
Customized Retention Strategies in Orthodontics
Tips for preserving treatment outcomes and achieving long-term stability.
In orthodontics, retention is key to maintaining the ideal esthetics and function established during the active phase of treatment. Through the active phase, periodontal ligament (PDL) fibers are stretched as the dentition is moved. Following the active phase, these fibers want to release their tension and bring the dentition back to its original housing. This is called relapse. Orthodontic providers are charged with creating a customized retention protocol for each patient and addressing the common causes of relapse. Many factors affect the likelihood of relapse, including the initial diagnosis and malocclusion, stability of orthodontic movements used in treatment, prescribed retention devices, and patient compliance. Orthodontic relapse has biological, treatment-related, and patient-specific etiologies.
Biological factors related to orthodontic relapse include the influence of the PDL fibers, forces from surrounding muscles such as the cheeks and tongue, and remaining growth.1 After the teeth are moved orthodontically, the gingiva must remodel to the new position of the teeth. As the elastic, dentogingival, and interdental fibers can take 8 months or more to remodel, stabilizing the teeth in their final positions is critical during this time. To help prevent relapse caused by gingival fibers, a supracrestal circumferential fiberotomy, a gingival surgery in which these fibers are severed, may be performed.2 The teeth must also be placed in a way that the pressures from the cheeks and tongue are balanced. This is to ensure that unequal forces are not pushing teeth in one direction or another. If the lower incisors are proclined or retroclined excessively, for example, the musculature is likely to cause the teeth to relapse if not retained properly. The balance in muscle forces may change over an individual’s lifespan, thus affecting their relapse likelihood with age.2
Additionally, the relationships of the jaws to each other may change with age, which can also affect treatment results. This is particularly common with Class III skeletal patients who may have late mandibular growth and “outgrow” their treatment.2 Patients presenting with deep bites, anterior open bites, and extreme vertical facial patterns may require special consideration.2
Treatment and Patient-Related Factors
Some orthodontic movements have more long-term stability than others. Thus, success of retention also depends on treatment-related factors and their associated stability. Some argue that finishing with an ideal occlusion is more likely to be stable long term, but there is no substantial evidence to support this.2 However, if teeth become mobile through traumatic occlusion or gross interferences not corrected during treatment, this may contribute to relapse.
Excessive proclination or retroclination of the lower incisors and any expansion of the lower arch are movements known to be less stable. In particular, the intercanine width may relapse due to soft tissue pressures.2 The goals of treatment should include obtaining a proper occlusion, an esthetic result, and, most important, a stable result.
Patient-specific factors, including patient’s original malocclusion, individual habits, and compliance with retainer wear, play an important role in the long-term stability of the orthodontic result.1 In one study, a microelectronic sensor was used to study retainer wear time in patients with and without a mobile app encouraging retainer wear. At 12 months, wear time was low in both groups (median 3.09 hours/day in the intervention group and median 1.44 hours/day in the control group).3 Thus, due to the numerous biological and treatment-related factors that may cause relapse if the teeth are not retained properly, low compliance with retainer wear can put patients at risk for relapse.
Types of Retention
Once desired occlusion, function, and esthetics are established from the active phase of orthodontic treatment, relapse of the original malocclusion must be prevented. The three main forms of retention include Hawley, Essix or thermoplastic, and bonded fixed retainers.
The most commonly used appliances are the Hawley and Essix retainers (Figure 1). The Hawley retainer is removable and fabricated from acrylic resin and wire.4,5 It consists of a palatal acrylic base with clasps and a labial arch wire4 that must occasionally be adjusted and tightened for patient comfort and retention. Highly durable, the Hawley retainer can be adjusted to achieve small tooth movements.
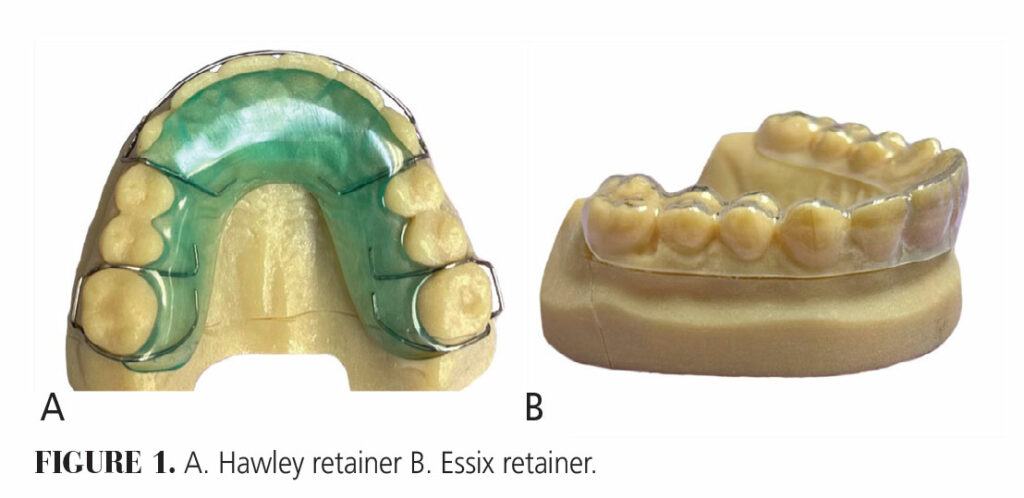 The Essix retainer is growing in popularity due to its clear esthetics, lower cost, and ease of cleaning. Furthermore, the Essix retainer can be quickly made in house, eliminating the need to send to a lab. These retainers are made by heating a thermoplastic sheet and compressing it inside a vacuum over a patient’s mold.4 Many practices will now choose to use in-house three-dimensional printed models to produce Essix retainers.
The Essix retainer is growing in popularity due to its clear esthetics, lower cost, and ease of cleaning. Furthermore, the Essix retainer can be quickly made in house, eliminating the need to send to a lab. These retainers are made by heating a thermoplastic sheet and compressing it inside a vacuum over a patient’s mold.4 Many practices will now choose to use in-house three-dimensional printed models to produce Essix retainers.
Studies have compared Hawley and Essix retainers. Mai et al6 found no significant differences in changes to intercanine and intermolar widths between patients using Hawley and Essix retainers during follow-up. When comparing occlusal contacts, the number of occlusal contacts with Hawley retainers was significantly more than with Essix retainers, especially in the posterior. This makes sense, as Hawley retainers do not cover the occlusal surface.
In terms of patient compliance and management, a study by Hichnes et al5 found that patients were less embarrassed and more likely to wear Essix retainers compared to Hawley retainers. Another study found that patients had a harder time with speech articulation with the Hawley retainer.6 These factors should be considered if esthetics and phonetics are significant patient concerns. In the end, a good retention protocol is one that will be worn.
Fixed retainers are another type of retention used on incisors either with or without a retainer. They can be used on the upper or lower anterior segments but use on the maxilla requires careful positioning to avoid interferences. Different wires can be used and cured to the teeth with composite. Fixed retainers have several advantages including better esthetics, no patient compliance, and durability. Disadvantages include precision of bonding that is technique sensitive and oral hygiene concerns.7
When providers are deciding whether to include a fixed bonded retainer in their retention strategy, the prior malocclusion should be evaluated. Malocclusions that include, but are not limited to a diastema, generalized spacing, severe crowding, and prior incisor rotations may warrant fixed lingual retainers.7 Many patients find ease of mind with fixed retainers, but patients must understand that these wires only hold teeth in a two-dimensional plane, and that they can break without their knowledge. To maintain proper retention, an Essix or Hawley should be worn on top.
Orthodontic retention is critical to preserve the final occlusion obtained through orthodontic treatment and to avoid relapse. Many factors affect the likelihood of relapse and numerous appliances are utilized for retention. While each type has certain benefits and drawbacks, determining which retainer a patient is most likely to wear is critical.
References
- Jedliński M, Grocholewicz K, Mazur M, Janiszewska-Olszowska J. What causes failure of fixed orthodontic retention? – Systematic review and meta-analysis of clinical studies. Head Face Med. 2021;17:32.
- Martin C, Littlewood SJ, Millett DT, et al. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev. 2023;5:CD002283.
- Zhang X, Al-Moghrabi D, Pandis N, Shah S, Fleming PS. The effectiveness of a bespoke mobile application in improving adherence with removable orthodontic retention over 12 months: A randomized controlled trial. Am J Orthod Dentofacial Orthop. 2022;161:327-337.
- Lyros I, Tsolakis IA, Maroulakos MP, et al. Orthodontic retainers—a critical review. Children (Basel). 2023;10:230.
- Hichens L, Rowland H, Williams A, et al. Cost-effectiveness and patient satisfaction: Hawley and vacuum-formed retainers. Eur J Orthod. 2007;29:372-378.
- Mai W, He J, Meng H, et al. Comparison of vacuum-formed and Hawley retainers: a systematic review. Am J Orthod Dentofacial Orthop. 2014;145:720-727.
- Kartal Y, Kaya B. Fixed orthodontic retainers: a review. Turk J Orthod. 2019;32:110-114.
From Decisions in Dentistry. October/November 2024;10(6):14-15.


