Assessing and Managing Pediatric Xerostomia Risk
While not traditionally noted as high risk for xerostomia, young patients are more commonly experiencing medical conditions and medication use that increase susceptibility to dry mouth.
This course was published in the March 2023 issue and expires March 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 430
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss risks for xerostomia in the pediatric population.
- Identify conditions that may increase the risk for xerostomia in young patients.
- Explain xerostomia risk assessment tools for use in dental settings.
Dry mouth is the subjective sensation of xerostomia, a well-recognized occurrence in adults. Associated with plaque buildup, caries, gingivitis and periodontitis, dry mouth is often underreported by patients and underrecognized by practitioners.1,2 Xerostomia receives relatively little attention among young adults and is only now being seriously considered as important in the pediatric population.3,4 Children at elevated risk for xerostomia often have medical conditions affecting salivary production, take medications with xerostomic adverse effects, and engage in school and extracurricular activities in which dehydration is likely.3
Xerostomia is related to periodontal disease and caries through overcolonization of bacterial plaque.4,5 These conditions are worsened by the consumption of candies and sugary drinks to maintain moisture, common among those with dry mouth.5 Lack of saliva predisposes the young patient to oral infection. In addition, low bacterial clearance increases plaque formation and reduces neutralization of the acidic oral environment. Historically, plaque buildup was associated with poor self-care; however, xerostomia may be due to medical conditions and/or medication use.
Clinical signs of xerostomia include caries lesions or decalcification on the labial surface of maxillary incisors due to cervical plaque accumulation, low oral pH, and lack of movement of the salivary film.3 The subjective nature of xerostomia makes it difficult to identify through standardized measures, such as salivary flow rates. Thus, it is typically identified in children through questions and clinical evaluation.
Young patients may present with xerostomia due to an increase in the prevalence of asthma, diabetes, autoimmune diseases, cancer, psychiatric conditions (e.g., anxiety, depression, schizophrenia, bipolar disorders or attention deficit disorders), and seizure disorders. The medications prescribed for these conditions often include xerostomia as a side effect. Because xerostomia may be a causative factor for oral conditions such as gingivitis and caries in young patients, it should be recognized and managed as part of an oral care plan. Xerostomia results from lower quantity and/or quality of saliva due to dehydration, mouth breathing, and/or hypofunction or dysfunction of salivary glands.1,3,4,6
ASTHMA
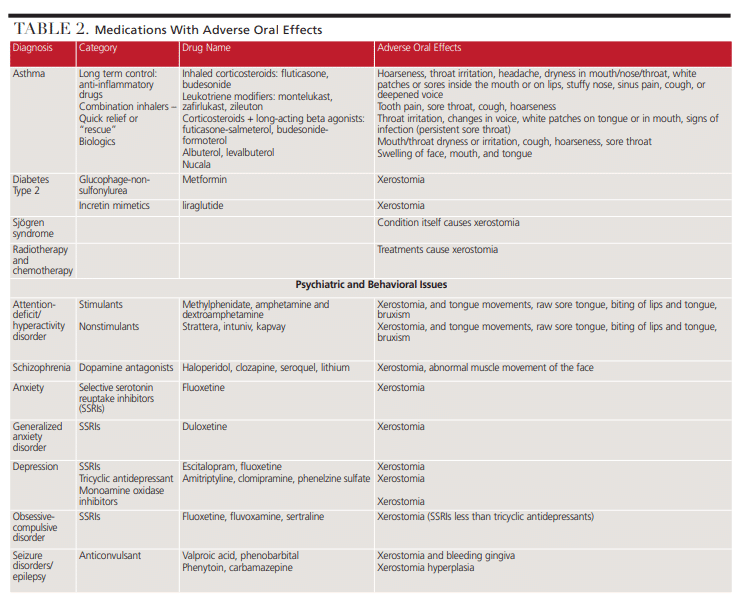
According to 2019 data, 7 million children in the United States have asthma,7 and the medications used to control it often provide a combination of long-term management and quick relief. Unfortunately, they may have adverse effects beyond xerostomia, including candidiasis, ulcerations and taste change.8,9 Dental providers should ensure young patients and their parents and/or caregivers are aware of how to use these medications properly to reduce negative impacts on oral health.
Long-term asthma medications include inhaled corticosteroids that function as anti-inflammatories and leukotriene modifiers that reduce the effects of the body’s leukotriene release in response to allergens. Combined drugs include inhaled corticosteroids with a long-acting beta-2 agonist, which last at least 12 hours by acting on the smooth muscles of the airways to keep them open. Short-acting quick-relief or rescue medications are bronchodilators (which last up to four hours).8,9 These have topical effects on the mucosa and present a risk for oropharyngeal candidiasis and pseudomembranous lesions. Long-term use of beta-2 agonists reduces salivary output by the parotid and other glands, decreasing the production of antibacterial components and increasing plaque colonization and growth.10
TYPE 2 DIABETES
Type 2 diabetes is becoming more common in young children and teens and is associated with an increase in obesity that drives insulin resistance. It is often diagnosed during the teen years when hormonal changes make it more difficult for cells to utilize insulin.11 Individuals with diabetes are prone to dehydration. Hyperglycemia can produce dry mouth, as can impaired kidney function from prolonged high glucose levels and prescribed medications.12
The treatment of choice for type 2 diabetes includes lifestyle modification and improved diet. If medication is required, metformin and liraglutide are approved for children. Glucophage-non-sulfonylurea will reduce liver glucose and help cells use insulin more effectively.13 Liraglutide assists the pancreas in releasing insulin when glucose levels are high. Because dry mouth and throat irritation may be indications of possible thyroid tumors and cancer, an examination of the lower anterior neck region should be performed at each visit and questions should be asked about dryness or irritation of the throat.14
SJÖGREN SYNDROME
Sjögren syndrome is a chronic autoimmune disease that significantly affects salivary gland production. Primary Sjögren syndrome (without other underlying illness) is usually diagnosed during middle age, yet 1% to 5% of adults with the disease report the onset of symptoms before age 12.15,16 Therefore, a simple screening of teens for parotid gland enlargement and questions about dry eyes and mouth would alert providers to the possibility.
RADIOTHERAPY AND CHEMOTHERAPY
While radiation doses during radiotherapy for pediatric head and neck tumors are much lower than those used in adults, they still affect the parotid, submandibular and minor salivary glands. This results in lower salivary function, contributing to poor oral hygiene, a tendency toward oral infections and pain, and difficulty chewing and swallowing. Reduced salivary function usually occurs within a week of treatment initiation and persists after treatment has ceased. It can take up to two years to recover if the damage is not too severe. Dry mouth can be reduced if the parotid and/or one submandibular gland is protected from radiation.17
Leukemias account for 28% of all cancers in children.18 Chemotherapy in children for acute lymphoblastic leukemia and acute myeloid leukemia can damage salivary glands due to the changes in the lining of the oral cavity and salivary glands. Salivary flow rates and changes in composition contribute to the feelings of dry mouth and the increase in adverse oral effects. Symptoms of xerostomia can range from slight to severe, and may make it difficult to speak. These symptoms can last a year or more. If a patient has chemotherapy on cycles (as is common with most cancers), it will allow some time for tissue recovery.17–19
PSYCHIATRIC AND BEHAVIORAL ISSUES
Up to 60% of inpatient pediatric psychiatric patients have xerostomia, yet few studies address these needs.5 Psychiatric conditions themselves can affect the quality and quantity of saliva. Patients ages 18 to 49 have significantly greater xerostomia than patients ages 50 to 77. Also, xerostomia has been detected more frequently in psychiatric patients than those without such disorders.20 Importantly, 91% of medications used to treat psychiatric conditions — such as antidepressants, antipsychotics/mood stabilizers, and anti-anxiety/sedative medications — list xerostomia as the primary side effect.21
ATTENTION-DEFICIT DISORDER/ATTENTION-DEFICIT/HYPERACTIVITY DISORDER
Attention-deficit disorder and attention-deficit/hyperactivity disorder are common childhood diagnoses, with the latter being one of the most common neurodevelopmental disorders of childhood. It is usually diagnosed in childhood and persists into adulthood. Treatment often includes behavioral therapy with medication. For children younger than 6, behavioral therapy is the first line of treatment. After age 6, medication may be added.
SCHIZOPHRENIA
Early onset schizophrenia typically presents between ages 13 and 17, and very early onset appears before age 13. The primary treatment is pharmacological, with antipsychotic medications as a first-line choice. All categories of medications used to treat schizophrenia have xerostomia as a side effect.22
ANXIETY AND DEPRESSION
Just over 7% of children ages 3 to 17 are diagnosed with anxiety,23 which presents in these patients as fear or worry they do not readily outgrow. Multiple categories of anxiety-associated disorders exist, including obsessive-compulsive disorder, post-traumatic stress disorder and general anxiety. Most commonly, selective serotonin-reuptake inhibitors or selective norepinephrine-reuptake inhibitors are the drugs of choice. These medications reduce the production of neurotransmitters, which create anxiety in the child.24 The prevalence of major depressive disorders among children is approximately 20% by the time they have completed adolescence. Children with depression may have an increased risk of illness and substance abuse. While tricyclic antidepressants have been successfully prescribed for severe depression or anxiety, these medications present significant, but temporary, side effects early or when dosage is increased.25
SEIZURE DISORDERS
Epilepsy is a common chronic neurologic condition in children, affecting 0.5% to 1% of the population during childhood. The highest rate is in the first year of life (0.144%), with prevalence declining among those ages 1 to 4 (0.061%) and ages 6 to 10 (0.054%). The risk of seizure in infants is greater in boys, but similar for boys and girls by age 10.26 Multiple types of seizures exist, including focal (partial) and generalized, with several subcategories. Anticonvulsant medications are prescribed to control and/or prevent seizures, and side effects may develop after several weeks or months of treatment.27,28
ADDING XEROSTOMIA TO THE PEDIATRIC ORAL HEALTH ASSESSMENT
In light of the foregoing discussion, dental providers should consider including xerostomia assessments as part of their regular examination for caries, periodontal conditions, head and neck tumors, and other oral health concerns. These efforts should include providing specific guidance for pediatric and adolescent patients and their parents/caregivers. This is key because parents/caregivers and children are often unaware of the reasons for xerostomia and the impact of oral dryness on the development of plaque and resulting oral health issues.
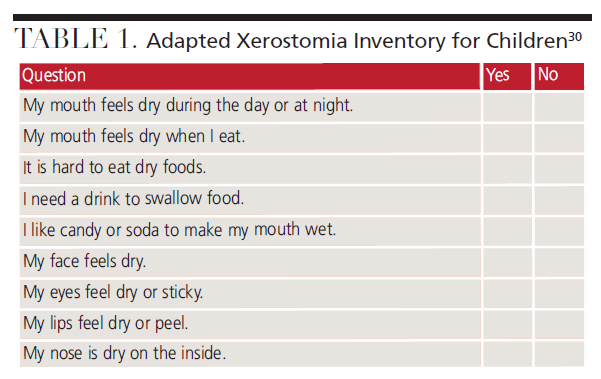
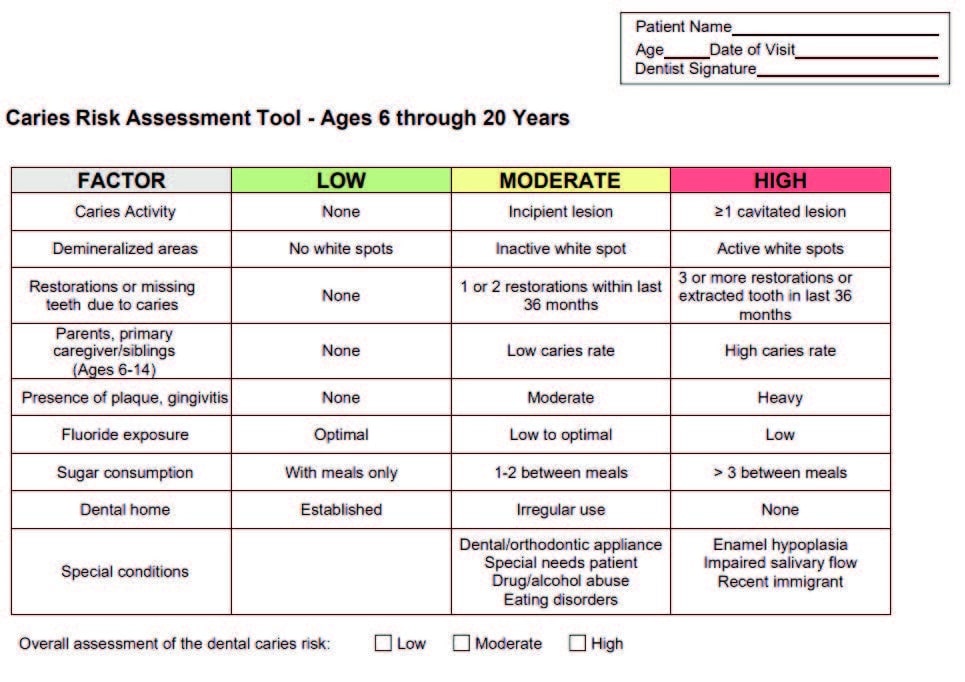
Dental teams often use some form of caries risk assessment with young patients in which plaque, gingival inflammation, demineralization and/or caries are noted. A free form available from Texas Health and Human Services provides a simple caries risk assessment tool for patients ages 6 through 20 (Figure 1).29 By adding a review of the patient’s medical history and current medications to this assessment, along with a few targeted questions taken from the xerostomia inventory (Table 1),30 a more complete evaluation of the pediatric patient is achieved in a short time frame.
The original xerostomia inventory consists of 11 questions with answers based on the frequency of xerostomia. The modified version seen in Table 1 uses simple, age-appropriate language with yes/no answers to make it easy for young patients to complete while still providing information about the presence of xerostomia.
CONCLUSION
Oral health professionals are well-equipped to provide preventive guidance for young patients regarding xerostomia. While this population has not traditionally been thought of as high risk for xerostomia, the increase in medical conditions and medications that result in xerostomia warrant consideration and assessment for this condition. Thus, taking a full medical and medication history is an important first step. Specific attention should be given to reasons that extend beyond poor self-care, including the presence of plaque, inflammation and caries.
Xerostomia in children is often unrecognized due to a lack of understanding by the patient or parent/caregiver. Revising current evaluation tools can raise awareness and help create targeted care plans. Awareness is crucial, and education is key.
References
- Navazesh M, Kumar SK. Xerostomia: prevalence, diagnosis, and management. Compend Contin Educ Dent. 2009;6:326–332.
- Villa A, Connell CL, Abati S. Diagnosis and management of xerostomia and hyposalivation. Ther Clin Risk Manag. 2014;11:45–51.
- Walsh LJ. Dry mouth: a clinical problem for children and young adults. Int Dent SA. 2007;9:48–58.
- Mizutani S, Ekuni D, Tomofuji T, et al. Relationship between xerostomia and gingival condition in young adults. J Periodont Res. 2015;50:74–79.
- Villa A, Polimeni A, Strohmenger L, Cicciù D, Gherlone E, Abati S. Dental patients’ self-reports of xerostomia and associated risk factors. J Am Dent Assoc. 2011;142:811–816.
- Kaur M, Himadi E, Chi DL. Prevalence of xerostomia in an adolescent inpatient psychiatric clinic: a preliminary study. Spec Care Dentist. 2016;36:60–65.
- Cox ER, Halloran DR, Homan SM, Welliver S, Mager DE. Trends in the prevalence of chronic medication use in children: 2002–2005. Pediatrics. 2008;122:1053–1061.
- Urquhart A, Clarke P. U.S. racial/ethnic disparities in childhood asthma emergent health care use: National Health Interview Survey, 2013–2015. J Asthma. 2020;57:510–520.
- Mayo Clinic. Treating Asthma in Children Ages 5 to 11. Available at: https://www.mayoclinic.org/diseases-conditions/childhood-asthma/in-depth/asthma-in-children/art-20044383. Accessed February 3, 2023.
- Godara N, Godara R, Khullar M. Impact of inhalation therapy on oral health. Lung India. 2011;28:272–275.
- U.S. Centers for Disease Control and Prevention. Prevent Type 2 Diabetes in Kids. Available at: https://www.cdc.gov/diabetes/prevent-type-2/type-2-kids.html. Accessed February 3, 2023.
- López-Pintor RM, Casañas E, González-Serrano J, et al. Xerostomia, hyposalivation, and salivary flow in diabetes patients: review article. J Diabetes Res. 2016;2016:4372852.
- Mayo Clinic. Type 2 Diabetes in Children. Available at: https://www.mayoclinic.org/diseases-conditions/type-2-diabetes-in-children/diagnosis-treatment/drc-20355324#:~:text=Medication,insulin%20are%20taken%20by%20injection.Incretin%20mimetics. Accessed February 3, 2023.
- WebMD. Victoza 2-Pak Pen Injector Side Effects by Likelihood and Severity. Available at: https://www.webmd.com/drugs/䁰/drug-163054/victoza-2-pak-subcutaneous/details/list-sideeffects. Accessed February 3, 2023.
- Longhi BS, Appenzeller S, Centeville M, Gusmao RJ, Marini R. Primary Sjögren’s syndrome in children: Is a family approach indicated? Clinics (Sao Paulo). 2011;66:1991–1993.
- Ramos-Casals M, Solans R, Rosas J, et al. Primary Sjögren syndrome in Spain: Clinical and immunological expression in 1010 patients. Medicine (Baltimore). 2008;87:210–219.
- Deasy JO, Moiseenko V, Marks L, Chao SC, Nam J, Eisbruch A. Radiotherapy dose-volume effects on salivary gland function. Int J Radiat Oncol Biol Phys. 2010;76(Suppl 3):S58–S63.
- American Cancer Society. Types of Cancer That Develop in Children. Available at: https://www.cancer.org/cancer/cancer-in-children/types-of-childhood-cancers.html. Accessed February 3, 2023.
- Jenson SB, Mouridsen HT, Reibel J, Brunner N, Nauntofte B. Adjuvant chemotherapy in breast cancer patients induces temporary salivary gland hypofunction. Oral Oncol. 2008;44:162–173.
- Veerabhadrappa SK, Chandrappa PR, Patil S, Roodmal SY, Kumarswamy A, Chappi MK. Evaluation of xerostomia in different psychological disorders: an observational study. J Clin Diagn Res. 2016;10:ZC24–ZC27.
- Winterstein AG, Gerhard T, Shuster J, et al. Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in Medicaid database. Ann Pharmacother. 2008;42:24–31.
- Masi G, Liboni F. Management of schizophrenia in children and adolescents. Drugs. 2011;71:179–208.
- U.S. Centers for Disease Control and Prevention. Anxiety and Depression in Children: Get the Facts. Available at: https://www.cdc.gov/childrensmentalhealth/features/anxiety-depression-children.html#:~:text=Anxiety%20and%20depression%20affect%20many,1.9%20million)%20have%20diagnosed%20depression. Accessed February 3, 2023.
- Wang Z, Whiteside SPH, Sim L, et al. Comparative effectiveness and safety of cognitive behavioral therapy and pharmacotherapy for childhood anxiety disorders: a systematic review and meta-analysis. JAMA Pediatr. 2017;171:1049–1056.
- Dwyer JB, Bloch MH. Antidepressants for pediatric patients. Curr Psychiatr. 2019;18:26–42F.
- Aaberg KM, Gunnes N, Bakken IJ, et al. Incidence and prevalence of childhood epilepsy: a nationwide cohort study. Pediatrics. 2017;139:e20163908.
- Epilepsy Foundation. How Seizure Medicines Work. Available at: https://www.epilepsy.com/treatment/medicines/how-medicines-work. Accessed February 3, 2023.
- University of Iowa Stead Family Children’s Hospital. Pediatric Epilepsy. Available at: https://uihc.org/childrens/services/pediatric-epilepsy. Accessed February 3, 2023.
- Texas Health Steps Caries Risk Assessment Tool — Ages 6–20 years. Available at: https://www.hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/health-services-providers/thsteps/ths-fdh-cra-6-20-years.pdf. Accessed February 3, 2023.
- Thomson WM, van der Putten GJ, de Baat C, et al. Shortening the xerostomia inventory. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:322–327.
From Decisions in Dentistry. March 2023;9(3)40-43.