 UNDEFINED/GETTY IMAGES PLUS
UNDEFINED/GETTY IMAGES PLUS
Laminar Impressions for Unsupported Maxillary Tissue
This impression technique uses a laminar approach with a custom tray to record unsupported maxillary tissue in complete denture prosthodontics
This course was published in the November 2020 issue and expires November 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the clinical challenges involved in making impressions of edentulous patients.
- Discuss various methods for impressing an unsupported anterior maxillary ridge in a relaxed state.
- Describe the laminar impression technique, and how it can be adapted to help produce more accurate impressions in prosthodontics patients with mobile tissue.
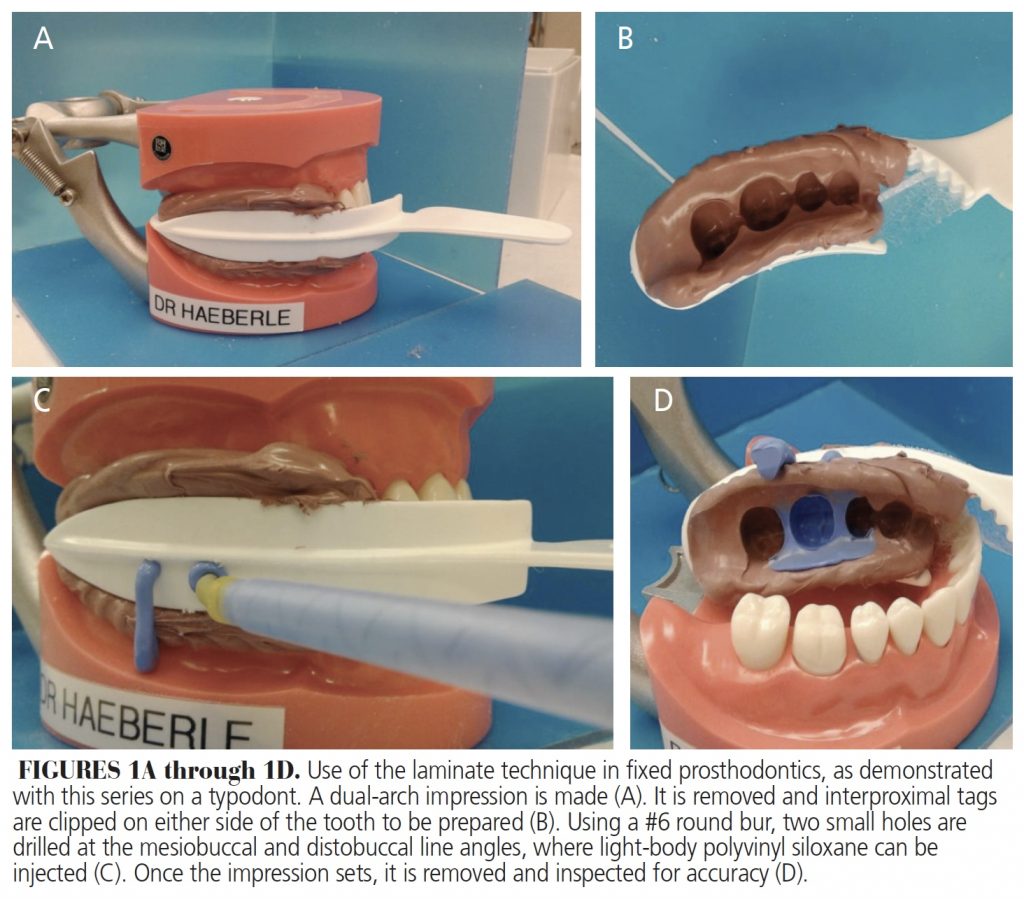
The laminar impression technique has been used in fixed prosthodontics for single crown impressions.1,2 Initially, a half-arch, double-sided impression tray is used to capture a heavy-body polyvinyl siloxane (PVS) impression of the unprepared tooth with the patient closed in maximum intercuspation (Figures 1A through 1D). After polymerization and removal of the impression, holes are drilled into the tray using a #6 or #8 round bur at the mesial and distal line angles. Following completion of the crown preparation, the impression is reinserted and the patient closes into the previously recorded position (i.e., maximum intercuspation). Light-body PVS impression material is injected into the mesial hole of the tray until sufficient material extrudes from the distal hole. By impressing the preparation and surrounding tissues with this technique, the clinician captures a detailed record with less chance of distortion. This article describes an adaption of the laminar impression technique using a single custom impression tray with a two-step impression sequence to overcome the challenges of making impressions that minimally displace mobile tissue in an edentulous patient.
The concepts, methods and materials utilized with edentulous impressions have been reported since the middle of the 18th century.3 In a chronology of events described by Starke,4 various materials have been employed for this procedure. Wax and plaster of paris were used from the mid-1800s through the early 1900s. The development of modeling plastics helped clinicians obtain a more customized fit. Further development led to improved formulations of wax and modeling compounds that were malleable using hot water. Early in the 20th century and beyond, additional advances were seen in impression waxes, along with the introduction of other materials, such as zinc oxide, alginates, polysulfide rubber, polyether and PVS. Many of these materials continue to be a part of removable prosthodontics treatment.
Numerous papers have reported on various impression techniques for complete denture prosthodontics.5–8 A common philosophy taught for making final impressions7 for complete denture prostheses involves the use of selective pressure. The selective pressure impression technique combines aspects of both mucostatic and functional impression techniques.8 This method is based on the histological anatomy of the supporting tissues.9 The selective pressure impression involves preparation of a custom impression tray to ensure the application of light pressure to areas of the arch that can best tolerate functional loads. Healthy mucosa firmly bound to underlying dense cortical bone is best suited to withstand masticatory forces. In the maxilla, stress-bearing areas include the crest of the ridge and lateral palatal slope. For the mandible, the main stress-bearing areas are the buccal shelves. Conversely, minimal to no pressure is applied to areas of the arch that are not suited for stress under function — such as structures in the anterior maxilla, midpalatine raphe, and loosely bound tissue. These areas require wax relief with the process of tray fabrication.10
As materials and techniques evolved, researchers examined how tissues react to the impression based on the amount of pressure exerted during the procedure.11,12 The clinical presentation of ridge morphology, tissue health and tissue displaceability will impact decisions about the best impression method to create a stable, retentive and comfortable prosthesis. A custom tray can be fabricated and modified based on the impression philosophy used.
UNSUPPORTED ANTERIOR TISSUE
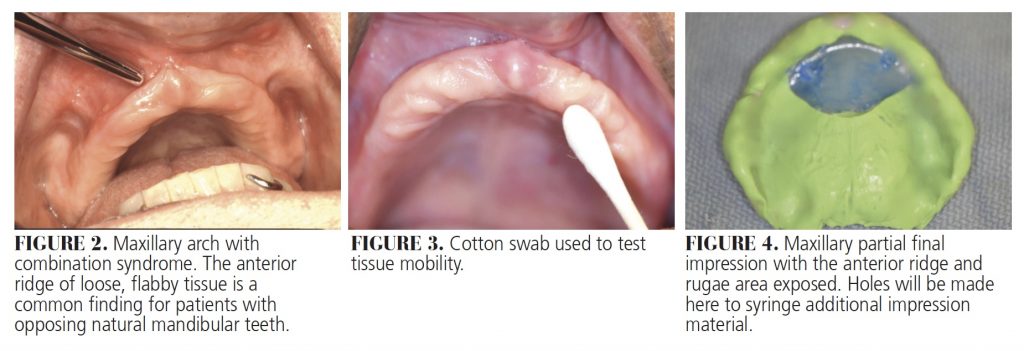
An occasional finding with edentulous patients is loose, unsupported tissue in the anterior maxillary ridge. Anterior hyperfunction syndrome (combination syndrome), first described by Kelly,13 is found in some patients with an edentulous maxillary arch opposing mandibular anterior natural teeth (usually the last teeth to be lost). The patient’s function, as well as the load placed against the premaxilla, leads to the development of this condition (Figure 2). Other findings reported by Kelly13 include unsupported tissue in the anterior maxilla, pneumatized tuberosities, palatal irritation with papillary hyperplasia, epulis fissuratum, and resorption of the posterior mandibular alveolar ridges. A number of clinical studies have investigated patients with maxillary complete dentures opposing mandibular anterior teeth. While hypermobile tissue in the anterior maxilla was not apparent in some cases,14–16 a small but statistical correlation was found in others.17–19 Two studies noted that more than half of their subjects displayed excessive resorption in the premaxilla.20,21 The presence of flabby tissue in the anterior maxilla has also been observed when the opposing arch has implant-retained overdentures.22,23
Some combination of functional and mucostatic impression techniques may be used to overcome the challenges of making an impression that minimally displaces mobile tissue. This article describes a technique using a single custom impression tray with a two-step impression sequence. Holes in the anterior portion of the tray enable low-viscosity PVS impression material to be injected — like the laminar impression technique — to capture the anterior unsupported ridge in a static state.
TECHNIQUE IN DEPTH
A patient who had been edentulous for 20 years presented to the clinic requesting new dentures. Her chief concern was an inability to eat comfortably with her existing dentures. Upon examination, it was determined the anterior maxillary ridge displayed mobile tissue (Figure 3). By palpation of the ridge, it was discovered this extended posteriorly to the canine region bilaterally. Following a discussion to explain the findings and treatment options, the patient decided on conventional treatment without surgical augmentation or dental implants.
Preliminary alginate impressions were made using stock edentulous trays of appropriate size for the patient, and diagnostic casts were made with Type III dental stone. A double layer of relief wax was applied to the maxillary anterior aspect of the cast. A custom tray was fabricated using visible light-cured resin. The borders of the custom tray were adjusted to create space for border molding using heavy-body PVS material.
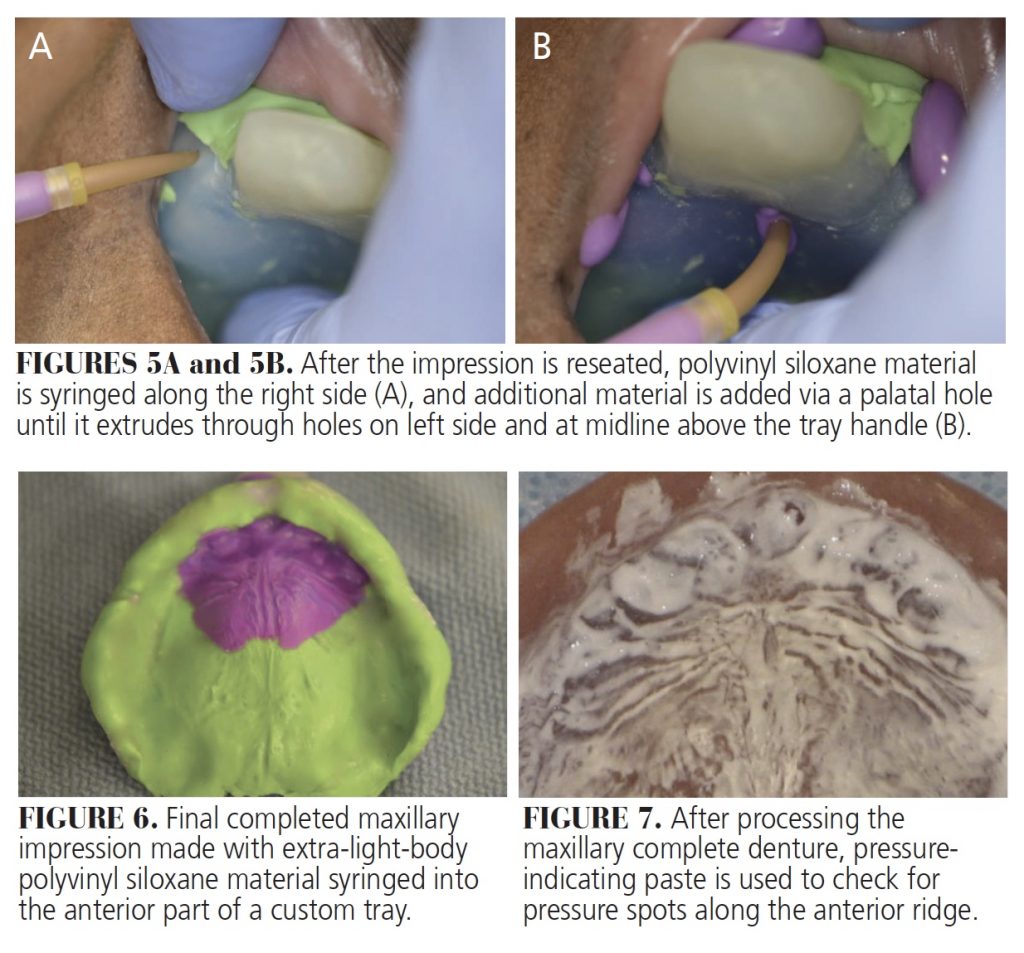
The maxillary final impression was taken in two parts. For the first part, where the tissue was well supported, a light-body PVS impression was made (Figure 4). Upon removal, the impression was inspected for accuracy and pressure areas. Any material that extended anteriorly (where double relief wax was placed) was removed. Four holes were placed in the impression tray in the area lying over the unsupported tissue. Following the application of tray adhesive, the ridge was dried and the impression tray was repositioned intraorally. An impression syringe with extra-light-viscosity PVS was used — similar to the laminar impression technique in fixed prosthodontics — to inject impression material into the right and palatal holes until material was seen flowing from the other areas.
After the material set, the impression was removed and inspected (Figures 5A and 5B, and Figure 6) before being boxed and poured to create the master cast. Subsequent steps led to the fabrication and delivery of maxillary and mandibular complete denture prostheses. At the day of insertion, pressure-indicating paste was used to evaluate the intaglio surface for possible areas showing excessive pressure (Figure 7). An even distribution of the pressure paste was noted, indicating the tissue was not subject to excessive force.
![Laminar impressions figure]() DISCUSSION
DISCUSSION
Residual ridge resorption following tooth extraction is a phenomenon that varies with the individual, but may proceed throughout the life of an edentulous patient.24 When the resorption leads to an unsupported or flaccid ridge, it can create denture instability, loss of retention and tissue irritation. Taking an accurate impression that does not displace this tissue presents a challenge: If the clinician does not account for flabby tissue, it could be distorted by the compression of the technique.25
Management can be achieved by varying the impression procedure to minimize tissue distortion. Different methods to impress an unsupported anterior maxillary ridge in a relaxed state have been reported using open window or perforated custom impression trays, solid trays with extra relief wax in the anterior region, and sectional trays using a variety of impression materials.26–34 Bench studies have shown that with flabby tissue, tray design can affect impression outcomes.35 Consequently, this case employed an alternative approach to previously published techniques, and utilized the concept of laminar impressions to minimize tissue displacement. The advantages of this technique are that the custom impression tray is one piece and the secondary impression of the unsupported tissue is contained, thus reducing the risk of it separating or being displaced. Choosing one type of impression material (e.g., PVS) that is dimensionally stable is an advantage when using a two-stage approach with a windowed tray in association with plaster of paris or irreversible hydrocolloid.
Other means of treating combination syndrome include surgical correction to reduce the ridge, ridge augmentation with bone graft or synthetics, or placement of dental implants.36–40 Surgery to reduce the unsupported tissue may compromise the ability to achieve sufficient surface area to support a complete denture. Bone grafts (with or without implants) to help retain a full prosthesis may create a financial burden on the patient. Basic prosthodontic principles involving accurate impressions that are well adapted and cover the basal seat of each arch with well-extended borders are key steps toward prosthesis support and stability. Good, functional occlusal relationships, with minimal anterior vertical overlap and routine follow-up to check proper fit and occlusion, are also important to ensure that forces associated with mastication are equally distributed.
SUMMARY
Combination syndrome is characterized by the features that occur when an edentulous maxilla is opposed by natural mandibular anterior teeth, including loss of bone from the anterior portion of the maxillary ridge. This results in redundant soft tissue in the area, which creates a challenge when making the final impression.
The technique described here uses a single custom impression tray and employs a two-stage PVS final impression — with the second part utilizing the concept of laminar impressions adapted from the fixed partial prosthodontics impression technique. This approach captures the mobile tissue of the denture-bearing surface in a static position. Using a one-piece custom tray helps confine the material better than other techniques using windowed or two-piece impression trays.
References
- Schoenrock GA. The laminar impression technique. J Prosthet Dent. 1989;62:392–395.
- McMaster DE. Using the laminar impression technique for provisional restorations. J Am Dent Assoc. 2000;131:1324–1325.
- Zimmer ID, Sherman H. An analysis of the development of complete denture impression techniques. J Prosthet Dent. 1981;46:242–249.
- Starke E Jr. A historical review of complete denture impression materials. J Am Dent Assoc. 1975;91:1037–1041.
- Massad J, Cagna D. Vinyl polysiloxane impression material in removable prosthodontics. Part 1: edentulous impressions. Comp Contin Educ Dent. 2007;28:452–459.
- el-Khodary N, Shaaban N, Abdel-Hakim A. Effect of complete denture impression technique on the oral mucosa. J Prosthet Dent. 1985;53:543–549.
- Petropoulos VC, Rashedi B. Current concepts and techniques in complete denture final impression procedures. J Prosthodont. 2003;12:280–287.
- Devan M. Basic principles of impression making. J Prosthet Dent. 1952;2:26–35.
- Boucher C. Impressions for complete dentures. J Am Dent Assoc. 1943;30:14–25.
- Duncan JP, Raghavendra S, Taylor TD. A selective-pressure impression technique for the edentulous maxilla. J Prosthet Dent. 2004;92:299–301.
- Oh WS, Morris HF. The principles of functional and mucostatic impressions for complete denture bases: a review. Comp Contin Educ Dent. 2017;38:664–667.
- Tripathi A, Singh SV, Aggarwal H, Gupta A. Effect of mucostatic and selective pressure impression techniques on residual ridge resorption in individuals with different bone mineral densities: a prospective clinical pilot study. J Prosthet Dent. 2019;121:90–94.
- Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 1972;27:140–150.
- Carlsson G, Ortorp A, Omar R. What is the evidence base for the efficacies of different complete denture impression procedures? A critical review. J Dent. 2013;41:17–23.
- Palmqvist S, Carlsson G, Owall B. The combination syndrome: a literature review. J Prosthet Dent. 2003;90:270–275.
- Desjardins R, Tolman D. Etiology and management of hypermobile mucosa overlying the residual ridge. J Prosthet Dent. 1974;32:619–638.
- Sülün T, Sakar O, Bilhan H, Ispirgil E. The effect of mandibular anterior teeth on the hypermobile tissue in the anterior part of the maxillae. Arch Gerontol Geriatr. 2012;55:12–15.
- Resende C, Ribeiro J, Dias K, et al. Signs of combination syndrome and removable partial denture wearing. Rev Odontol UNESP. 2014;43:390–395.
- Shen K, Gongloff R. Prevalence of the ‘combination syndrome’ among denture patients. J Prosthet Dent. 1989;62:642–644.
- Salvador MC, do Valle AL, Ribeiro MC, Pereira JR. Assessment of the prevalence index on signs of combination syndrome in patients treated at Bauru School of Dentistry, University of Sao Paulo. J Appl Oral Sci. 2007;15:9–13.
- Bagga R, Robb ND, Fenlon MR. An investigation into the prevalence of combination syndrome. J Dent. 2019;82:66–70.
- Elsyad MA, Ashmawy TM, Faramawy AG. The influence of resilient liner and clip attachments for bar-implant-retained mandibular overdentures on opposing maxillary ridge. A 5-year randomized clinical trial. J Oral Rehabil. 2014;41:69–77.
- Tymstra N, Raghoebar GM, Vissink A, Meijer HJ. Maxillary anterior and mandibular posterior residual ridge resorption in patients wearing a mandibular implant-retained overdenture. J Oral Rehabil. 2011;38:509–516.
- Carlsson GE. Responses of jawbone to pressure. Gerodontol. 2004;21:65–70.
- Antonelli J, Guerrero M, Georgescu M, Ortiz J. Quantifying flabby ridge tissue displacement during impression-making for patients with combination syndrome. Comp Contin Educ Dent. 2019;40:e1–e7.
- Daher T, Dermendjian S, Morgano SM. Obtaining maxillomandibular records and definitive impressions in a single visit for a completely edentulous patient with a history of combination syndrome. J Prosthet Dent. 2008;99:489–491.
- Shum MH, Pow, EH. Management of excessive movable tissue: a modified impression technique. J Prosthet Dent. 2014;112:387–389.
- Crawford RW, Walmsley AD. A review of prosthodontic management of fibrous ridges. Br Dent J. 2005;199:715–719.
- Bansal R, Kumar M, Garg R, Saini R, Kaushala S. Prosthodontic rehabilitation of patient with flabby ridges with different impression techniques. Indian J Dent. 2014;5:110–113.
- Labban N. Management of the flabby ridge using a modified window technique and polyvinylsiloxane impression material. Saudi Dent J. 2018;30:89–93.
- Pai UY, Reddy VS, Hosi RN. A single step impression technique of flabby ridges using monophase polyvinylsiloxane material: a case report. Case Rep Dent. 2014;2014:104541.
- Jyoti N, Shah N, Karthik MM. Prosthodontic rehabilitation of patients with combination syndrome. Int J Dent Clin. 2010;2:37–44.
- Lynch CD, Allen PF. Management of the flabby ridge: using contemporary materials to solve an old problem. Br Dent J. 2006;200:258–261.
- Bolouri A, McKinney TW. Two-stage impression making for complete dentures over loose, mobile supporting tissues. Comp Contin Educ Dent. 1988;10:196,199–201.
- Shin J, Ko KH, Huh YH, Cho LR, Park CJ. Displacement of simulated flabby tissues by different tray designs and impression materials. J Prosthodont. 2019;28:444–451.
- Saito C, Luvizuto ER, Bosco AF, Goiato MC, Panzarini SR. Flabby ridge correction using an auxiliary technique with connective tissue graft. J Craniofac Surg. 2012;23:e112–e115.
- Williams CW, Meyers JF, Robinson RR. Hydroxyapatite augmentation of the anterior portion of the maxilla with a modified transpositional flap technique. Oral Surg Oral Med Oral Pathol. 1991;72:395–399.
- Peñarrocha M, Viña JA, Carrillo C, Peñarrocha D, Peñarrocha M. Rehabilitation of reabsorbed maxilla with implants in buttresses in patients with combination syndrome. J Oral Maxillofac Surg. 2012;70:e322–e330.
- Piermatti J. Rehabilitation of the edentulous maxilla complicated by combination syndrome with an implant overdenture: a case report. Gen Dent. 2013;61:64–69.
- Ogino Y, Masafumi K, Yamada J, Toriya K, Koyano K. Implant treatments for edentulous maxilla with anterior hyperfunction. J Oral Implantol. 2015;41:731–735.
From Decisions in Dentistry. November 2020;6(10): 40-43.