ZORANM/E+/GETTY IMAGES PLUS
ZORANM/E+/GETTY IMAGES PLUS
Digital Designs and Fabrication in Restorative Practice
Seung Kee Choi, DMD, MS, offers perspective on the clinical advantages of utilizing digital designs and manufacturing in restorative care
Even if a dental office does not utilize impression scanning or custom fabrication via in-office computer aided design/computer aided manufacturing (CAD/CAM), nearly all modern restorative procedures involve digital designs and manufacturing. For example, traditional impressions that are sent out are generally digitized by the laboratory, which uses the data to design and manufacture the prosthesis using CAD/CAM techniques. And with improvements in software and hardware, including milling units and three-dimensional (3D) printers — along with dropping prices — more offices are embracing in-house design and manufacturing.
To gain perspective on the digital aspect of restorative treatment, we asked SEUNG KEE CHOI, DMD, MS,of the Department of Advanced Oral Sciences and Therapeutics at the University of Maryland School of Dentistry to discuss strategies that will allow dental teams to take full advantage of CAD/CAM workflows.
Whether clinicians use an intraoral scanner to create digital impressions or a commercial laboratory digitizes traditional impression materials, digital scans are a cornerstone of restorative CAD/CAM practice. What are the advantages of intraoral scanning?
One clear advantage over conventional impression-making and wax-ups is the ability to form images of patient’s intraoral condition almost instantaneously. The advantages are analogous to obtaining radiographic images using a digital sensor versus conventional film. Using digital data, the clinician can quickly gain diagnostic values, such as occlusion and positions and proportions of teeth. Moreover, digital designs can be created in less time than diagnostic wax-ups, and can serve as an effective visual tool to communicate various problems to the patient, as well as when discussing treatment plan options.</p
Overall, clinicians and patients may find the evaluation/consult appointments more efficient using data obtained from intraoral scanning than those obtained via conventional impressions and wax-ups. In addition, the quality of treatment outcomes can be improved with intraoral scanning. Clinicians can evaluate tooth preparations immediately after an intraoral acquisition of the preparations, which can be magnified and visualized for details such as occlusal clearance, taper and smoothness. If necessary, modifications can be made chairside and the existing intraoral scan can either be modified or a new intraoral scan obtained in minutes. Based on the evidence that digitally fabricated restorations can provide equal or greater accuracy than conventional restorations, this quality assurance measurement should further increase clinicians’ and patients’ confidence in the outcome.1,2
Digital systems have their own challenges in terms of data security and storage, but maintaining digital data does not involve the same issues as maintaining physical patient data in the form of casts, paper records and impressions. The use of dental stones and impression materials can be reduced or even eliminated from the clinic, increasing physical space while reducing cost and issues with storing and handling the material. Disasters, such as fire and flooding, can render physical patient data useless, but may not affect the integrity of digital data (especially if it is constantly backed up in a remote location). The efficiency of communicating with patients and colleagues (e.g., referring dentists, specialists and laboratory technicians) can also be enhanced through digital data.
Are there instances in which conventional impressions might be more appropriate than an intraoral scan?
In spite of the clear advantages of intraoral scanning, there are instances in which a conventional impression is more appropriate. One instance is difficulty in accessing the area of interest with the intraoral scanner. If the intraoral scanner utilizes a camera head design that is too large for the patient or the patient has a limited mouth opening, conventional impression technique should be used. In the areas of the mouth where space is limited (e.g., teeth #2, 15, 18 and 31), capturing the finish line around the interproximal area of the tooth preparation — which may require tilting the camera tip — can be extremely difficult. Last but not least, a patient who is not able to remain still may affect the accuracy of the scan or even make it difficult to acquire intraoral scans entirely. For these instances, conventional impressions should be considered.
When it comes to CAD software and designing restorations in-house, what’s involved in terms of costs, training and staffing needs? Are time constraints a factor in clinical practice?
Most CAD software programs are not free. In fact, in addition to the initial purchase price, many require an additional fee to receive software support and updates, which are often necessary to fix bugs in the programs. Companies may provide initial training at no cost. Beyond this, online media (e.g., social media and online digital study clubs) may provide useful forums for exchanging ideas for troubleshooting and creating solutions to challenges. However, users may find such forums inadequate to attain the necessary training to deal with daily hardware and software issues. In this instance, advanced training in the form of continuing education provided by an experienced clinician or company technician/ clinician will be useful — but typically entails additional costs.
A properly trained staff member should be designated as the in-house “expert” in digital technologies. An in-house laboratory technician may be the preferred arrangement for a very productive clinic since she or he can provide the necessary laboratory support. Of course, hiring a technician adds to the cost of operating a digital clinic.
Time is another cost associated with designing restorations in-house. It is likely that dentists will need to design the restorations themselves if their clinic lacks support staff (as mentioned above). Most clinicians will experience a learning curve, which can require considerable time initially. Furthermore, clinicians inexperienced with CAD software will find designing errors not only time-consuming to resolve, but also frustrating and discouraging.
For most routine restorations (single-unit crowns, for example), designing restorations using CAD software should be a relatively straightforward and efficient process, even in an office where additional trained staff members are not available. Still, a clinic that has the potential to be efficient with CAD/CAM should consider having a CAD/CAM-trained staff member so doctors can focus on maximizing their chairtime, rather than spending time with digital designs.
Workflow demands, clinician preference, and the dental team’s skill set will all affect this decision, so it really becomes an individual choice based on the practice. Speaking personally, the only reason I would ask the laboratory to design the restoration would be if I didn’t have time to design it myself and/or I didn’t have personnel in my clinic who were trained to handle the task. Other clinicians may prefer to delegate the design function to the lab, freeing the team for other procedures.
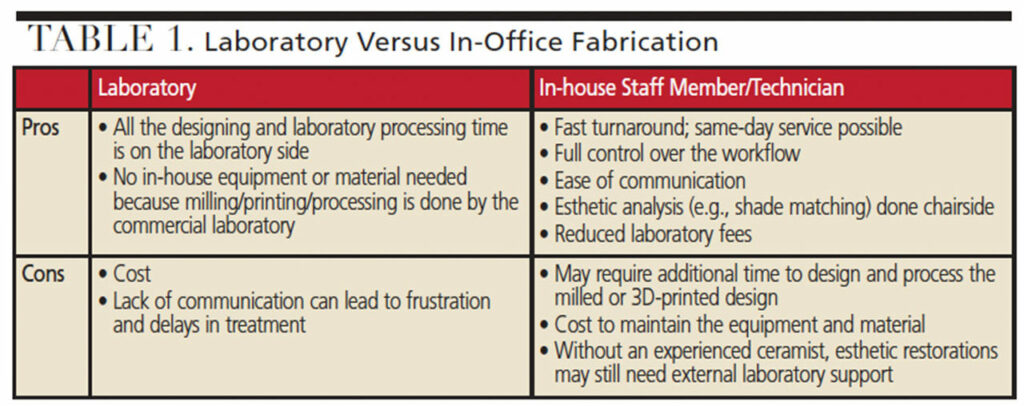
The same thinking applies to the fabrication process, as there are pros and cons to handling fabrication in-house or using the lab to manufacture the prosthesis. Table 1 provides an overview of the advantages and disadvantages of each approach.
What are the key indications for in-office milling? What demands does it place on the team, and what are its limitations in clinical practice?
In-office milling is indicated for various single-unit restorations (e.g., inlays, onlays, veneers and crowns). Short-span fixed partial dentures can also be milled in-office. Since milling can produce good surface finishes, provisional restorations and denture bases are indicated for in-office milling, as well.
Various types of support can help make in-office milling a success. Ideally, a staff member who is experienced in digital design and operating the milling unit (e.g., loading and starting the milling process, and changing the milling burs and coolant when necessary) would be a valuable part of the workflow.
An individual who can finish the milled restorations (by crystallizing if the material is lithium disilicate, or sintering if zirconia) and characterize them would be equally helpful. Thus, a smooth transition is necessary between each of the steps in the digital workflow, and effective communication is needed among team members in order to deliver the milled restoration during the given appointment time. However, even with the properly trained individuals in place, problems (such as hardware and/or software issues) can occur unexpectedly, putting the team under pressure to deliver the restoration/s on time. It is therefore expected that clinics without adequate support would be under much pressure if their goal were to deliver same-day restorations.
In terms of limitations in clinical practice, machine wear — specifically milling burs — should be expected and addressed with timely replacement.
What are the most common indications for 3D printing in restorative therapy? Are there limitations to existing technology — for example, do we currently have 3D materials suitable for printing permanent crowns and bridges?
The printers and materials used in 3D custom fabrication are constantly evolving, which means applications are expanding, too. For instance, 3D printing of resin materials is becoming popular for producing dentures, as well as designs to be invested for casting metal restorations or pressing ceramics. However, the most common indication for 3D printing is perhaps fabrication of implant surgical guides, which can be done in-office with accuracy and at reasonable cost.
One of the limitations of the existing technology in 3D printing is indeed material. There are publications showing both the potential and challenge of printing ceramics for fixed restorations. Though it can be expected that ceramics — and metals, too — may become available for printing in the future, these are not yet applicable to routine patient care.
Another limitation of 3D printing technology is that it is very sensitive to inconsistency in the digital file. Often, software programs are necessary to ensure the digital designs are “watertight” or defect-free, and such programs can add to the cost of using this technology.
Briefly explain the advantages of CAD/CAM technology in removable prosthodontics.
The advantages of utilizing CAD/CAM technology in removable prosthodontics include:
- Reduced number of patient appointments (which can be as few as two), as well as less laboratory processing time
- Convenience of reproducing removable prostheses by using the stored data • Compared to conventionally processed bases, efficient delivery of the prostheses due to superior fit of the milled denture bases (since the milling process utilizes prepolymerized acrylic resin that will not undergo polymerization shrinkage during milling)
- Superior strength of the denture base compared to a conventionally processed base
- Also, the CAD/CAM denture base may be more biohygienic than conventionally processed denture base because it contains less residual monomer and is more hydrophobic than conventional materials.
Please discuss the clinical viability of integrating conventional and digital techniques in restorative treatment.
Though going “fully digital” is a goal many dental clinics and laboratories strive to achieve, it is beneficial, and sometimes necessary, to incorporate conventional techniques in the digital workflow.
In removable prosthodontics, it is feasible to rely on digital technology from the beginning (scanning the patient intraorally) to the end (milling or printing the prosthesis). However, clinicians who don’t have access to an intraoral scanner can utilize conventional impressions. Some of the commercially available digital workflows for removable prosthodontics also incorporate making conventional impressions and the centric relation record at the start of treatment, prior to digitizing them (though this step may become digital soon once a reliable intraoral scanning method is determined). Clinicians and technicians who prefer to use conventional denture teeth for various reasons (perhaps due to esthetics and availability of the teeth) may have the denture bases milled to have those teeth set in wax for the try-in. Laboratories also may choose to process denture bases and teeth to metal frameworks for removable partial dentures, even if the framework was milled, and milled denture teeth could be bonded to the framework.
In fixed prosthodontics, most restorations can be fabricated digitally. When considering esthetic restorations, it is difficult to fully rely on digital technology. A skilled laboratory technician (a master ceramist, for example) who is experienced with producing natural color and proportion of teeth by hand-layering the ceramic material is extremely valuable to the digital workflow in esthetic cases. When considering metal restorations, laboratories that cannot afford to purchase equipment to mill metal may rely on a small 3D printer or milling unit to produce a pattern for the restoration. The pattern would then be conventionally processed (say, by casting).
Any final thoughts?
Technology and material science are continually evolving, and this greatly impacts the cutting edge of CAD/CAM dentistry. For this reason, much of the information provided here is subject to change (possibly in the near future). However, it is important to remember that CAD/CAM dentistry is still deeply rooted in the sound concepts and principles that should govern all phases of evidence-based care.
REFERENCES
- Fasbinder DJ. Computerized technology for restorative dentistry. Am J Dent. 2013;26:115–120.
- Chochlidakis KM, Papaspyridakos P, Geminiani A, Chen CJ, Feng IJ, Ercoli C. Digital versus conventional impressions for fixed prosthodontics: a systematic review and meta-analysis. J Prosthet Dent. 2016;116:184–190.