TRAFAWMA/ISTOCK/GETTY IMAGES PLUS
TRAFAWMA/ISTOCK/GETTY IMAGES PLUS
Comparing Three Ceramic Materials for Digital Dentistry
Lithium disilicate, zirconia, and resin-matrix ceramic materials present three viable options for digitally based restorative dentistry.
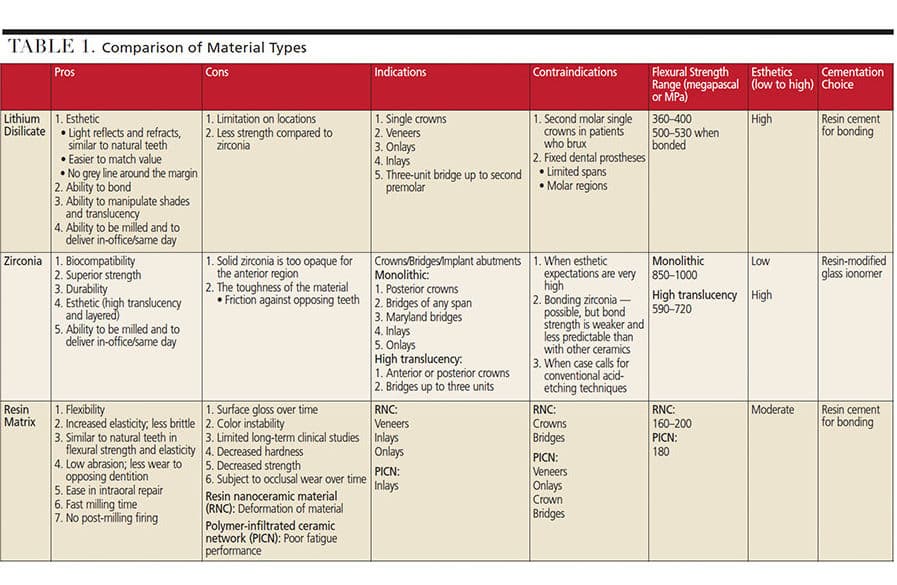
Interest in digital dentistry has been a driving force in the increased use of computer aided design/computer aided manufacturing (CAD/CAM) technology in dental practice. As digital dentistry and CAD/CAM become more prevalent, it is imperative to understand the properties and comparisons of crowns fabricated in this manner. This article will discuss three ceramic materials used in CAD/CAM applications in terms of strength and esthetics, as well as the pros and cons of each option (Table 1).
LITHIUM DISILICATE
Porcelain-fused-to-metal (PFM) crowns have been the standard for full coverage crowns for many decades; however, with the increased demand for esthetics, all-ceramic crowns have become one of the most popular material choices. Research indicates all-ceramic crowns have a better gingival response and higher esthetic quality than conventional PFMs.1 With multiple options to choose from, proper material selection becomes a key factor in restorative dentistry. Among the various types of all-ceramic crowns, studies show that lithium disilicate crowns offer strength and high esthetics.
Lithium disilicate is a glass ceramic and one of the most popular CAD/CAM materials currently in use. More translucent than zirconia, lithium disilicate’s translucency2 and optical properties3 support highly esthetic indications. Crowns with greater translucency will appear similar to natural teeth, which is essential in esthetic cases. In addition, lithium disilicate crowns show a 10-year survival rate of 96.7%4 and demonstrate a complication rate on the loss of pulp vitality after five years of 2%, which is similar to metal-ceramic crowns.5 However, studies have noted that failures of lithium disilicate crowns were mostly from the posterior region. Another limitation is the abrasion of opposing enamel. While ceramic will abrade the opposing enamel more than metal, there are studies noting that polishing with a fine diamond bur after adjustment can minimize this deleterious effect.6 Despite its potential limitations, lithium disilicate seems to be a good material choice with proper case selection, especially given its high esthetic quality.
Lithium disilicate crowns can be fabricated with either conventional (lost-wax hot-pressing technique) or CAD/CAM processes. Furthermore, there are various ways to fabricate lithium disilicate crowns utilizing CAD/CAM technology: dentists can take a digital impression and mill the restoration in the office (or send to the lab for milling); alternately, they can send the digital impression for pressing at the lab.
These restorations have similar flexural strengths whether milled or pressed: 360 megapascal (MPa) for milled and 400 MPa for pressed. Additionally, one study showed no significant marginal gap difference between lithium disilicate crowns made with vinyl polysiloxane impression/milling, digital impression/pressing, or digital impression/milling.7 Another study comparing heat-pressed lithium disilicate with milled restorations also showed no difference in marginal gaps.8 Both pressed and CAD/CAM-milled crowns can provide good marginal fit, but this depends on the smoothness of the margin prep. One consideration is that milled crowns require smooth margins because milling burs are unable to replicate the roughness or discrepancy of the prep at the margin. One remedy is to have a proper prep design and smooth margins. Lastly, a multilayer block with different translucencies can be used to mill a restoration with superior esthetics. This means clinicians can provide a variety of in-office crown options using CAD/CAM technology based on esthetics.
Overall, lithium disilicate crowns provide an alternative to PFMs. They offer high esthetic quality, adequate strength, and the ability to deliver in-office crowns utilizing CAD/CAM technology. It is important to note, however, that tooth location and prep design become key factors in a successful outcome when choosing this type of material.
ZIRCONIA
The ever-increasing emphasis on esthetics has been instrumental in the ongoing search for materials that have enough strength to replace the metal that was previously used for dental restorations. As esthetic demands grow, deciding which material to choose becomes a critical factor in digital dentistry. Many providers are now considering zirconia restorations over conventional PFM restorations.
Zirconia was introduced in prosthetic dentistry, in combination with CAD/CAM techniques, for the fabrication of crowns and fixed partial dentures. It is utilized in various clinical situations due to its biocompatibility, hardness, fracture resistance and esthetics when compared to traditional metal-ceramic restorations.9 Zirconium oxide is a white crystalline oxide of zirconium, which is a metal with properties similar to titanium. The zirconia used in the production of hard dental ceramics is partially stabilized with yttrium oxide.
One of the significant advantages of zirconia is that it inhibits crack propagation in dental restorations through a process known as phase transformation toughening. Zirconia restorations can absorb a crack’s energy by transforming from the tetragonal crystalline phase to the more stable monoclinic phase, effectively stopping crack propagation.10
Clinically, zirconia may be chosen due to its excellent strength and mechanical properties, durability and excellent esthetics (in some forms). Additionally, less tooth preparation is needed for zirconia restorations — both occlusally and axially — compared to PFM preparations. Moreover, there is lower wear potential on the antagonist teeth with zirconia.11 Yttria-stabilized zirconia achieves its full strength after sintering (baking) and can reach an average biaxial flexural strength of 850 MPa to more than 1000 MPa. These restorations can be fabricated from solid full-contour zirconia, the more esthetic, high translucency (HT) zirconia, or porcelain layered zirconia. Solid full-contour zirconia or monolithic zirconia tends to be opaque, which is why it is usually reserved for posterior restorations. However, all zirconia crowns, regardless of type, are highly biocompatible.12,13
Monolithic zirconia crowns are fabricated entirely of the zirconia ceramic, with no porcelain layered over the core material. These monolithic zirconia crowns are highly effective in masking discolored dental preparations, such as those that have darkened due to previous dental treatments (including post-and-core or restored dental implants). Moreover, monolithic zirconia contains more stabilizers than HT zirconia, so it does a slightly better job of resisting the forces of occlusion — which is why it is particularly suitable for patients who brux.14 Additionally, monolithic crowns tend to be opaque and lack the translucency and fluorescence of HT zirconia restorations. For esthetic reasons, most dentists utilize the monolithic zirconia crowns for non-esthetic areas.
Although weaker than solid zirconia, HT zirconia (at 590 MPa to 720 MPa or higher) is stronger than PFM restorations and still maintains natural and vibrant translucency. Unlike solid opaque and monochromatic zirconia, HT zirconia is suitable for anterior crowns due to its more translucent and opalescent characteristics. In addition, porcelain layered zirconia provides similar esthetic quality as HT zirconia — however, the weak link in a layered zirconia crown is the layered porcelain, which has a flexural strength of approximately 100 MPa. Because monolithic HT zirconia does not incorporate vulnerable layered porcelain, it is stronger than porcelain fused to any substructure material, whether a metal or all-ceramic system. In addition, fabrication of HT zirconia crowns is a less complicated procedures compared to the production of layered zirconia, such as multilayered restorations utilizing opaque zirconia cores with a translucent feldspathic veneering.
Improved tooth-matching materials, such as the new translucent HT zirconia, have been developed to offer high strength and good esthetics.9 However, the effects of altering material constituents to increase translucency needs to be further evaluated in terms of physical properties, including phase transformation and low temperature degradation.
All-ceramic prostheses are now replacing metal-based restorations, and the consistency of prefabricated CAD/CAM ceramic blocks may surpass manually processed ceramics. With the development of CAD/CAM systems in restorative dentistry, high-strength zirconia can now be used for fabrication of various prostheses, including crowns, fixed partial dentures, posts and cores, implants and implant abutments.
With CAD/CAM technology, dentists have the ability to mill zirconia, which gives patients more options for an all-ceramic zirconia restoration that can be fabricated in-house or digitally sent to the lab for fabrication.
Advances in dental CAD/CAM technology have been crucial in the development of high-strength dental ceramics, and the mechanical properties of zirconia-based ceramics are the highest ever reported for a dental ceramic. Clinicians should bear in mind, however, that while yttria-stabilized zirconia is an extremely hard material, the published clinical data is somewhat limited at this time.
RESIN-MATRIX CERAMICS
In the search for a CAD/CAM restorative that mimics both enamel and dentin in esthetics and physical properties, dental material scientists have created a diverse class of ceramics. The newest materials being developed contain various combinations of ceramics and resin composites — and these are designated as hybrid ceramics, resin nanoceramics (RNC), resin-matrix ceramics, polymer-infiltrated ceramic networks (PICN), and nanoceramic resin hybrids. The goal of resin-matrix ceramics is to incorporate the advantages of glass ceramics and composites in one material.
Among the advantages of glass ceramics are durability, color stability and biocompatibility, which are all desirable properties in a CAD/CAM restorative. However, the disadvantages — such as tendency to fracture, abrasion of the opposing dentition, and difficulty in intraoral repair — have increased interest in incorporating composite resin into the glass ceramic. The advantages of composite resin — including ease of repair, low abrasion to opposing dentition, and polishability — can complement glass ceramics. However, the disadvantages of composite resin compared to glass ceramics, including low durability, color instability over time, and inferior mechanical properties, are not desirable in a CAD/CAM material. Therefore, combining glass ceramics with resin would create synergistic effects that would closely mimic natural dentition, providing operators with another useful option for digital dentistry.15–18 While there are no long-term clinical studies on any of the resin-matrix ceramic materials, some early research has been conducted on this class of materials.
As noted, one of the resin-matrix ceramics is RNC, which contains silica, zirconia and agglomerated nano-sized particles of silica and zirconia embedded in a cross-linked polymer matrix. One of its advantages is quality similar to glass ceramics. For instance, onlays of this material were deemed equal in performance with glass ceramic onlays over a five-year period.15 These resin-matrix ceramics mill faster and with less margin chipping, which increases the service life of the milling unit’s diamond burs. Another possible advantage is the wear rate of this resilient ceramic approaches the wear rate of adhesive resin cement, which means margin integrity might be better maintained over time. It was also noted that due to differences in its elastic properties, RNC is less brittle, less prone to fracture, and more flexible than glass ceramics. Its greater resilience was attributed to its ability to accommodate more stress absorption by way of deformation.
Other studies have noted that while lithium disilicate offers greater bond strength, the advantages of resin-matrix ceramics include less abrasion to the opposing dentition and decreased chairtime because there is no need for oven sintering.16,19 To recap, this new generation of polymer-based materials combines the advantages of ceramics (durability and color stability) with those of composite resins (elasticity and low abrasiveness to the opposing dentition).15,16
Another resin-matrix ceramic discussed in the literature is PICN, which contains inorganic and organic components in a ceramic network, with reinforcement of a acrylic polymer network resin. As with all resin-matrix ceramics, PICN material must also be placed with a bonded resin cement.20 This material exhibits durability and color stability comparable to glass ceramics, with more resiliency and smoother margins than glass ceramics.16 As with other resin-matrix ceramics, esthetics are comparable to glass ceramics in the first year. In a study that compared it to other resin-matrix and ceramic materials, PICN was shown to be least resilient under fatigue.17
Practically speaking, the primary disadvantage of resin-matrix ceramics is the lack of long-term clinical studies. In light of their rapid evolution, fully evidence-based practice is not currently possible with these materials. Although PICN offers the advantages of durability, color stability and flexural strength, as previously noted this material’s fatigue performance is low compared to other CAD/CAM restoratives. Another study that compared the durability of RNC to acid found that RNC was less acid-resistant than a glass ceramic.21 This highlights the fact that more long-term clinical studies, in-vitro studies, and studies on new materials are needed. Other resin-matrix ceramics also seem to have issues, partially due to the different combinations of components, and thus completely different mechanical properties.
Although lithium disilicate is superior to these materials with respect to fracture load, flexural strength and hardness, RNC and PICN may be considered because their elastic modulus is similar to natural teeth.18 From the available research, it can be extrapolated that resin-matrix restorations are easier to repair intraorally than glass ceramics because of the possibility of using composite as a repair material (as opposed to complete replacement of the restoration). Additionally, resin-matrix ceramics can exhibit more flexibility than glass ceramics, making them easier to handle and less prone to fracture.
CLOSING THOUGHTS
In digital dentistry, current materials — such as lithium disilicate and zirconia, with their specific advantages and disadvantages — provide great choices for various clinical situations. As more materials are developed and refined, resin-matrix ceramics may become a regular option for single-tooth cases involving veneers, inlays and onlays. With the introduction of resin-matrix ceramics, the ultimate goal is to create a CAD/CAM block that can produce restorations closely mimicking natural dentition — a development that would allow practitioners to have an array of options to best address each patient’s needs.
KEY TAKEAWAYS
- As digital dentistry and computer aided design/computer aided manufacturing (CAD/CAM) become more prevalent in dental practice, it is imperative for clinicians to understand the advantages and disadvantages of various restorative materials.
- With multiple options to choose from, material selection becomes a key factor in successful restorative outcomes.
- More translucent than zirconia, lithium disilicate’s translucency2 and optical properties3 support highly esthetic indications.
- Lithium disilicate crowns can be fabricated with either conventional (lost-wax hot-pressing technique) or CAD/CAM processes.
- Compared to traditional metal-ceramic restorations, zirconia is utilized in various situations due to its biocompatibility, hardness, fracture resistance and esthetics.9
- One of the advantages of zirconia is that it inhibits crack propagation through a process known as phase transformation toughening.
- The newest digital restorative materials being developed contain various combinations of ceramics and resin composites.
- This new generation of polymer-based restoratives combines the advantages of ceramics (durability and color stability) with those of composite resins (elasticity and low abrasiveness to the opposing dentition).15,16
REFERENCES
- Sadowsky S. An overview of treatment considerations for esthetic restorations: a review of the literature. J Prosthet Dent. 2006;96:433–442.
- Kurtulmus-Yilmaz S, Ulusoy M. Comparison of the translucency of shaded zirconia all-ceramic systems. J Adv Prosthodont. 2014;6:415–422.
- Mizrahi B. The anterior all-ceramic crown: a rationale for the choice of ceramic and cement. Br Dent J. 2008;205:251–255.
- Pieger S, Salman A, Bidra A. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 2014;112:22–30.
- Pjetursson B, Sailer I, Zwahlen M, Hämmerle C. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implan Res. 2017;18:73–85.
- Lawson N, Janyavula S, Syklawer S, McLaren EA, Burgess J. Wear of enamel opposing zirconia and lithium disilicate after adjustment, polishing and glazing. J Dent. 2014;42:1586–1591.
- Anadioti E, Aquilion S, Gratton D, et al. 3D and 2D marginal fit of pressed and CAD/CAM lithium disilicate crowns made from digital and conventional impressions. J Prosthodont. 2014;23;610–617.
- Hamad K, Rashdan B, Omari W, Baba N. Comparison of the fit of lithium disilicate crowns made from conventional, digital, or conventional/digital techniques. J Prosthodont. 2019;28:e580–e586.
- Ghodi S, Jafarian Z. A review on translucent zirconia. Eur J Prosthodont Restor Dent. 2018;26:62–74.
- Tinchert J, Zwez D, Maerx R, Anusavice KJ. Structural reliability of alumina-, feldspar-, leucite-, mica- and zirconia-based ceramics. J Dent. 2000;28:529–535.
- Filser F, Kocher P, Weibel F, Lüthy H, Schärer P, Gauckler LJ. Reliability and strength of all-ceramic dental restorations fabricated by direct machining (DCM). Int J Comput Dent. 2004;4:89–106.
- Shahmiri R, Standard OC, Hart JN, Sorrell CC. Optical properties of zirconia ceramic for esthetic dental restorations: a systemic review. J Prosthet Dent. 2018;119:36–46.
- Saridan S, Tak O, Alniacik G. Basic properties and types of zirconia: an overview. World J Stomatol. 2013;2:40–47.
- Mormann WH, Stawarczyk B, Ender A, Sener B, Attin T, Mehl A. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: two-body wear, gloss retention, roughness and Martens hardness. J Mech Behav Biomed Mater. 2013;20:113–125.
- Fasbinder DJ, Neiva GF, Heys D, Heys R. Clinical evaluation of chairside computer assisted design/computer assisted machining nano-ceramic restorations: Five-year status. J Esthet Res Dent. August 8, 2019. [Epub ahead of print.]
- Awada A, Nathanson D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent. 2015;114:587–593.
- Venturini AB, Prochnow C, Pereira GK, Segala, RD, Kleverlaan CJ, Valandro LF. Fatigue performance of adhesively cemented glass-, hybrid- and resin-ceramicmaterials for CAD/CAM monolithic restorations. Dent Mater. 2019;35:534–542.
- Albero A, Pascual A, Camps I, Grau-Benitez M. Comparative characterization of a novel CAD/CAM polymer-infiltrated-ceramic-network. J Clin Exp Dent. 2015;7:e495–e500.
- Zimmermann M, Koller C, Reymus M, Mehl A, Hickel R. Clinical evaluation of indirect particle-filled composite resin CAD/CAM partial crowns after 24 months. J Prosthodont. 2018;27:694–699.
- Awad MM, Albedaiwi L, Almahdy A, et al. Effect of universal adhesives on microtensile bond strength to hybridceramic. BMC Oral Health. 2019;19:178.
- Colombo M, Poggio C, Lasagna A, Chiesa M, Scribante A. Vickers micro-hardness of new restorative CAD/CAM dental materials: evaluation and comparison after exposure to acidic drink. Materials (Basel). 2019;12:1246.
The authors have no commercial conflicts of interest to disclose.
From Decisions in Dentistry. February 2020;6(2):12–14,16.