissatisfaction with their work and accomplishments.4 This may lead to job turnover, absenteeism, low morale, insomnia, and increased use of drugs and alcohol, as well as marital and family issues.3 One example would be dentists who experience burnout when they find their skill sets and work attitudes are not compatible with working in corporate dentistry.
POTENTIAL IMPACTS OF THE PANDEMIC
It would be remiss not to mention the impact the COVID-19 pandemic has potentially had on the initiation and progression of burnout in healthcare, specifically, in the first several months of the pandemic. Early evidence is emerging on the impact isolation from patients had on dental practitioners due to the lack of relational (i.e., in-person) contact. Lack of relationships with others, especially the doctor-patient-staff model, may show that providers are experiencing some level of burnout due to a lack of control in practice and the uncertainty of the future of practice and patient contact.5
An unpublished survey of dental professionals in North Carolina between September and November 2020 conducted by the North Carolina Caring Dental Professionals and North Carolina Dental Society (n=842 dentists, n=572 dental hygienist respondents) found that 43.5% of dentists and 38.5% of dental hygienists were fully engaged in their work, per the Maslach burnout inventory. By comparison, 18.8% of dentists and 14.0% of dental hygienists reported professional burnout during this COVID-19 pandemic time frame. The remaining respondents fell somewhere in between, reporting feeling either ineffective, overextended or disengaged.6
Most of the burnout research in healthcare workers has studied physicians, with little research on dentists. The fact that almost one in two U.S. physicians has symptoms of burnout implies the origins of this problem are rooted in the environment and care delivery system, rather than in the personal characteristics of medical professionals.7 Physicians list time constraints, use of electronic health records, and other workplace-related factors as top stressors in medicine. Compared to fully engaged providers, physicians with burnout may be subject to a greater number of medical errors and deliver a lower quality of care — and with higher costs and worse outcomes.8 A 2020 study of U.S. providers suggests that dentist burnout is potentially a key predictor of reporting perceived dental errors.9
The multiple platforms in which dentists deliver oral healthcare in the U.S. (solo, group, specialty, dental service organization, and other models of practice) raise the question: Are the origins of burnout in dentistry rooted in the environment and care delivery system, rather than in the individual characteristics of a few susceptible practitioners?
In a study of three graduate programs in dentistry at the University of Barcelona, it was noted that narcissistic and borderline personality types were most frequently found in individuals who present burnout syndrome. An obsessive-compulsive personality was observed in 75% of the participating dentists. The pattern of unstable and impulsive personality and the need for excessive admiration, which are typical of a narcissistic personality, characterized the dentists susceptible for developing burnout.10
There are six driving forces used to determine areas in the workplace (called areas of worklife scale) that may be contributing to burnout in dental offices. These include unstainable workload, perceived lack of control, insufficient rewards for effort, lack of a supportive community, lack of fairness, and mismatched values and skills.3,11
STRESSORS
Dentists must confront many stressful situations in practice. At the top of the list are time and scheduling issues, patient demands, uncooperative patients, need for high levels of concentration and focus, and team issues.12,13 A study in New Zealand revealed the most commonly reported stressors were treating difficult children (52%), constant time pressure (48%), and maintaining high levels of concentration (43%).12 The strategies most utilized for managing work-related stress included interactions with people (78%), sports (64%), and forgetting about work (59%).12
A study by the American Dental Association (ADA) reports that 86% of dentists claim experiencing one or more of these stressful conditions in any given year. This equates to 60 days/year that dentists are significantly stressed and disengaged at work.13 According to Rada and Johnson-Leong,14 dentists are prone to anxiety disorders, clinical depression and professional burnout due to the way dentists practice and their personality traits. Chronic interpersonal workplace-related stressors have a high correlation with anxiety, depression, musculoskeletal complaints, sleep disorders, memory problems and substance-use disorders, which all can be associated with burnout.14 Dentists experience moderate to severe stress levels at work each day. One study found the moderate to severe stress level characterized 82.7% of dentists surveyed,13 while another study found the number to be approaching 86%.15
The ADA’s 2015 Dentists Well-Being Survey indicated updated data concerning stress levels in the workplace. The majority of dentists (67%) reported they have a moderate level of stress at work.16 Less than one in eight dentists (12%) reported severe stress at work. The level of work stress was about the same for female dentists as male dentists, and for younger dentists versus older dentists. Part-time dentists were more likely to have light stress than full-time dentists. More than one-third of part-time dentists (39%) reported light stress at work, while only 18% of full-time dentists reported light stress. Fewer than 25% of part-time dentists reported they faced severe stress at work.16
While only one in 10 dentists was considered at high risk for alcoholism, nearly one in five (18%) of all practicing dentists felt they should cut down on drinking. Feeling a lack of control at work and being unsatisfied with their dental practices were associated with higher risk for alcoholism.16 More than one in five dentists (22%) was found to have a moderate level of depression, and 4% had a high level of depression. Half of the dentists who scored a high level reported that they have not been diagnosed or have not considered themselves to have depression (Figure 1).16
PRESSURE FROM THE START
Stressors in dentistry are ubiquitous and start early in a clinician’s career. The individual’s ability to recognize the source of stress and respond appropriately are critical to preventing burnout. A 2016 study of 121 new dentists (defined as having graduated from six months to less than five years prior) in India revealed that new dentists are especially vulnerable to stress that may lead to burnout. Factors contributing to burnout were emotional exhaustion (39.27%), frustrations (47.83%), feeling worn out at the end of the workday (46.80%), feeling worn out by the end of the evening (35.05%), exhaustion in the morning at the thought of another day at work (35.05%), feeling that every working hour is tiring (46.80%), and having less energy and time for family and friends (47.83%).17
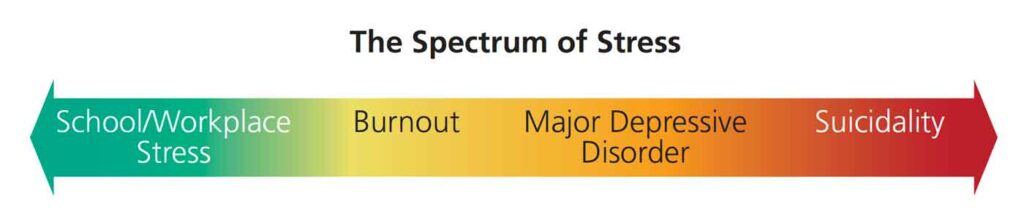
In a 2019 study of 2053 dentists in the United Kingdom, 54.9% reported currently experiencing high job stress, with general dentists noting the highest level of stress.18 The most common sources were worrying (43.8%), threats of complaints/litigation (79%), dissatisfied patients (75.1%), concern about the General Dental Council — the organization that regulates dental professionals in the United Kingdom (72.8%), work pressure from National Health Service (NHS) to meet financial goals (72.4%), running behind schedule (64.9%), performing NHS work (63.2%), and dealing with difficult patients (61.2%).18 The research also found that dentists displayed much higher levels of suicidal thoughts than the general population due to the fear of litigation and external regulations, thus making dentists more prone to stress, burnout and psychological distress.18
Lloyd and Musser19 investigated the personality traits of medical students as compared to dental students, and found dental students are more obsessive-compulsive in degree and number of symptoms, more codependent, 50% less likely to seek help, and are more competitive and isolating. These attributes are in line with the personality types that enter into dentistry as a profession.19 Results indicate that dental students evidenced considerably higher symptom levels than those previously reported in a general population survey.19 Compared with the general population, dental students showed a mild elevation in somatic symptomatology, a moderate elevation in anxiety and depressive symptomatology, and a marked elevation in obsessive-compulsive symptomatology and interpersonal sensitivity.19
It is possible these marked elevations in obsessive-compulsive symptomatology and interpersonal sensitivity may reflect, in part, a sensitization to excessive performance demands. This sensitization may manifest in cognitive inefficiencies — such as indecisiveness, blocking or memory impairment — and excess sensitivity to the evaluative judgments of other people.19 In comparing dental students with other sample groups, dental students were also found to display more psychiatric symptomatology than general medical subjects judged free of psychiatric illness, and to approach levels of symptomatology found in general medical subjects judged psychiatrically ill or in need of psychiatric treatment.19 In a 2017 study in Massachusetts, dentists were reported to have similar or higher prevalence than the general population for stress, alcohol consumption, prescription drug use, back pain, neck pain, headache, osteoarthritis and gastroesophageal reflux disease.20
PERFECTIONISM
The concept of perfectionism in dentistry can be divided into two categories: perfectionistic concerns, and perfectionistic strivings.
Perfectionistic Concerns:21 Unhealthy perfectionism can be destructive and paralyzing. This is earmarked by a dentist setting unreachable or unreasonable goals, such as feeling like he or she must learn and offer all types of dentistry to patients. Another example would be setting unrealistic production goals in an effort to pay off debt. A key warning sign of an unhealthy practitioner is seeking and accepting only perfection in all cases. This can be a major stumbling block. The goal of good dental work is not “perfection,” but excellence in care. When the dental work fails or does not turn out as expected, the dentist should see this as a learning experience to improve future care. Mistakes should not be seen as reflecting unworthiness or “not being good enough,” but, rather, as testament to the practitioner’s humanity. This is a good way to improve who a dentist is as a clinician and a person. Remaining humble and teachable are key to improving the clinical drive toward excellence.21
Perfectionistic Strivings:21 A dentist with a healthy view of perfectionism sets reasonable and reachable goals. This provider sees dentistry as a continual learning experience, views patient care as a journey, and is thankful for the opportunity to practice dentistry. When clinical outcomes are less than hoped for, the individual rebounds quickly after dealing with it and processing how to improve — and without catastrophizing. A well-balanced practitioner does not obsess on failure or mistakes, but tries to remain humble and teachable, while being open to accepting constructive criticism in order to move forward.
Dentists exhibiting perfectionistic concerns are more prone to overall burnout, exhaustion (emotional/physical), depersonalization (including cynicism), sarcasm and compassion fatigue — all of which will hinder work performance. Ultimately, these actions are destructive and earmarked by poor coping skills. In comparison, dentists exhibiting perfectionistic strivings are less prone to these debilitating behaviors. Their actions are motivating and earmarked by good coping skills.21
Perfectionists deal with many issues that can result in burnout, such as unrealistically high standards of performance, mistakes, doubts, expectations and criticism of self and others, and feelings of not being in control or not knowing everything. Perfectionism can be paralyzing, causing the clinician to stagnate and procrastinate in decision-making and action. A provider who sets perfection as the standard for dental care is not only unrealistic, but is in denial about his or her humanity. No one is perfect. The goal in healthcare should reflect a standard of excellence in care, a continual evaluative process of how to improve care through education, and acceptance of imperfection.
MITIGATING BURNOUT
Other than the time tested and anecdotal results of eating healthy, getting plenty of sleep, and exercising, the emphasis currently is to focus on web-based solutions, such as addressing relaxation, breathing, mindfulness, meditation, online cognitive behavioral therapy, and suicide prevention.22 These are great tools to implement, but should be used as adjuncts to address office issues, increase social interaction with the community and colleagues, minimize isolation, manage family/office time efficiently and, for those inclined, practicing religious beliefs. Controlling the office appointment book through block scheduling is an immediate step practitioners can take to reduce stress.
CONCLUSION
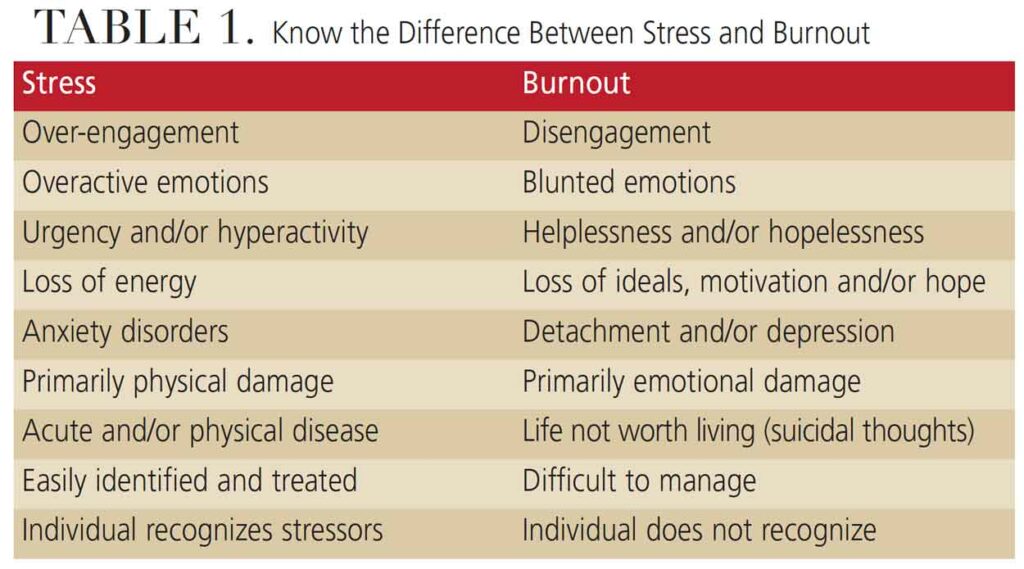
Burnout has been described as “an inflammation that occurs when people and work don’t fit together properly.” In some ways, calling burnout an “inflammation” is exactly what living with burnout feels like, a constant irritation that is ever-present and doesn’t get better unless addressed (Table 1). The good news is that burnout is preventable if recognized early and the individual asks for help.
Today’s environment for coping with stress-related work issues has never been better, as help and healing techniques are readily available for those who seek them. The goal of this article is to provide insights into the factors that contribute to professional burnout, and encourage dental providers to be proactive in taking care of themselves and seeking help if necessary.
REFERENCES
- Reith TP. Burnout in United States healthcare professionals: a narrative review. Cureus. 2018;10:e3681.
- World Health Organization. Burnout an “Occupational Phenomenon:” International Classification of Diseases. Available at: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases. Accessed March 31, 2021.
- Maslach C, Jackson SE, Leiter MP. The Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press;1996.
- Cocker F, Joss N. Compassion fatigue among healthcare, emergency and community service workers: a systematic review. Int J Environ Res Public Health. 2016;13:618.
- de Pedro MM, Fernández-Valera MM, García-Izquierdo M, Sánchez MI. Burnout, psychological capital and health during COVID-19 social isolation: a longitudinal analysis. Int J Environ Res Public Health. 2021;18:1064.
- North Carolina Caring Dental Professionals. Resources. Available at: https://nccaringdental.com/library-new/resources/. Accessed March 31, 2021.
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among U.S. physicians relative to the general U.S. population. Arch Intern Med. 2012;172:1377–1385.
- Yates SW. Physician stress and burnout. Am J Med. 2020;133:160–164.
- Yansane A, Tokede O, Walji M , et al. Burnout, engagement, and dental errors among U.S. dentists. J Patient Saf. April 3, 2020. Epub ahead of print.
- Martínez AA, Aytés LB, Escoda CG. The burnout syndrome and associated personality disturbances. The study in three graduate programs in dentistry at the University of Barcelona. Med Oral Patol Oral Cir Bucal. 2008;13:E444–E450.
- Leiter MP, Maslach C. Areas of worklife: a structured approach to organizational predictors of job burnout. In: Perrewe PL, Ganster DC, eds. Research in Occupational Stress and Well Being. Vol. 3. Oxford: Elsevier; 2014:91–134.
- Ayers KM, Thomson WM, Newton JT, Rich AM. Job stressors of New Zealand dentists and their coping strategies. Occup Med (Lond). 2008;58:275–281.
- American Dental Association. 2003 Dentists Well-Being Survey. Chicago: American Dental Association; 2005.
- Rada RE, Johnson-Leong C. Stress, burnout, anxiety and depression among dentists. J Am Dent Assoc. 2004;135:788–794.
- Kay EJ, Lowe JC. A survey of stress levels, self-perceived health and health-related behaviors of UK dental practitioners in 2005. Br Dent J. 2008:204;E19.
- American Dental Association. 2015 Dentists Well-Being Survey. Chicago: American Dental Association; 2017.
- Kulkarni S, Dagli N, Duraiswamy P, et al. Stress and professional burnout among newly graduated dentists. J Int Soc Prev Community Dent. 2016;6:535–541.
- British Dental Journal. More than half of dentists say stress is affecting their practice. Available at: https://www.nature.com/articles/sj.bdj.2019.18#citeas. Accessed March 31, 2021.
- Lloyd C, Musser LA. Psychiatric symptoms in dental students. J Nerv Ment Dis. 1989;177:6–69.
- Nalliah RP, Budd A, Allareddy V. Pilot survey of the health of Massachusetts dentists. J Investig Clin Dent. 2017;8.
- Curran T, Hill AP. Perfectionism is increasing over time: a meta-analysis of birth cohort differences from 1989 to 2016. Psychol Bull. 2019;145:410–429.
- Pospos S, Young IT, Downs N, et al. Web-based tools and mobile applications to mitigate burnout, depression and suicidality among healthcare students and professionals: a systematic review. Acad Psychiatry. 2018;42:109–120.
From Decisions in Dentistry. May 2021;7(5)36-39.