
COURTESY AMANDA REUTER, DMD
Addressing Ectopic Eruption of Permanent First Molars
Discover effective approaches to manage this common concern
This course was published in the September 2023 issue and expires September 2026. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 180
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define and identify the prevalence of ectopic eruption (EE) of
the first molars. - Discuss the etiology of EE of the first molars.
- List possible treatment strategies for this condition.
Ectopic eruption (EE) is defined as a localized disturbance in the eruption path of a tooth leading to an abnormal position or orientation of that tooth. EE of permanent first molars is observed when the molar assumes an abnormal mesioangular path of eruption, resulting in an impaction at the distal aspect of the primary second molar.1–3
The two types of EE are:1–6
- Reversible ectopic eruption: the 6-year molar tends to “jump” spontaneously or “self-correct” to erupt in its normal position in the dental arch. However, the distal part of the primary second molar may still undergo some amount of resorption.
- Irreversible ectopic eruption: the 6-year molar tends to “hold” or remain impacted preventing eruption into its normal position. It results in premature, atypical resorption of the distal root of the primary second molars.
The possible sequelae of irreversible EE include delayed eruption of the permanent first molar, abscess, premature loss of the primary second molar, loss of space in the dental arch, and subsequent impaction of the second premolar.2,3 Effective management of EE includes timely recognition, diagnosis, providing anticipatory guidance to parents, and early intervention when necessary.

COURTESY AMANDA REUTER, DMD
EE may be suspected when one 6-year molar is particularly behind on eruption compared to its counterparts or when the mesial marginal ridge of a 6-year molar appears to be trapped under the distal aspect of the primary second molar (Figure 1 and 2).3,5
EE of permanent first molars can be diagnosed from bitewing or panoramic radiographs in the early mixed dentition.1,4 Clinicians should begin evaluating the position of the mesial aspect of the permanent first molar in relation to the distal part of the primary second molar on bitewing films at 5 years old.5–8 This provides the opportunity to initiate necessary dialogue with parents early in the process and provide anticipatory guidance. Furthermore, clinicians need to correlate clinical signs with radiographic findings when diagnosing EE.5
COURTESY AMANDA REUTER, DMD
The canting of the occlusal plane of the primary second molar, delayed eruption of one or both 6-year molars of the same arch, and eruption of the distal cusps without the mesial cusps of the same permanent first molar can be considered typical clinical signs of EE. These clinical signs coupled with radiographs provide a definitive diagnosis of EE.3,5
Etiology
The etiology of EE of the first permanent molar could be influenced by various factors. No single etiologic factor has been found to be common to all children experiencing EE. Table 1 lists possible etiologies.1–6
The prevalence of EE of the first permanent molar ranges between 0.75% to 6%.2,4 EE is more common in the maxilla than the mandible.4–6 EE of the maxillary first permanent molar is the most common type with a reported prevalence of 0.75% to 8.7%.2,3,9 Also, the incidence of EE of first permanent molars is slightly higher in boys than girls.4,5
Some research shows that EE of the first permanent molar is often accompanied by other dental anomalies.4 Approximately 60.7% of patients with EE of the first permanent molar exhibit at least one dental anomaly, including cleft lip and palate, supernumerary teeth, congenitally missing teeth, and infra-occlusion.4
Previous research reports that 66% of the first permanent molars experiencing EE tend to self-correct before the age of 7.1,9 However, recent studies demonstrate that 71% of these teeth self-correct by the age of 9.1 Nevertheless, an ectopically erupted first permanent molar that remains locked under the primary second molar at ages 7 to 8 may be irreversible.3,4
Treatment Considerations
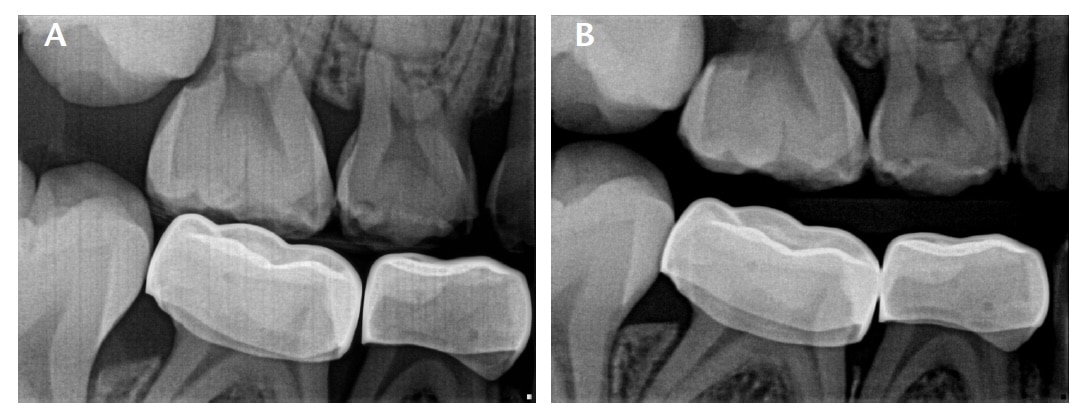
The successful management of EE first permanent molars largely depends on the clinician’s ability to identify the reversible vs irreversible type of EE and the timing of treatment (Figures 3A and 3B). Upon initial diagnosis, a period of observation of 3 to 6 months is recommended to determine whether the EE is reversible or irreversible, especially if the patient is between the ages of 7 and 8.2,3,4,6
When a permanent molar exhibits a slight degree of impaction that is limited to less than the middle of its marginal ridge, it usually tends to self-correct. However, if a significant degree of impaction exists that includes the complete marginal ridge, it usually does not self-correct.5,6
The degree of impaction of the permanent first molar determines the magnitude of resorption that a primary second molar will undergo. Barberia-Leache et al5 described four grades of severity based on the resorption rate of the primary second molar in relation to its distal root:
- Grade I: mild (resorption limited to cementum or with minimal dentin involvement)
- Grade II: moderate (resorption of the dentin without pulp exposure)
- Grade III: severe (resorption of the distal root of primary second molar leading to pulp exposure)
- Grade IV: very severe (resorption affects the mesial root of the primary second molar)
Grades I and II usually self-correct spontaneously before the age of 7 and are considered reversible.3–6 Treatment may not be necessary due to self-correction in grade I but some grade II cases may require minor interventions. However, grades III and IV tend to remain impacted (ie, irreversible) and require interceptive treatment that corrects the eruptive pathway.5,6
Treatment interventions should aim to preserve the primary second molar and avoid early loss of the tooth and the subsequent space loss.5 The presence of severe impaction of the permanent first molar, significant resorption of the primary second molar, and the bilateral occurrence of EE are characteristics that can help identify an irreversible type of EE needing active intervention.1,9
Another challenge is timing the initiation of treatment.4 If EE of the first permanent molar is diagnosed between the ages of 5 and 6, observation until the age of 7 is indicated with the expectation of possible self-correction.10 However, the chances of self-correction decrease once the patient is past the age of 7.2,8,10 Ages 7 and 8 are considered a good time to initiate treatment for severe irreversible cases that do not show any signs of self-correction.4,6,11 Early correction of ectopically erupting permanent molars is an integral part of interceptive orthodontics and is crucial for the proper development of a stable occlusion. A clinician should consider four critical factors before choosing an orthodontic management strategy:2,6,7,8
- Age. If self-correction does not occur between the ages of 7 and 8, 6 months of observation are recommended. Active treatment is necessary if no spontaneous correction occurs during this period.
- Status of the second primary molar. If the tooth experiences irreversible pulpitis or increased abnormal mobility, then extraction is the best option. The clinician should then plan for space management.
- Presence of the second premolar. If the second premolar is congenitally missing, then extraction of the second primary molar is recommended. This will allow the first permanent molar to erupt mesially into the resultant space. The clinician should consider working closely with an orthodontist in this situation.
- Severity of impaction. As the severity of impaction of the first permanent molar increases, the need for early and active treatment intervention increases concurrently.
Once the decision to intervene has been made, the patient and parent/caregiver must be considered while developing the treatment strategies. Most orthodontic corrective procedures employed to remedy EE are economic, fast, and simple. But some may be too complicated, costly, and need substantial chair time along with significant compliance and motivation from patients and parents/caregivers.2,6
Treatment modalities for EE are classified into two types: interproximal wedging and distal tipping. Interproximal wedging is indicated for mild to moderate impactions. Distal tipping with or without second primary molar extraction is indicated in cases of severe impaction. Both types aim to reestablish the correct eruptive path for the impacted permanent first molar.2–4,6–8
Interproximal wedging includes the placement of a separating medium, such as elastic separators, Kesling separators, brass wires, spring-type de-impactors, helical springs, and bonded light wires, between the first permanent molar and the second primary molar.6–8,11 Additionally, the placement of preformed crowns or bands on the primary second molar or performing enameloplasty on its distal surface is recommended in cases of moderate impaction. These procedures provide an inclined plane on the primary second molar that guides the eruption of the ectopic permanent first molar. Interproximal wedging procedures require careful supervision and frequent recare appointments.6–8,11
Distal tipping includes the use of a removable or fixed orthodontic appliance. It aims to de-impact the tooth with active appliance therapy.6–8 Removable modified-Hawley appliances, original and modified Humphrey’s appliances, Halterman’s appliance, Croll’s appliance, uni or bilateral reversed band and loop with a distal spur, K-loops, flexible sectional nickel-titanium wires with open coil spring, cervical headgear traction, and fixed devices with transpalatal arches, distal arms/hooks, or finger springs used with bonded buttons for elastomeric chains may be used to accomplish distal tipping.6,7
In cases when the permanent first molar erupts following the extraction of the second primary molar, the process of distalization and space regaining becomes extremely important. This should be followed by space maintenance until the eruption of the second premolar.7 Uprighting techniques, space regainers, and/or space maintainers may be used depending on the case situation.
Primary teeth are the best space maintainers. Research demonstrates that the primary second molar can be used as a space maintainer even in cases with a high degree of both root and crown resorption.3 Typically, a very low percentage of the affected primary second molars will display pulp or periapical complications.3
In situations when the primary second molar is shed early or extracted, the first permanent molar tends to move mesially and tip, resulting in space deficiency for the second premolar. The goal then is to distalize the first permanent molar, upright it, and regain space for the premolar.11 As discussed previously, several orthodontic appliances can help achieve this goal.
Another treatment option is the use of extraoral appliances to induce distal traction on the permanent first molar. This will help upright the tooth in 9 to 12 months. But the process will create relatively little new space. Hence, modern intraoral fixed appliances might be a better choice, especially to regain space.11
Once space is regained, space management becomes critical. Traditional space maintainers can be used until the eruption of the second premolar. In most cases with lost or extracted primary second molar, a reverse band and loop space maintainer are indicted. It may not always be feasible to use a reverse band and loop but when it is, the band is placed around the first primary molar and the loop is extended distally to meet at the mesial surface of the partially erupted permanent first molar.7
When the permanent first molar has adequately erupted and can be banded, or the first primary molar is mobile and close to exfoliating, the appliance needs to be changed. The clinician can switch to a transpalatal arch for unilateral loss of a maxillary primary second molar, a Nance appliance for bilateral loss of maxillary primary second molars, or a lower lingual holding arch for the mandibular arch.7 The lower permanent incisors must have erupted before placing a lower lingual holding arch.
Early orthodontic interventions to correct severe EE begin around ages 7 to 8.3,11 The second premolar typically erupts between the ages of 10 and 12. As such, the motivation of the patient and parent/caregiver must be considered before attempting early treatment. If the patient or parent/caregiver is unwilling, then comprehensive orthodontic treatment may be a option when the patient comes of age.11
Garrocho-Rangel et al6 suggest that the ideal orthodontic technique or appliance to correct EE of the permanent first molar possess the following:
- Performed in only one visit and require minimal adjustment or activation sessions
- Conservative, simple, quick, and inexpensive to fabricate with minimal laboratory work and no impressions
- Provides adequate anchorage and, if possible, without band placement
- Self-cleaning and does not cause damage to surrounding soft tissues
- Needs minimal patient cooperation
- Safe, preventing possible detaching leading to ingestion or aspiration of unilateral appliances
However, researchers acknowledge that none of the listed treatment modalities meet all of the above requirements.6 Therefore, determining the best orthodontic approach for the management of EE is established by the clinician. He or she should carefully consider the clinical and radiographic findings of the case, level of cooperation required from the patient and parent/caregiver, and benefits vs risks of each treatment strategy.6
The best treatment strategy is one that accounts for individual clinical circumstances and effectively tackles potential sequelae to provide the best possible outcome while placing the patient´s well-being at the forefront.
Conclusion
A variety of treatment options are available for the successful management of EE of the first permanent molar. Success is achieved through early recognition, proper diagnosis, development of individualized treatment strategies, and initiation of treatment at the most appropriate time. Additionally, effective communication with parents/caregivers and considering their motivation will further increase the chances of success. Lastly, a team approach to managing severe cases of EE of the first permanent molar is beneficial. Orthodontists and pediatric dentists may both effectively contribute to the comprehensive care of the patient.
References
- American Academy of Pediatric Dentistry. Management of the developing dentition and occlusion in pediatric dentistry. The Reference Manual of Pediatric Dentistry. Chicago: American Academy of Pediatric Dentistry; 2022:424–441.
- Kupietzky A. Correction of ectopic eruption of permanent molars utilizing the brass wire technique. Pediatr Dent. 2000;22:408-412.
- Mendoza-Mendoza A, Villalon-Rivero G, González-Mallea E, et al. Ectopic eruption of the permanent maxillary first molar: Study in a population of 505 South European children. Edorium Journal of Dentistry. 2014;1(1):1–5.
- Chen X, Huo Y, Peng Y, Zhang Q, Zou J. Ectopic eruption of the first permanent molar: Predictive factors for irreversible outcome. Am J Orthod Dentofacial Orthop. 2021;159:e169–e177.
- Barberia-Leache E, Suarez-Clúa MC, Saavedra-Ontiveros D. Ectopic eruption of the maxillary first permanent molar: characteristics and occurrence in growing children. Angle Orthod. 2005;75:610–615.
- Garrocho-Rangel A, Benavídez-Valadez P, Rosales-Berber MÁ, Pozos-Guillén A. Treatment of ectopic eruption of the maxillary first permanent molar in children and adolescents: A scoping review. Eur J Paediatr Dent. 2022;23:94–100.
- Kupietzky A, Soxman JA. Ectopic Eruption of Maxillary First Permanent Molars. Handbook of Clinical Techniques in Pediatric Dentistry. Hoboken, New Jersey: Wiley; 2021:201-215.
- Hennessy J, Al-Awadhi EA, Dwyer LO, Leith R. Treatment of ectopic first permanent molar teeth. Dent Update. 2012;39:656–661.
- Liu J, Liu Y, Li S, Ying S, Zheng L, Zhao Z. Artificial intelligence-aided detection of ectopic eruption of maxillary first molars based on panoramic radiographs. Journal of Dentistry. 2022;125:104239.
- Aldowsari MK, Alsaidan M, Alaqil M, et al. Ectopic eruption of first permanent molars for pediatric patients attended King Saud University, Riyadh, Saudi Arabia: a radiographic study. Clin Cosmet Investig Dent. 2021;13:325-333.
- Kurol J. Early treatment of tooth-eruption disturbances. Am J Orthod Dentofacial Orthop. 2002;121:588–591.
From Decisions in Dentistry. September 2023; 1(8):32-35.




