
Dental Implications of Gastroparesis
As evidenced by this case report, gastrointestinal motility disorders can have significant ramifications for oral health.
Oral health professionals should be prepared to identify clinical findings associated with diagnosed or undiagnosed gastric diseases, dietary habits and psychological disorders (such as bulimia) that may result in vomiting and reflux. Gastric fluids are composed of hydrochloric acid, which may have a pH of 1.0 to 2.0.1 These strong acids can soften enamel and dentin, increasing the risk of tooth surface loss caused by bruxing, toothbrushing, or consuming hard or abrasive foods.2 In addition to the intrinsic effects of gastric fluids, erosive tooth wear may also be related to the extrinsic dietary acids found in many foods and sugar-sweetened beverages.3 As such, when erosion is detected, oral health professionals should identify its etiology and institute behavioral and preventive strategies to manage it.4 Gastroparesis is one example of a gastric condition that can have significant oral health consequences. In order to help guide clinicians toward effective management strategies, this article presents a case study of erosive tooth wear attributed to this condition.
Gastroparesis is a chronic gastrointestinal motility disorder characterized by delayed gastric emptying;5 patients experience partial paralysis of the stomach, which results in food retention in the stomach for extended periods. Symptoms include nausea, vomiting and bloating.5,6 Patients with gastric disorders who seek medical treatment are provided with dietary counseling and may be prescribed medications to alleviate symptoms. When taking medical histories, oral health professionals should ask if the patient has been diagnosed with gastroparesis or other gastric disorders in order to plan appropriate treatment.7
CASE REPORT
For example, the medical history of a woman with the chief complaint of extremely sensitive teeth revealed a diagnosis of gastroparesis. The patient was taking esomeprazole and omeprazole, both of which are proton pump inhibitors that suppress production of gastric acids. In addition to the pain and functional difficulties her dentition was causing, the patient was self-conscious about her smile (Figure 1). A comprehensive examination revealed erosion with dentin exposure, staining, decalcification, noncarious cervical lesions and gingival recession. These were noted in her record. The patient’s gingival display was adequate and within normal limits. A caries risk assessment was completed and, due to low salivary pH and hyposalivation, her risk level was deemed high.

A treatment plan was formulated and discussed with the patient. A diagnostic wax-up of the proposed occlusal scheme was completed (Figure 2). Oral hygiene instructions were presented. The patient was prescribed a high-fluoride toothpaste and given xylitol mints and oral spray containing a pH-neutralizing agent.8 The patient was also counseled about dietary habits. Additionally, the oral side effects of her gastroparesis medications — including decreased salivary flow leading to xerostomia — were discussed.

composite onlays were placed at the
new vertical dimension of occlusion.
After reevaluating the patient’s caries risk level, an esthetic treatment plan was formulated. Lithium disilicate onlays were planned for teeth #18, #19, #20 and #29. Lithium disilicate crowns were planned for teeth #21, #28, #30 and #31. These all-ceramic crowns have high success rates.9 Composite buildups were planned for teeth #22 through #27. Because the patient’s periodontal condition was stable, with no biologic width problems, crown lengthening and gingivectomy were not required. The decision was made to increase the vertical dimension of occlusion due to the loss of tooth structure during conservative preparation.10
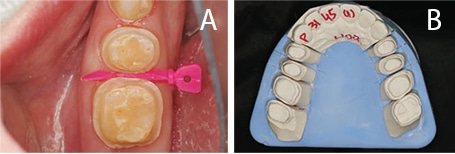
The patient accepted the proposed treatment plan. A smile design was completed based on the wax-up, and the patient was eager to begin treatment. Before preparing the teeth, the patient was placed in temporary splinted composite overlays at the new vertical dimension of occlusion (Figure 3 and Figure 4). The patient adapted well to these changes.

With the new vertical dimensions of occlusion, the maxillary anterior teeth were prepared for crowns. Anterior teeth #6 to #11 were prepared, impressed and temporized for lithium disilicate restorations. At the next appointment, lithium disilicate crowns were applied to teeth #6 through #11. The patient indicated she was pleased with the esthetic result. At the following appointments, posterior quadrants were prepared and restored sequentially, using bonded lithium disilicate onlays and crowns (Figures 5A and 5B; Figures 6A through 6C). Composite buildups were completed on the lower anterior teeth #22 through #27. The treatment eliminated the patient’s dentinal hypersensitivity and improved oral function and appearance (Figures 7A and 7B).

DISCUSSION AND CONCLUSION
As noted, dental professionals should be able to identify dental erosion and erosive tooth wear,11,12and be adept at recognizing the signs of dental erosion, determining the etiology, and discussing clinical findings with patients. Sensitive findings in the medical history, such as the effects of eating disorders (e.g., anorexia or bulimia), should be handled cautiously.7 Patients who are unaware that gastric acid may cause erosion should be referred to their physician for additional diagnostic testing. Patients should also be educated about the risks acid reflux poses to oral and systemic health. In cases in which it is determined that erosive tooth wear is due to dietary habits, patients should be advised to limit their intake of acidic foods and beverages.13 They need to understand that it is far better to manage tooth surface loss early, as opposed to taking a “wait-and-watch” approach that may lead to more extensive and expensive restorative dentistry.
These patients should be placed on a frequent recare schedule that includes regular caries risk assessment, monitoring of dietary acid intake, and reinforcement of preventive strategies. This will help to support patients’ oral health, as well as restoration stability and longevity.
Even though the etiology of dental erosion is multifactorial, clinicians should be able to identify possible causes and discuss these with patients. Oral health professionals should also work with patients’ physicians to ensure appropriate counseling and treatment. In addition to managing erosive tooth wear, it is important for dental team members to understand the need to educate patients about the causes of erosion — and what can be done to prevent its potentially damaging oral health consequences.
KEY TAKEAWAYS
- Whether the result of gastric disease, dietary habits or psychological disorders (such as bulimia), the introduction of gastric acids into the oral cavity can have negative ramifications for oral health.
- Potential consequences include softening of enamel and dentin that increases the risk of tooth surface loss caused by bruxing, aggressive toothbrushing, or consuming hard or abrasive foods.2
- When erosion is detected, oral health professionals should seek to identify its etiology, and institute behavioral and preventive strategies to manage it.4
- When taking medical histories, dental professionals should ask if the patient has been diagnosed with gastric disorders in order to plan effective treatment.7
- As appropriate, patients who are unaware that gastric acid may cause erosion should be referred to a physician for additional diagnostic testing. Patients should also be advised about the risks acid reflux poses to oral and systemic health.
- These patients should be placed on a frequent recare schedule that includes regular caries risk assessment, monitoring of dietary acid intake, and reinforcement of preventive strategies.
ACKNOWLEDGEMENT
The authors would like to thank Susan Do, DDS, for providing the images.
REFERENCES
- Moazzez R, Bartlett D. Intrinsic causes of dental erosion. Monogr Oral Sci. 2014;25:180–196.
- Ranjitkar S, Smales RJ, Kaidonis JN. Oral manifestations of gastroesophageal reflux disease. J Gastroenterol Hepatol. 2012;27:21–27.
- Barbour ME, Lussi A. Erosion in relation to nutrition and the environment. Monogr Oral Sci. 2014;25:143–154.
- Lussi A, Caravalho TS. Erosive tooth wear. A multifactorial condition of growing concern and increasing knowledge. Mono Oral Sci. 2014;25:1–15.
- Camilleri M, Grover M, Farrugia G. What are the important subsets of gastroparesis? Neurogastroenterol Motil. 2012;24:597–603.
- Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L, American College of Gastroenterology. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108:18–37.
- Lussi A. Dental erosion clinical diagnosis and case history taking. Euro J Oral Sci. 1996;104:191–198.
- Bellamy R, Harris R, Date RF, et al. In situ clinical evaluation of a stabilized stannous fluoride dentifrice. Int Dent J. 2014;25:197–205.
- Christensen GJ. The all-ceramic restoration dilemma: where are we? J Am Dent Assoc. 2011;142:668–671.
- Spear FM, Kokich VG, Marhew D. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137:160–169.
- Barbour M, Lussi A, Shellis R. Screening and predication of dental erosion. Caries Res. 2011;45(Suppl 1):24–32.
- Hellwig E, Lussi A. Oral hygiene products, medications and drugs — hidden etiologic factors for dental erosion. Monogr Oral Sci. 2014;25:155–162.
- Cochrane NJ, Cai F, Yuan Y, Reynolds EC. Erosive potential of beverages sold in Australian schools. Aust Dent J. 2009;54:238–244.
The authors have no commercial conflicts of interest to disclose.
Featured photo by ERAXION/ISTOCK/ GETTY IMAGES PLUS
From Decisions in Dentistry. February 2017;3(2):28–31.




