 SARAHKAYB / CC BY-SA (HTTPS://CREATIVECOMMONS.ORG/LICENSES/BY-SA/4.0)
SARAHKAYB / CC BY-SA (HTTPS://CREATIVECOMMONS.ORG/LICENSES/BY-SA/4.0)
Intrabony Xanthoma Detected During Implant Planning
This case report details the radiographic presentation and histologic appearance of intrabony xanthoma, and discusses features that can help distinguish it from more common odontogenic lesions.
This course was published in the September 2020 issue and expires September 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss terminology used when diagnosing and treating intrabony xanthomas.
- List any predilections associated with intrabony xanthomas, and some of the more common odontogenic lesions that may have a similar radiographic appearance.
- Describe the histological and radiographic appearance and features of intrabony xanthomas.
- Explain the primary treatment for intrabony xanthoma of the jaw, and imaging modalities that may help establish a differential diagnosis.
Xanthoma is a benign lesion consisting of lipid-rich foam cells or histiocytes. While xanthomas most commonly present on skin in various anatomic locations, such as subcutis of elbows, buttocks, knees, fingers, eyelids, and skin creases (particularly of palms), a deep tissue variant of occurs in synovium, tendon and bone.1 The word “xanthoma” is derived from the Greek word xanthos, which translates to yellow.2 There is an accumulation of loose histiocytes, cholesterol and lipid deposits, resulting in yellowish pigmentation in the skin. The primary form of hyperlipidemia is associated with cutaneous xanthomas.2 The primary form is genetic in origin and can be classified based on plasma triglyceride and cholesterol levels. The secondary form of hyperlipidemia affects patient with other medical conditions, including alcoholism, chronic liver failure, chronic renal failure and diabetes. A xanthoma, when observed within bone, is identified as an intrabony xanthoma.
CASE REPORT
A 49-year-old male presented to Midwestern University College of Dental Medicine in Glendale, Arizona in October 2017 for second opinion for potential dental implant placement in the maxillary anterior area. He brought radiographs from his previous dental office that included a cone beam computed tomography (CBCT) volumetric study, bitewings, and anterior periapical radiographs acquired in September 2017. The patient informed the practitioner that his previous dentist diagnosed root resorption of the maxillary left central incisor (tooth #9), and recommended extraction and dental implant placement. The patient’s medical history included surgical removal of basal cell carcinoma from his nose, followed by radiation therapy to the area in 2014. He also indicated a familial history of high cholesterol and was being monitored by his physician.
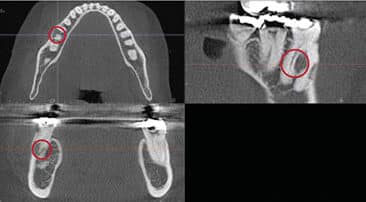
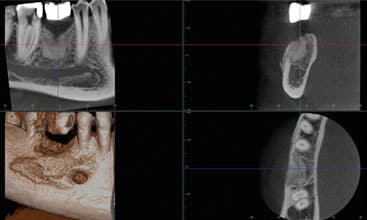
The outside CBCT scan was not accompanied by a formal radiology interpretation report. As part of the initial screening process, outside radiographs brought by the patient were reviewed by treating dental students, along with a board-certified oral and maxillofacial radiology faculty at the college. Radiographic findings included well-defined, low attenuation, homogeneous radiolucency present on the buccal aspect of the tooth #9, with no communication to the pulp canal — consistent with radiographic diagnosis of external root resorption of #9 (Figure 1 and Figure 2). Tooth #9 was extracted, and a socket preservation bone graft was completed for future dental implant placement. Although tooth #9 was the chief concern for the patient, it was the lower right that became the primary concern.
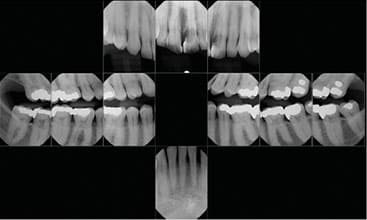
An incidental area of interest was observed in right mandibular posterior area by the oral radiologist, and was described as well-defined, homogeneous low attenuation radiolucency extending from mesial root of tooth #30 to the distal root of #30. This radiolucency extended from the furcation area superiorly to apical third of tooth roots. External root resorption was observed on the mesial aspect of tooth #30’s distal root. Mandibular buccal cortical bone adjacent to the furcation area of tooth #30 exhibited thinning, with slight expansion. No tooth displacement or perforation of buccal cortical plate was observed (Figure 3). Other incidental radiographic findings included deviation of the nasal septum, constricted airway, asymmetric hypoplastic left maxillary sinus, functional remodeling of right and left temporomandibular joints, and osteoarthritic changes in the cervical spine.
A histopathological examination was conducted, with hard tissue biopsy of the mandibular lesion, along with extraction of tooth #30. A diagnosis of intrabony xanthoma was made by an oral and maxillofacial pathologist.
RADIOGRAPHIC PRESENTATION
Most often observed in the second and third decades of life, intrabony xanthomas show no gender predilection. Gnathic lesions — that is, lesions relating to the jaw — usually present as a solitary radiolucency outlined by a well-defined periphery, with a strong predilection for the posterior mandible.1 They generally present as nonspecific homogeneous or mixed density radiolucency. Intrabony xanthomas can vary in radiographic appearance and present a corticated border, punched out border, or sclerotic border.
HISTOLOGIC PRESENTATION
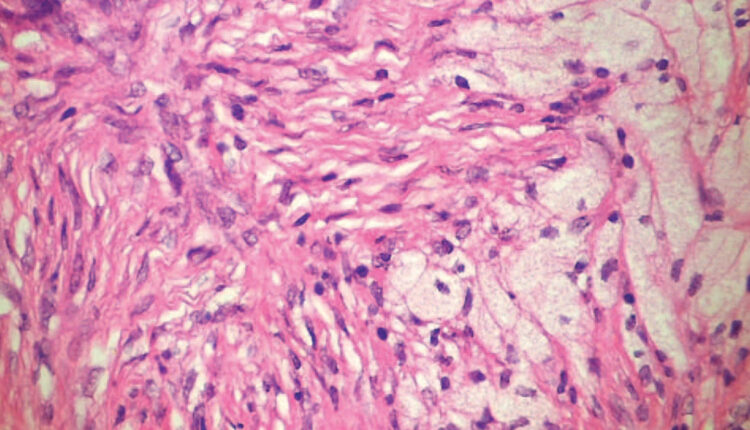
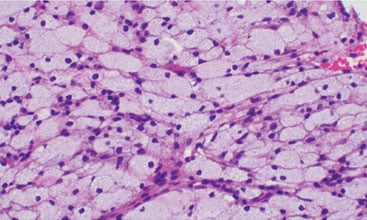
The predominant histologic feature of an intrabony xanthoma is the presence of foamy giant cells. The cells have abundant cytoplasm and hyperchromatic nuclei, which are small. These small nuclei are typically eccentrically located. These sheets of cells may be in clusters surrounded by fibrous tissue that does not have a storiform pattern, as seen in other lesions, such as benign fibrous histiocytomas and non-ossifying fibromas. The occasional non-foamy mononuclear or multinuclear giant cell is found, as well. The patient’s xanthoma was stained with hematoxylin and eosin. Sections revealed osseous tissue, with sheets of foam cells (xanthoma cells). These cells exhibited uniform oval dark nuclei, abundant pale cytoplasm, and distinct cytoplasmic borders. The xanthoma cells showed little variation in nuclear size, shape or chromaticity (Figure 4).
ODONTOGENIC LESIONS WITH A SIMILAR RADIOGRAPHIC APPEARANCE
Two characteristics of intrabony xanthomas make the radiographic diagnosis challenging: rarity of the lesion, and variability in radiographic features. Because the occurrence of this lesion is so low, clinicians may mistake it for more common lesions. In addition, intrabony xanthomas can mimic a wide range of disease entities, making a differential diagnosis through histopathological examination essential to obtaining an accurate diagnosis. For example, radiographically, ameloblastomas, buccal birfurcation cysts and clear cell odontogenic carcinoma may have an appearance similar to intrabony xanthomas.
Ameloblastoma — There are two variants of the ameloblastoma, the multicystic and unicystic. The multicystic is most often found in the posterior mandible and ascending ramus. The prevalence of this tumor is equal throughout the third to seventh decades of life, and there appears to be no gender predilection. These tumors appear most often as multilocular and radiolucent. When the lesions are large, they have a characteristic “soap bubble” appearance, and when they are smaller, they are said to have a “honeycomb” appearance. Expansion of the buccal and/or lingual plates is commonly seen if computed tomography is utilized to image the patient. Resorption of roots associated with this lesion may be seen, as well. If these lesions are unilocular, they exhibit a scalloped border, which should aid in the differential diagnosis.
Unicystic ameloblastomas are most commonly seen in younger patients, chiefly in the second decade of life. These tumors will be found most often in the posterior mandible. Intrabony xanthoma is similar in appearance to ameloblastoma, as both lesions present as radiolucencies. Ameloblastomas are known to cause remarked expansion of cortical plates, and present with a large number of internal septations, resulting in larger number of loculations or increased multilocularity. However, diagnosis of either lesion can only be made after histopathological evaluation.
Buccal Bifurcation Cyst — The buccal bifurcation cyst is an inflammatory odontogenic cyst. This cyst is relatively uncommon, but, when found, it is seen in children ages 4 to 14 years. It is found to affect the mandibular first molars predominantly. One third of the cases show bilateral involvement. This cystic lesion was first described in 1983 by Stoneman et al3 Radiographically, the lesion most often presents as a well circumscribed radiolucent lesion involving the buccal furcation and roots of the affected tooth. Size of the lesion will vary from 1.2 to 2.5 cm in diameter. If the lesion is imaged utilizing computed tomography, the root tips will be seen to be tipped toward the lingual. Some cases may also demonstrate proliferative periostitis of the cortical bone overlying the buccal cortex. This is demonstrated by single or multiple layers of reactive bone in the area immediately adjacent to the cyst. Intrabony xanthoma is similar in appearance to buccal bifurcation cyst, as both lesions present as radiolucencies. A buccal bifurcation cyst is known to apply pressure on the roots of mandibular molar teeth and results in tipping of teeth. This effect has not been documented or observed with intrabony xanthoma. However, diagnosis of either lesion can only be made after histopathological evaluation of hard and soft tissues in the area of the lesion.
Clear Cell Odontogenic Carcinoma — A rare neoplasm of the jaws, clear cell odontogenic carcinoma (CCOC) was first described by Hansen et al4 in 1985. It is predominantly found in the posterior mandible of women in their fifth through seventh decades of life. Its radiographic appearance typically reveals a radiolucent lesion, with ill-defined and or irregular borders. These can be unilocular or multilocular in nature, like ameloblastomas. These tumors can mimic ameloblastomas clinically, as well.5
Histologically, CCOC is characterized by sheets and islands of vacuolated/clear cells, while typically presenting as swelling in the anterior mandible.6
If the tumor is of adequate size, it can be destructive in nature. This could include the displacement or loss of dentition, destruction of the inferior alveolar nerve canal, and cortical bone and pathologic fracture. Tomographic images can reveal both solid and cystic components. These images may also confirm the destructive nature of the tumor, showing its invasive pattern of growth. Intrabony xanthoma is similar in appearance to CCOC, as both lesions can present as ill-defined radiolucencies. While CCOC is known to cause remarked destruction of alveolar bone, intrabony xanthoma has not been reported to be aggressive like CCOC in the rate and amount of bone resorption. Histopathological evaluation is mandatory to establish a diagnosis of CCOC.
MANAGING INTRABONY XANTHOMA
Treatment for primary intrabony xanthoma of the jaw is surgical enucleation and curettage. Because the etiology is not systemic (such as with hyperlipidemia), recurrence is rare. Although the lesions appear aggressive on radiographs, clinically they are not. Due to low recurrence rates and because the lesion is not locally aggressive, surgical treatment can be conservative. This should consist of enucleation and thorough curettage of the surrounding bone cavity. The treating surgeon should follow up on the patient with both clinical and radiographic examinations in an effort to detect possible recurrence.
The intrabony xanthoma identified in this case report was treated in this manner, along with extraction of tooth #30, which exhibited external root resorption. As of this writing, the area is healing, with no radiographic evidence of recurrence five months later, as observed on the CBCT scan acquired for dental implant planning (Figure 5).
CONCLUSION
Introducing oral health professionals to the existence, occurrence and characteristics of intrabony xanthomas will assist in making an accurate diagnosis of posterior jaw lesions. Because gnathic intrabony xanthomas can have a similar radiographic appearance as more common lesions, such as ameloblastomas, buccal bifurcation cysts and CCOC, they could easily be misdiagnosed.
The use of CBCT scanning is an excellent choice for maxillofacial imaging, as it creates non-superimposed images. This imaging modality has numerous applications in general dental and specialty dental practices. Incidental findings (i.e., additional findings unrelated to the original indication of the scan) are frequently identified on CBCT scans.7 This case report exemplifies the discovery of an incidental finding on a scan conducted for implant planning. If clinicians are aware of the existence of intrabony xanthomas and familiar with the radiographic presentation of these lesions, this imaging option can help establish a differential diagnosis. A histological examination should always be conducted to make the diagnosis and deliver appropriate treatment.
REFERENCES
- Marx RE, Stern D. Oral and Maxillofacial Pathology: A Rationale for Diagnosis and Treatment. Hanover Park, IL: Quintessence Publishing Co; 2002.
- Mateo MM, Torres MP, Alba LM, Gimilio ME, Gil JV. Primary mandibular bone xanthoma. Int J Oral Maxillofac Surg. 2004;33:806–807.
- Stoneman I, Buchner A, Taicher S. Mandibular buccal bifurcation cyst; The mandibular infected buccal cyst-molar area. Dent Radiogr Photogr. 1983;56:1–14.
- Hansen LS, Eversole LR, Green T, Powell NB. Clear cell odontongenic tumor — a new histologic variant with aggressive potential. Head Neck Surg. 1985;8:115–123.
- Park JC, Kim SW, Baek YJ, et al. Misdiagnosis of ameloblastoma in a patient with clear cell odontogenic carcinoma: a case report. J Korean Assoc Oral Maxillofac Surg. 2019;45:116–120.
- Datar UV, Kamat MS, Kanitkar SS, Byakodi SS. Clear cell odontogenic carcinoma: A rare case report with emphasis on differential diagnosis. J Cancer Res Ther. 2017;13:374–377.
- Dief S, Veitz-Keenan A, Amintavakoli N, McGowan R. A systematic review on incidental findings in cone beam computed tomography (CBCT) scans. Dentomaxillofac Radiol. 2019;48:20180396.
From Decisions in Dentistry. September 2020;6(8):32-35.





