
Implant Treatment Planning for Hybrid Prostheses
A clinical approach to planning, placement and restoration of implant supported hybrid prostheses.
This course was published in the June 2020 issue and expires June 2023. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the basic concepts of planning, placement, and the restorative phases of implant supported hybrid prosthesis therapy.
- Describe clinical indications for this form of implant treatment, as well as key diagnostic data used in case planning.
- Explain the means by which hybrid prostheses replace missing alveolar height.
First of a two-part series: The first article in this two-part series on implant supported hybrid prostheses covers the planning, placement and restorative phases of treatment. Appearing in a future issue, Part 2 will focus on maintaining hybrid prostheses and managing complications.
Although preventive dental care has improved dramatically, complete edentulism remains a major public health problem. According to the U.S. Centers for Disease Control and Prevention, 17.3% of Americans are missing all of their teeth.1 Edentulism is a chronic disability that affects quality of life; for example, the patient’s limited chewing ability restricts food choices and compromises nutrient intake.2 Furthermore, its effect on speech and esthetics may inhibit the ability to socialize.3 While removable complete dentures offer a cost-effective treatment option, their removable nature represents a major challenge for most patients. Fortunately, technology has improved the predictability of implant dentistry. This has dramatically increased the volume of implant treatment, including cases involving fully edentulous patients and fixed implant prostheses.
In 1952, Brånemark discovered the concept of osseointegration and applied it to fixed implant prostheses for edentulous patients, thus creating fixed complete dentures — also known as hybrid prostheses. This term is commonly used to describe a complete denture that is fully supported and retained by implants (i.e., it does not rely in soft tissue for support or stability). It is described as hybrid due to the dissimilar nature of the materials used in fabrication. This typically involves a metal bar (noble or titanium alloy) used as a framework that supports acrylic resin and denture teeth. Fixed complete dentures are defined as “a fixed dental prosthesis that replaces the entire dentition and associated structures of the maxillae or mandible; it cannot be removed by the patient.”4
When treating edentulous patients, an alternative to a hybrid prosthesis is the use of implant supported fixed prosthesis (i.e., implant bridges). This modality entails placement of more implants (six to eight) to provide multiple implant bridges per arch. Adequate alveolar bone height and width are essential for implant placement. Advanced bone loss can compromise the esthetic and biomechanical aspects of the implant prosthesis due to elongated clinical crowns and uneven prosthetic contours.
Unlike implant supported fixed bridges, hybrid prostheses replace missing alveolar height by means of pink acrylic resin used for teeth retention. Hybrid prostheses generally require fewer implants, and alveolar ridge morphology is not as critical because implants do not have to be placed “exactly where the teeth are.” This is due to the use of angle modification abutments (i.e., multiunit abutments). In other words, when there is a need to replace teeth but not alveolar height, an implant fixed prosthesis is a viable option. When alveolar morphology is less than ideal due to extensive bone resorption, either in some areas or the complete ridge, the hybrid restoration is a good option.5 Another factor to consider is the number of implants to be placed, as well as laboratory work, which can significantly change implant treatment, making the hybrid prosthesis generally a more affordable option.
Malo and colleagues6,7 introduced the all-on-four concept in 2003. This involves placing four implants per arch without preliminary grafting: two anterior vertical implants, and two posterior angled implants. In the mandible, the two posterior implants are placed just anterior to the mental foramina and angled distally about 30° relative to the occlusal plane. Distal maxillary implants are angled parallel to the anterior wall of the maxillary sinus, thus providing the same 30° angulation. Angled implants position the platform further distal in the arch and minimize cantilever.
Multiunit angled abutments allow the prosthetic screw access to be placed in a more favorable position through the cingulum/occlusal surface of the prosthetic teeth; this ensures a passive fit (Figure 1). Placement of longer implants in native bone provides higher insertion torque values, and generally allows immediate loading of the temporary prosthesis. Long-term success of this treatment has been reported at 94.8% to 96.4%, with a prosthetic survival rate of 99.2% to 100%, with up to 10-years follow up.8–15
There are four main phases when providing implant treatment for hybrid prostheses: (1) Diagnostic stage and treatment planning; (2) implant surgery and healing period; (3) prostheses fabrication; and (4) maintenance. The aim of this article is to review the first three phases of treatment. The maintenance phase, maintenance protocols, and long-term complications will be discussed in detail in the concluding article of this two-part series.

DIAGNOSTIC PHASE
Adequate patient selection is crucial for treatment success. During the diagnostic phase, a detailed medical history must be obtained. Special attention should be paid to uncontrolled systemic conditions that could complicate the surgical procedure and jeopardize patient’s safety and treatment outcome.
Due to the extensive nature of the surgery, the use of IV sedation is recommended. Sedation increases pain control and allows administration of emergency drugs. Medical clearance should be part of the diagnostic phase when systemic conditions are present. For example, uncontrolled diabetes impairs the patient’s ability to heal and increases the risk of postoperative infections. While properly controlled patients can be treated as nondiabetic, it is imperative to acknowledge this control must be maintained for long-term treatment success. It is recommended that HbA1c levels remain at 7.0 or less for ideal treatment conditions. Heart and respiratory conditions could present higher sedation and surgical risks, and lead to increased bleeding, low oxygen saturation, and increased risk for stroke or cardiac infarction, among other complications.
Systemic conditions that affect bone metabolism — such as osteoporosis, osteopenia, some types of arthritis, and cancer, among others — must be considered as part of the medical history. Medications used to treat such conditions should be assessed due to the risk of developing medication-related osteonecrosis of the jaw after implant surgery. This is a complication associated with anti-resorptive and antiangiogenic drugs (e.g., bisphosphonates and denosumab). Whenever possible, dental treatment should be completed prior to administration of the mentioned drugs.16
It is crucial to understand and manage patients’ expectations regarding implant treatment with hybrid prostheses. In general, edentulous patients adapt easier to the new prosthesis; they know the struggle presented by lack of teeth and use of removable dentures. Patients with terminal dentition must understand and cope with losing their teeth and having them replaced by prosthetic appliances. Each treatment step must be fully understood by the patient, as should the difference between teeth and implant prostheses.
During the diagnostic phase, a thorough extraoral and intraoral exam should be completed. It is important to consider the patient’s dental condition (edentulous or failing dentition), reason for edentulism (e.g., caries, periodontal disease or trauma), opposing dentition (e.g., complete denture, hybrid prosthesis or natural dentition), soft tissue condition, and presence of parafunction (e.g., bruxism). Parel and Phillips17 found the primary risk factors contributing to implant failure in patients with hybrid prostheses were opposing natural dentition, poor bone density, male gender, bruxism, and implant location in a distally inclined site. When one or more of these risk factors are present, treatment plan modifications must be considered — such as tissue grafting procedures, prosthetic material selection, additional implants, and modified loading protocols.
Clinical records must be obtained as part of the diagnostic process; these include study models mounted in an articulator (either analogic or digital), a full set of extraoral and intraoral photographs, and radiographic imaging (e.g., full mouth periapical series, panoramic radiographs and cone beam computed tomography [CBCT]).
In implant treatment planning for edentulous patients, a large field of view CBCT must be obtained to display key anatomical structures, such as the maxillary sinuses, base of the nose, zygomatic process (if zygomatic implants will be placed), inferior alveolar nerve, and the inferior border of the mandible. Small field of view CBCT images generally fail to include these anatomical structures. Two-dimensional radiographs are not recommended for treatment planning due to lack of information on bone width, anatomical structures, and three-dimensional implant positioning.
TREATMENT PLANNING
Prosthetic treatment planning for hybrid prostheses follows the principles utilized for complete dentures. The process involves creating a teeth setup (either digital or analog), and, when possible, teeth try-in. Attention must be paid to the esthetics, phonetics, occlusion and interocclusal space. A set of immediate dentures is fabricated from the teeth setup and used for immediate loading.
Virtual implant planning can be completed utilizing the CBCT data (Figure 2). In addition to implant treatment software, implant planning services are available for clinicians who do not have the time (or comfort) to use such software themselves. These services often provide the digital plan, surgical guides and immediate prosthesis.18
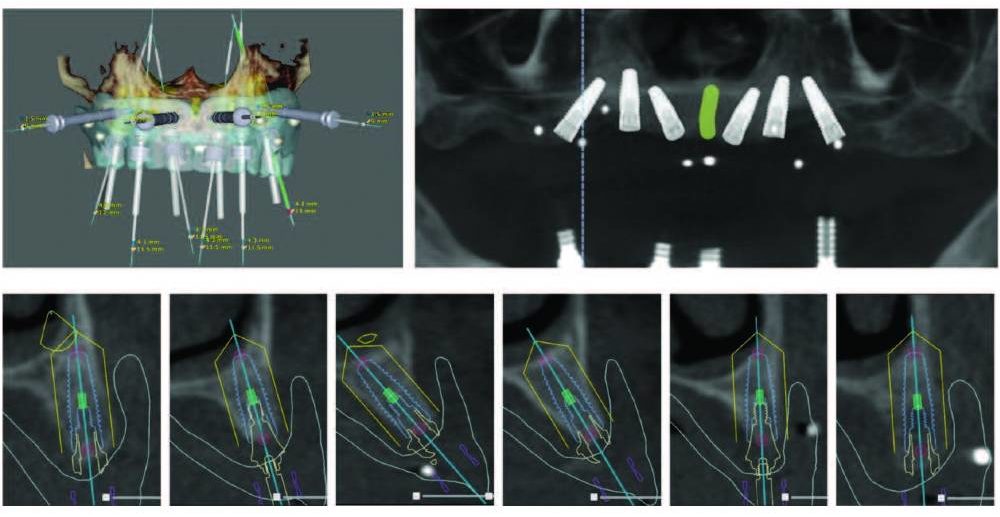
Implant width and length are selected according to the proposed placement sites; the software also helps calculate the position and angulation, as well as the multiunit abutments needed for angle correction. Tools within the software allow the clinician to determine bone density, implant proximity to anatomical structures, and identify other possible surgical complications. A complete virtual plan will provide information to stock the necessary implants, and plan the drilling sequence according to implant size and bone density.
Surgical guides are created based on the diagnostic teeth setup and available bone for implant placement (per the CBCT). Digital workflows allow the creation of a restrictive surgical stent that will guide every step of implant placement, from initial drilling to implant insertion, minimizing variation from the digital plan to the final implant position.
Interocclusal space must be considered during the planning phase. Hybrid prostheses should have a minimum height of 15 mm. This permits adequate material thickness and prevents prosthetic complications, such as prosthetic tooth fracture and framework fracture. Interocclusal space must be created (if not sufficient) by means of alveoloplasty; this is completed prior to implant placement and should be considered when selecting implant length.19
IMPLANT SURGERY
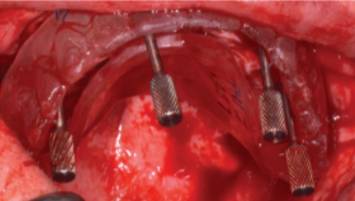
The use of a surgical guide is imperative to place the implants in the correct position and angulation. In some cases, implant placement can be completed in flapless fashion. The requirements are that the patient is already edentulous, no bone reduction is needed, and a fully restrictive surgical guide with the corresponding implant surgical kit is used.
If remaining teeth are extracted during the same surgery, buccal and lingual cortical bone must be preserved to allow implant placement and high insertion torque for immediate loading.
After tooth extraction, bone reduction is completed to allow for 15 mm of restorative space from the incisal edge to the implant platform. Bone can be reduced utilizing a surgical bur and copious sterile saline irrigation, or a reciprocating saw. Some surgical stents are designed to guide the bone reduction (Figures 3A and 3B). When bone reduction is completed, implant placement can be initiated.
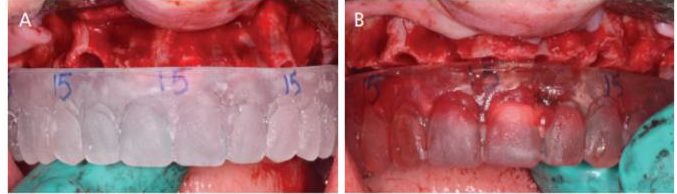
Subsequent to implant placement, multiunit abutments are selected and connected to the implants. Angle correction should place the prosthetic screw access through cingulum of anterior teeth and occlusal surface of posterior teeth; this can be evaluated with a clear duplicate of the denture (Figure 4). Multiunit abutments must be torqued as recommended by the manufacturer. Special care should be exercised when suturing the flaps to preserve as much keratinized tissue as possible on the buccal and lingual aspects of the implants.
An immediate denture can be converted to an implant fixed temporary prosthesis. This is known as immediate loading and can be completed if an insertion torque ≥ 35 Ncm for at least four implants is achieved.
Different techniques for immediate loading have been described; these can be direct (abutment pick-up in the mouth), or indirect (obtaining an impression and completing the process in the laboratory). The prosthetic appliance should provide the same result regardless of the method of fabrication.
Occlusion must be equilibrated to prevent implant overload and potential prosthetic fracture; toward this end, group function or balanced occlusion is recommended. Excessive load must be avoided on the cantilever section during the healing phase. The intaglio surface of the temporary prosthesis should be highly polished and free of concavities; in addition, flanges on the prosthesis should be avoided to prevent excess food and plaque accumulation, and allow for adequate hygiene. Radiographs must be obtained to confirm adequate implant placement and passive fit of the prosthesis.
Clinicians are advised to schedule regular follow-up appointments to ensure normal healing and proper self-care. The healing period is similar to any other implant treatment; when completed, final impressions can be made.
FINAL PROSTHESIS
The first step in making a final prosthesis is an accurate impression, and clinicians will generally utilize open-tray impression copings, splinted with pattern resin. This prevents movement of the copings during impression retrieval and pouring. The fabrication of a verification jig is recommended to ensure an accurate model has been obtained.
An implant retained, horseshoe-shaped baseplate and wax rim can be utilized for facebow and occlusal records. These procedures mimic complete denture fabrication. Teeth setup is completed and tried. It is important to ensure that sufficient vertical restorative space (minimum 15 mm) is provided for adequate material thickness.
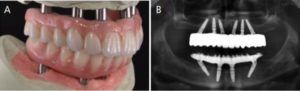
In building the final prosthesis, a metal framework supports the prosthetic teeth that were previously used during the wax try-in. The prosthesis is processed using polymethyl methacrylate wrapped around the titanium bar and prosthetic teeth (Figures 5A and 5B). After processing, the prosthetic contours are evaluated to ensure there are no concavities on the intaglio surface.
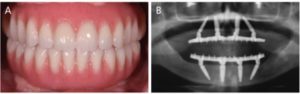
In recent years, advances in computer aided design/computer aided manufacturing and high-strength ceramic systems have allowed the creation of monolithic zirconia prostheses as an alternative to traditional hybrid prostheses (Figures 6A and 6B). An advantage of monolithic zirconia is the high resistance to fracture and wear compared to resin prosthetic teeth (which are the most common complications associated with hybrid prostheses).20
When placing the final prosthesis, a one-screw test is performed to ensure passive fit. This is completed by installing the prosthesis with only one screw and obtaining a radiograph; all implants must appear completely seated radiographically. Next, the rest of the screws are placed and torqued according to manufacturer specifications.
Occlusion must be carefully adjusted to achieve group function or bilateral balance (depending on the opposing arch). Adequate oral hygiene instruction should be provided to ensure that adequate self-care measures will be taken to improve the long-term prognosis and care of prosthetic implant treatment.
SUMMARY
In many cases, the utilization of hybrid prostheses is a viable option to restore function and esthetics in edentulous patients. When choosing this restorative modality, care should be exercised during each step of treatment to ensure optimal outcomes and avoid complications.
REFERENCES
- U.S. Centers for Disease Control and Prevention. Oral health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016. Available at: https://www.cdc.gov/oralhealth/pdfs_and_other_files/Oral-Health-Surveillance-Report-2019-h.pdf. Accessed May 19, 2020.
- Musacchio E, Perissinotto E, Binotto P, et al. Tooth loss in the elderly and its association with nutritional status, socio-economic and lifestyle factors. Acta Odontol Scand. 2007;65:78–86.
- Roumanas ED. The social solution-denture esthetics, phonetics, and function. J Prosthodont. 2009;18:112–115.
- The Glossary of Prosthodontic Terms: Ninth Edition. J Prosthet Dent. 2017;11:e1–e105.
- Bidra AS. Three-dimensional esthetic analysis in treatment planning for implant-supported fixed prosthesis in the edentulous maxilla: review of the esthetics literature. J Esthet Restor Dent. 2011;23:219–236.
- Malo P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Branemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):2–9.
- Malo P, Rangert B, Nobre M. All-on-4 immediate-function concept with Branemark System implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S88–S94.
- Malo P, Nobre M, Lopes A, Rodrigues R. Double full-arch versus single full-arch, four implant-supported rehabilitations: a retrospective, 5-year cohort study. J Prosthodont. 2015;24:263–270.
- Malo P, Nobre M, Lopes A, Ferro A, Gravito I. All-on-4 Treatment Concept for the rehabilitation of the completely edentulous mandible: a 7-year clinical and 5-year radiographic retrospective case series with risk assessment for implant failure and marginal bone level. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e531–e541.
- Malo P, Nobre M, Lopes A, Moss S. Posterior maxillary implants inserted with bicortical anchorage and placed in immediate function for partial or complete edentulous rehabilitations. A retrospective clinical study with a median follow-up of 7 years. Oral Maxillofac Surg. 2015;19:19–27.
- Malo P, Nobre M, Lopes A, Moss SM, Molina GJ. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011;142:310–320.
- Malo P, Nobre M, Lopes A, Ferro A, Gravito I. Immediate loading of implants placed in patients with untreated periodontal disease: a 5-year prospective cohort study. Eur J Oral Implantol. 2014;7:295–304.
- Martens F, Vandeweghe S, Browaeys H, De Bruyn H. Peri-implant outcome of immediately loaded implants with a full-arch implant fixed denture: a 5-year prospective case series. Int J Periodontics Restorative Dent. 2014;34:189–197.
- Cercadillo-Ibarguren I, Sánchez-Torres A, Figueiredo R, et al. Immediately loaded implant-supported full-arches: peri-implant status after 1–9 years in a private practice. J Dent. 2017;67:72–76.
- Testori T, Galli F, Fumagalli L, et al. Assessment of long-term survival of immediately loaded tilted implants supporting a maxillary full-arch fixed prosthesis. Int J Oral Maxillofac Implants. 2017;32:904–911.
- Svejda B, Muschitz C, Gruber R, et al. Position paper on medication-related osteonecrosis of the jaw (MRONJ). Wien Med Wochenschr. 2016;166:68–74.
- Parel SM, Phillips WR. A risk assessment treatment planning protocol for the four implant immediately loaded maxilla: preliminary findings. J Prosthet Dent. 2011;106:359–366.
- Greenberg AM. Digital technologies for dental implant treatment planning and guided surgery. Oral Maxillofac Surg Clin North Am. 2015;27:319–340.
- Bidra AS, Agar JR, Parel SM. Management of patients with excessive gingival display for maxillary complete arch fixed implant-supported prostheses. J Prosthet Dent. 2012;108:324–331.
- Venezia P, Torsello F, Cavalcanti R, D’Amato S. Retrospective analysis of 26 complete-arch implant-supported monolithic zirconia prostheses with feldspathic porcelain veneering limited to the facial surface. J Prosthet Dent. 2015;114:506–512.
From Decisions in Dentistry. June 2020;6(6):36–39.




