 LESION, CC BY-SA 3.0
LESION, CC BY-SA 3.0 Diagnosis of Endodontic-Periodontal Lesions
Because they can present with similar signs and symptoms, an understanding of the endodontic-periodontal continuum will help clinicians reach an accurate diagnosis.

Determining the precise etiology of an endodontic-periodontal lesion can be challenging because these lesions can present with similar signs and symptoms. Because successful treatment ultimately relies on an accurate diagnosis, it is critical that the primary etiology be identified before therapy is initiated.
The root canal system and periodontium are interconnected.1 The primary mode of communication between the root canal system and periodontium is through the apical foramina because these openings are the largest, and bacteria and/or their by-products can freely pass through them.
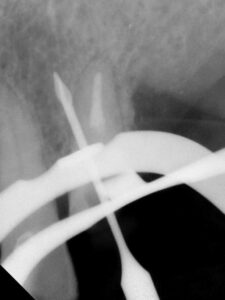
The smaller lateral and/or accessory canals can also act as a mode of communication between the root canal system and periodontium. Lateral and accessory canals are formed during tooth development due to a disturbance in the Hertwig’s epithelial root sheath and subsequent entrapment of blood vessels and connective tissue.2 The incidence of lateral canals varies with root location, with a lower frequency occurring coronally and a higher frequency occurring apically (Figures 1A and 1B).3 Accessory canals can also occur in the furcation region of mandibular molars. One investigator injected ink into molars under pressure and found the presence of furcation canals in 28% of teeth examined; however, the incidence of accessory furcation canals may be as high as 76%.4,5

Dentinal tubules are another potential mode of communication between the root canal system and periodontium. These tubules are usually covered with cementum that acts as a physical barrier. However, the cementum can be physically removed during periodontal treatment; in addition, a congenital absence of cementum is also possible. When the cementoenamel junction was studied using a scanning electron microscope, 18% of teeth were found to have exposed dentinal tubules at the cementoenamel junction due to a congenital absence of cementum.6

When the dental pulp is vital, there is an outward flow of dentinal fluid which contains immunoglobulins that can help prevent bacteria and/or their by-products from entering the root canal system.7 However, when the pulp becomes necrotic or the tooth has been previously treated, there is a lack of dentinal fluid, and this allows bacteria or their by-products to invade the root canal system more readily through the exposed dentinal tubules.
Vertical root fractures are yet another potential means of communication between the root canal system and periodontium. Clinical signs of a vertical root fracture include:
- A tooth that was previously treated endodontically
- J-shaped or “halo” radiolucency
- Deep, isolated periodontal pocket
- Coronally located sinus tract

The presence of two sinus tracts on both the buccal and lingual aspects are considered pathognomonic for a vertical root fracture.8 Although cone beam computed tomography has a low specificity for visualization of such fractures, there are common features that can be observed from cone beam imaging.9 These include:
- Loss of bone in the mid-root area, with intact bone coronal and apical to the defect
- Absence of the entire buccal plate of bone
- Radiolucency at the terminus of a post
- Space between the buccal and/or lingual plate of the bone and the root surface
- Visualization of the vertical root fracture10

Developmental malformations, such as vertical radicular grooves, can result in extensive periodontal attachment loss and bone destruction. As the groove becomes contaminated with bacteria and biofilm along its length, periodontal destruction continues until the periodontal pocket eventually reaches the apex of the tooth (Figures 2A through 2D).1

Other potential avenues of communication between the root canal system and periodontium include internal and external resorption (Figures 3A through 3E), perforations (Figure 4), and horizontal root fractures (Figure 5).
CAN ENDODONTIC PATHOSIS CAUSE PERIODONTAL PATHOSIS?
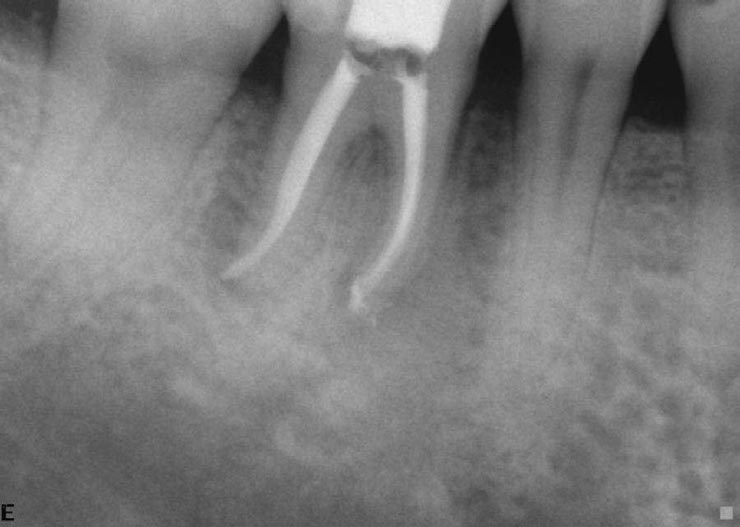
There is agreement between endodontists and periodontists that endodontic pathology can cause periodontal pathology. When the pressures from a dental abscess increase, the purulent exudate will follow the path of least resistance. If this path is through the periodontal ligament, a sinus tract can develop through the sulcus, resulting in a deep periodontal pocket. Pockets arising from pulpal disease should be expected to heal without the need for periodontal treatment (Figures 6A through 6C).1 However, studies indicate that a history of smoking, as well as extensive clinical attachment loss, deep probing depths, and severity of full-mouth periodontitis, are associated with a guarded prognosis for some endodontic-periodontal lesions.11

CAN PERIODONTAL PATHOSIS CAUSE ENDODONTIC PATHOSIS?
There is conflicting evidence as to whether periodontal disease can cause pulpal disease. Some investigators have reported pulpal changes, such as inflammation and pulp stones, next to lateral and accessory canals,12,13 whereas other investigators have found no correlation between periodontal disease and pulp histology.14,15 One investigator studied 414 advanced periodontally involved teeth, of which only 3% required root canal treatment.16 From a clinical standpoint, it can therefore be concluded that periodontal disease rarely causes pulpal necrosis due to the exposure of lateral and/or accessory canals.

On the other hand, endodontists and periodontists agree that if a periodontal pocket reaches the apical foramen, the pulp can become necrotic.17 Recent histological evidence has shown that when the periodontal pocket reaches the apex, the blood flow of the apical vessels can become compromised. In turn, bacteria can invade these compromised vessels and serve as avenues for the bacteria to enter the pulp.18

CLASSIFICATION OF ENDODONTIC-PERIODONTAL LESIONS
In 1972, Simon et al19 classified endodontic-periodontal lesions as: 1) primary endodontic lesions, 2) primary endodontic lesions with secondary periodontal involvement, 3) primary periodontal lesions, 4) primary periodontal lesions with secondary endodontic involvement, and 5) true combined lesions.

PRIMARY ENDODONTIC LESION
The etiology of a primary endodontic lesion is a necrotic and infected pulp. Although primary endodontic lesions may mimic the appearance of vertical root fractures, one of the signs of a vertical root fracture is that the tooth will have been previously endodontically treated. If the tooth has not been previously endodontically treated, the clinician should perform pulp sensibility testing. A deep periodontal pocket combined with a diagnosis of pulpal necrosis would indicate a primary endodontic lesion.20 In this case, root canal treatment should be completed, and healing should be expected to occur.

However, the presence of a primary endodontic lesion may also arise from a previously treated tooth with persistent endodontic disease. In this situation, the potential of a vertical root fracture should be considered, and the patient should be properly informed of all risks, benefits, and alternative treatments prior to the initiation of treatment.
PRIMARY ENDODONTIC LESION WITH SECONDARY PERIODONTAL INVOLVEMENT
As the name implies, the etiology of a primary endodontic lesion with secondary periodontal involvement is endodontic; however, the sulcular sinus tract has been patent for sufficient time for biofilm and calculus to form on the root surface. For these types of lesions, root canal treatment should be performed first, and the tooth should be reevaluated in three to six months for healing. If periodontal healing has not occurred, periodontal treatment should be performed. The treatment success of these lesions relies on the success of the periodontal therapy.19

PRIMARY PERIODONTAL LESION
The etiology of a primary periodontal lesion is radicular biofilm and calculus. In these types of lesions, periodontal pockets tend to be wider and more generalized, and calculus is typically visualized on the root. However, unless the periodontal pocket has reached the apex, the pulps of these teeth will almost always remain vital.17,18 If pulp sensibility testing confirms the pulp is vital, then only periodontal therapy is needed and the success rate depends upon the periodontal treatment.19

PRIMARY PERIODONTAL LESION WITH SECONDARY ENDODONTIC INVOLVEMENT
A primary periodontal lesion with secondary endodontic involvement arises when a periodontal pocket reaches the apex of the tooth, and the pulp becomes necrotic.17,18 The etiology of these lesions can either be from advanced periodontal disease or congenital defects, such as a longitudinal groove or invagination on a tooth root (Figures 2A through 2D). When present, these types of deep grooves or invaginations can act as a route for bacteria to reach the apex. When pulp sensibility testing confirms a diagnosis of pulpal necrosis, root canal treatment should be performed. However, because the primary etiology is periodontal in origin, the tooth will also require periodontal therapy. As before, the prognosis hinges on the success of the periodontal therapy.19
TRUE COMBINED LESION
The true combined lesion is rare. It occurs when an apical lesion that is expanding coronally merges with a periodontal pocket that is progressing apically. The prognosis of these cases is questionable. If treatment is to be rendered, the risks, benefits and alternatives must be discussed with the patient. Because these types of true combined lesions have both endodontic and periodontal etiologies, both root canal treatment and periodontal treatment are required. The prognosis of these types of lesions also depends upon the success of the periodontal therapy.19

CONCLUSIONS
An accurate diagnosis of endodontic-periodontal lesions can be confusing because these lesions can present with similar signs and symptoms. If a tooth has not been previously treated, and the pulp tests necrotic, root canal treatment should be performed, and no periodontal treatment is needed. If the pulp tests vital, then only periodontal treatment is indicated. However, in teeth with primary endodontic lesions with secondary periodontal lesions, primary periodontal lesions with secondary endodontic involvement, or true combined lesions, both endodontic and periodontal therapy are required. Because the therapeutic success rate of these combined lesions is ultimately determined by the periodontal treatment, it is recommended that a consultation be scheduled with a periodontist prior to initiation of any endodontic treatment.
KEY TAKEAWAYS
- Because the root canal system and periodontium are interconnected, determining the precise etiology of an endodontic-periodontal lesion can be challenging, as these lesions can present with similar signs and symptoms.
- With the understanding that successful treatment ultimately relies on an accurate diagnosis, it is critical that the primary etiology be identified before therapy is initiated.
- There is agreement between endodontists and periodontists that endodontic pathology can cause periodontal pathology. Yet there is conflicting evidence as to whether periodontal disease can cause pulpal disease.
- That noted, endodontists and periodontists agree that if a periodontal pocket reaches the apical foramen, the pulp can become necrotic.17
- Simon et al19 classified endodontic-periodontal lesions as: 1) primary endodontic lesions, 2) primary endodontic lesions with secondary periodontal involvement, 3) primary periodontal lesions, 4) primary periodontal lesions with secondary endodontic involvement, and 5) true combined lesions.
- True combined lesions are rare and occur when an apical lesion that is expanding coronally merges with a periodontal pocket that is progressing apically.
- Considering that true combined lesions have both endodontic and periodontal etiologies, both root canal treatment and periodontal therapy are required.
- As with all conditions, an accurate diagnosis will determine the treatment approach to any form of endodontic-periodontal lesion.
FIGURES 2A–2D COURTESY BIANCA ABOUBAKARE, DMD
FIGURES 3A–3E COURTESY JEFFREY KAWILARANG, DDS, MS
FIGURE 4 COURTESY ALAN H. GLUSKIN, DDS
REFERENCES
- Rotstein I, Simon JH. The endo-perio lesion: a critical appraisal of the disease condition. Endod Topics. 2006;13:34–56.
- Kuroiwa M, Kodaka T, Abe M, Higashi S. Three-dimensional observations of accessory canals in mature and developing rat molar teeth. Acta Anat. 1992;143:130–138.
- DeDeus QD. Frequency, location, and direction of the lateral, secondary and accessory canals. J Endod. 1975;1:361–366.
- Gutmann JL. Prevalence, location, and patency of accessory canals in the furcation region of molars. J Periodontol. 1978;49:21–26.
- Burch JG, Hulen S. A study of the presence of accessory foramina and the topography of molar furcations. Oral Surg Oral Med Oral Pathol. 1974;38:451–455.
- Neuvald L, Consolaro A. Cementoenamel junction: Microscopic analysis and external cervical resorption. J Endod. 2000;26:503–508.
- Hahn CL, Overton B. The effects of immunoglobulins on the convective permeability of human dentine in vitro. Arch Oral Biol. 1997;42:835–843.
- Tamse A. Vertical root fractures in endodontically treated teeth: diagnostic signs and clinical management. Endod Topics. 2006;13:84–94.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, Arockiam S, Maheswari TNU, Natanasabapathy V. Diagnosis of vertical root fractures by come beam computed tomography in root filled teeth with confirmation by direct visualization: A systematic review and meta–analysis. J Endod. 2021;47:1198–1214.
- Fayad MI, Ashkenaz PJ, Johnson BR. Different representations of vertical root fractures detected by cone-beam volumetric tomography: A case series report. J Endod. 2012;38:1435–1442.
- Fan X, Yu X, Yu S, et al. Prognostic factors of grade 2–3 endo-periodontal lesions treated nonsurgically in patients with periodontitis: A retrospective case-control study. BioMed Res. Int. 2020;2020:1–9.
- Seltzer S, Bender IB, Ziontz M. The interrelationship of pulp and periodontal disease. Oral Surg Oral Med Oral Pathol. 1963;16:1474–1490.
- Rubach WC, Mitchell DF. Periodontal disease, accessory canals and pulp pathosis. J Periodontol. 1965;36:34–38.
- Torabinejad M, Kiger RD. Histologic evaluation of dental pulp tissue of a patient with periodontal disease. Oral Surg Oral Med Oral Pathol. 1985;59:198–200.
- Mazur B, Massler M. Influence of periodontal disease on the dental pulp. Oral Surg Oral Med Oral Pathol. 1964;17:592–603.
- Bergenholtz G, Nyman S. Endodontic complications following periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol. 1984;55:63–68.
- Langeland K, Rodrigues H, Dowden W. Periodontal disease, bacteria, and pulpal histopathology. Oral Surg Oral Med Oral Pathol. 1974;37:257–270.
- Ricucci D, Siqueira JF, Rocas IN. Pulp response to periodontal disease: Novel observations help clarify the process of tissue breakdown and infection. J Endod. 2021;47:740–754.
- Simon JHS, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J Periodontol. 1972;43:202–208.
- Herrera D, Retamal-Valdes B, Alonso B, Feres M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J Clin Periodontol. 2018;45(Suppl 20):S78–S94.
From Decisions in Dentistry. April 2022;8(4)8-10, 13.


![The controversy around adding fluoride to drinking water was recently highlighted by an article in the Wall Street Journal, which addressed its possible negative neurological effects on children.[1] The article cited recent studies on what levels of fluoride are needed to protect teeth without risking possible cognitive harm to prenatal children and infants. Link in bio.
[1] Data on link.
---
#dentistry #dentist #dental #smile #dentista #teeth #cosmeticdentistry #dentistryworld #dentalphotography #odonto #tooth #dentistrylife #orthodontics #dentalcare #dentalhygienist #dentalimplants #oralhealth #veneers #dentalstudent #dentalassistant #dentalclinic #dentistlife #dentalhygiene #teethwhitening #oralsurgery #dds #endodontics #continuingeducation #education](https://decisionsindentistry.com/wp-content/plugins/instagram-feed/img/placeholder.png)