 ALEX-MIT/ISTOCK/GETTY IMAGES PLUS
ALEX-MIT/ISTOCK/GETTY IMAGES PLUS
Immediate Implant Placement and Provisionalization in the Esthetic Zone
This technique report details the use of an extracted tooth for the fabrication of a screw-retained, implant supported provisional crown following immediate implant placement in the esthetic zone.
Immediate implant placement along with immediate provisionalization are high-demand procedures when planning extraction of an non-restorable anterior tooth, particularly when located in the maxillary arch.1–5 The combination of these techniques has proven to be a successful treatment option — providing the case is selected carefully.3,6–9 In order to consider this approach, the treatment area must not have an active infection present. In addition, the area needs an adequate amount of bone to insert the implant and support the soft tissue in the interproximal areas of the hopeless tooth. A thick, normal-scalloped periodontal biotype is also recommended. Ultimately, the main factor that will determine if an implant is adequate to receive a provisional crown following placement is the presence of primary stability of at least 35 Ncm.10,11 A noncontributory history of bruxism or parafunctional habits is also recommended.12,13
Fabricating a crown for immediately placed implants can be accomplished using different techniques. The most common methods involve matrices using different materials and techniques (from custom clear to prefabricated), in conjunction with computer aided design/computer aided manufacturing technology. These matrices are usually relined with auto-polymerized acrylic resin or bis-acryl material.2,14,15 This requires extra time and planning during the surgical appointment to establish adequate emergence profile to support the peri-implant soft tissues. In addition, during this appointment the clinician must provide an esthetic result consisting of a well-aligned crown, with proper contours and shade that are in harmony with the adjacent dentition and smile line.
While these methods are successful, they are not as predictable when it comes to the esthetic outcome due to characterization of the facial portion of the crown. To mimic craze lines, hypocalcification or staining in a provisional could represent a difficult challenge during fabrication at the surgical appointment.
An alternative solution is the use of the extracted natural tooth — when available and in good condition — for fabrication of the provisional crown. This technique report illustrates the fabrication of a screw-retained, implant-supported provisional crown following immediate implant placement, which was accomplished by using the extracted natural tooth as the main component. The objective of this approach is to preserve and use the facial portion of the tooth for the provisional crown and provide a predictable esthetic outcome. It also creates a reference to establish adequate support for the peri-implant soft tissues, and identify an efficient location for the incisal edge and interproximal contacts during the surgical appointment. In addition, the use of the patient’s tooth can further provide a comfortable transition toward the definitive restoration.
TECHNIQUE REPORT
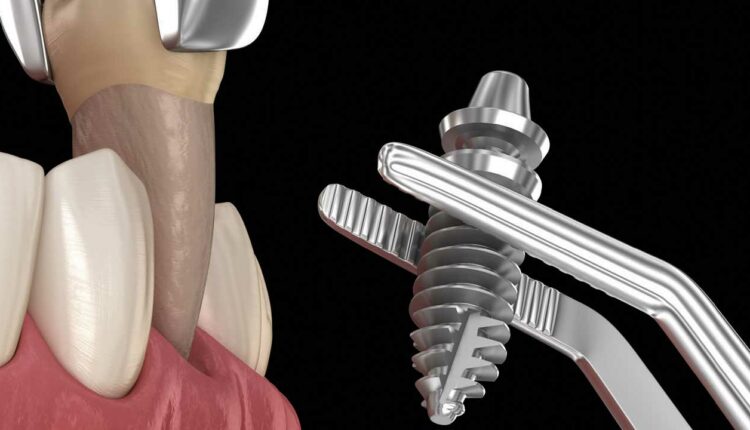
In cases in which a successful nontraumatic extraction of a non-restorable anterior tooth is performed (Figure 1), presurgical data collection should consist of a thorough diagnostic and radiographic examination, periodontal assessment, and occlusal records. A critical analysis of the smile and patient’s expectation should also be considered.16 An orientation index is fabricated prior the extraction using polyvinyl siloxane putty material.
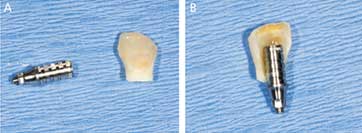
Upon extraction, there must be minimal trauma, preserving the facial and interproximal bone, followed by immediate implant placement. It is necessary to achieve primary implant stability, with a minimal insertion torque > 35 Ncm (Figure 2). After verification of the implant’s position and angulation, a temporary titanium abutment is hand-tightened into the implant and marked to the appropriate height. The temporary abutment is removed for extraoral adjustment, including additional retentive grooves using a carbide disc, and then hand-tightened back onto the implant (Figure 3). The natural tooth is steam-cleaned and adjusted to accommodate the temporary abutment (Figures 4A and 4B), using the prefabricated index as a reference.
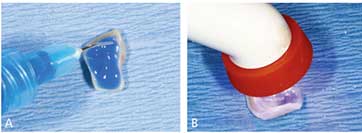
After confirmation of an accurate fit, the internal surface of the tooth is etched with 37% phosphoric acid for 30 seconds, followed by the application of a bonding agent and light polymerization (Figures 5A and 5B). With the use of the index, the adjusted natural tooth is aligned and attached to the temporary abutment with flowable composite resin for a screw-retained design through the palatal orifice (Figure 6). The connected piece is removed from the implant (Figure 7) and attached to an implant replica compatible with the placed implant. Composite resin is used to fill voids and shape the lingual, critical and subcritical contours17 to create an adequate emergence profile.
The provisional prosthesis is tried intraorally and adjusted extraorally in the cervical area of the crown until adequate support of the peri-implant soft tissues (without excessive pressure) is obtained. Occlusion is adjusted accordingly, providing clearance of contact in centric and eccentric movements.18 The tooth/composite interface is finished and thoroughly polished using finishing discs and polishing points (Figure 8) to develop a good soft tissue attachment.19 The screw is tightened to 30 Ncm,20 and the screw vent is blocked using polytetrafluoroethylene tape and composite. The occlusion is checked and occlusal clearance verified with a shim stock.

connected piece.
DISCUSSION
There are many reasons why a tooth may need to be extracted. In most scenarios, the clinical crown of the tooth remains in good condition and can be used. The method described here represents a practical and effective interim solution with an acceptable esthetic outcome; it also ensures patient comfort and provides adequate support to the peri-implant soft tissues by maintaining a good blood supply and preserving the architecture. These features support a comfortable transition for the patient, which is especially valuable for individuals who have not previously experienced edentulism or a removable prostheses.
For the case illustrated in this article, the patient was pleased with the provisional restoration (Figure 9). The final provisional showed some gray translucency due to the use of a metal abutment, as well as the amount of dental structure removed to accommodate the temporary abutment. It is recommended to use opaque resin or peek abutments to avoid this issue.

tissues.

dentition.
The patient was scheduled for postoperative follow-up appointments at one week and one month post-insertion. The patient referred little discomfort one week following the procedure; however, the gingiva demonstrated no sign of trauma (Figure 10 and Figure 11). The patient maintained a soft diet and avoided biting using the provisional crown. One month after implant placement and provisional delivery, the peri-implant soft tissue maintained the architecture and showed no sign of recession or inflammation (Figure 12).

When planning for implant placement in the anterior area and considering the option of immediate provisionalization,3,6–9 it is important to acknowledge the level of characterization required for the interim prosthesis to fulfill esthetic expectations.15 Some cases may be more challenging than others, particularly if there are translucency, craze lines or staining that could be difficult to mimic in a short period following implant placement.15 In this particular situation, staining and characterization could be problematic, especially when working in a surgical environment. In addition, establishing an adequate emergence profile could be more challenging due to the lack of reference, increasing the chances of not providing adequate support to the peri-implant soft tissues.17
The tissue response to the patient’s own tooth is expected to be superior to other provisional materials, which are prone to plaque accumulation when porous or unpolished.21 In addition, the duplication of the contours of the natural tooth, especially on the cervical third of the provisional crown, is expected to preserve the soft tissue morphology and allow creation of a natural-looking emergence profile.19 When a crown is overcontoured or undercontoured, it may result in lack of control of the soft tissue architecture — which may not be compatible with the definitive prosthesis.
CONCLUSION
This technique report provides an alternative option for the fabrication of a provisional crown following implant placement through the use of the natural extracted tooth. The rationale, transfer method, and materials are described for the reader. When using this technique with proper case selection, the clinician may provide a smooth prosthetic transition, with an excellent esthetic outcome and preservation of the soft tissue contours.
KEY TAKEAWAYS
- Immediate implant placement and provisionalization are frequent and well-accepted techniques for restoring single units in the esthetic zone.
- This report describes a method of using the extracted natural tooth to fabricate a screw-retained, implant-supported provisional crown following immediate implant placement.
- Given the right case, this approach can decrease treatment time while efficiently creating the emergence profile, therefore providing adequate support to the peri-implant soft tissues.
- In addition, it provides immediate esthetic results, with a favorable transition designed to satisfy the patient’s expectations.
REFERENCES
- Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. InJ J Oral Maxillofac Implants. 2003;18:31–39.
- Kolerman R, Nissan J, Rahmanov A, Zenziper E, Slutzkey S, Tal H. Radiological and biological assessment of immediately restored anterior maxillary implants combined with GBR and free connective tissue graft. Clin Implant Dent Relat Res. 2016;18:1142–1152.
- Del Fabbro M, Ceresoli V, Taschieri S, Ceci C, Testori T. Immediate loading of postextraction implants in the esthetic area: systematic review of the literature. Clin Implant Dent Relat Res. 2015;17:52–70.
- Cooper LF, Reside GJ, Raes F, et al. Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: a 5-year prospective evaluation. Int J Oral Maxillofac Implants. 2014;29:709–717.
- Bukhari SA, AlHelal A, Proussaefs P, Garbacea A, Kattadiyil MT. Use of patient’s own natural teeth as part of the interim prosthesis on immediately placed single implants in a staged surgical approach: A clinical report. J Oral Implantol. 2018;44:351–357.
- Norton MR. The influence of insertion torque on the survival of immediately placed and restored single-tooth implants. Int J Oral Maxillofac Implants. 2011;26:1333–1343.
- Slagter KW, den Hartog L, Bakker NA, Vissink A, Meijer HJ, Raghoebar GM. Immediate placement of dental implants in the esthetic zone: a systematic review and pooled analysis. J Periodontol. 2014;85:e241–e250.
- Wöhrle PS. Single-tooth replacement in the aesthetic zone with immediate provisionalization: fourteen consecutive case reports. Pract Periodontics Aesthet Dent. 1998;10:1107–1114,quiz 1116.
- Knoernschild KL. Early survival of single-tooth implants in the esthetic zone may be predictable despite timing of implant placement or loading. J Evid Based Dent Pract. 2010;10:52–55.
- Bhekare A, Elghannam M, Somji S, Florio S, Takanori S. Case selection criteria for predictable immediate implant placement and immediate implant provosionalization. J Oral Biol. 2018;5:6.
- Schwartz-Arad D, Chaushu G. Placement of implants into fresh extraction sites: 4 to 7 years retrospective evaluation of 95 immediate implants. J Periodontol. 1997;68:1110–1116.
- Cercadillo-Ibarguren I, Sánchez-Torres A, Figueiredo R, Valmaseda-Castellón E. Early complications of immediate loading in edentulous full-arch restorations: A retrospective analysis of 88 cases. Int J Oral Maxillofac Implants. 2017;32:1116–1122.
- Bahat O, Sullivan RM. Parameters for successful implant integration revisited part II: algorithm for immediate loading diagnostic factors. Clin Implant Dent Relat Res. 2010;12(Suppl 1):e13–e22.
- Ross SB, Pette GA, Parker WB, Hardigan P. Gingival margin changes in maxillary anterior sites after single immediate implant placement and provisionalization: a 5-year retrospective study of 47 patients. Int J Oral Maxillofac Implants. 2014;29:127–134.
- Siadat H, Alikhasi M, Beyabanaki E. Interim prosthesis options for dental implants. J Prosthodont. 2017;26:331–338.
- Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004;25:895–896,898,900 passim,quiz 906–907.
- Lai HC, Zhang ZY, Wang F, Zhuang LF, Liu X, Pu YP. Evaluation of soft-tissue alteration around implant-supported single-tooth restoration in the anterior maxilla: the pink esthetic score. Clin Oral Implants Res. 2008;19:560–564.
- Proussaefs P. Immediate provisionalization with a CAD/CAM interim abutment and crown: a guided soft tissue healing technique. J Prosthet Dent. 2015;113:91–95.
- Trimpou G, Weigl P, Krebs M, Parvini P, Nentwig GH. Rationale for esthetic tissue preservation of a fresh extraction socket by an implant treatment concept simulating a tooth replantation. Dent Traumatol. 2010;26:105–111.
- Roccuzzo M, Aglietta M, Cordaro L. Implant loading protocols for partially edentulous maxillary posterior sites. Int J Oral Maxillofac Implants. 2009;Suppl 24:147–157.
- Wang WC, Suzuki T. Utilization of extracted teeth as provisional restorations following immediate implant placement — a case report. Singapore Dent J. 2015;36:23–28.
The authors have no commercial conflicts of interest to disclose.
From Decisions in Dentistry. March 2021;7(3):10–12,14.








