Oleksii Liskonih / iStock / Getty Images Plus
Oleksii Liskonih / iStock / Getty Images Plus
Providing Dental Care in India vs the United States During a Global Pandemic
Life is full of uncertainty, and the COVID-19 pandemic has demonstrated the need to be adaptable both personally and professionally. We have definitely felt this as oral health professionals in both India and the United States, as well as in efforts to ensure safety in the workplace. Sahil Mhay, BDS, had intended to travel to the United States to work in a public health-focused research lab at the University of Michigan School of Dentistry (UMSOD) in Ann Arbor under the leadership of Romesh Nalliah, BDS, MHCM. However, the pandemic meant that Mhay, a practicing dentist, could not leave India. Throughout the pandemic, Mhay has continued to practice dentistry in India, while Nalliah has continued to practice dentistry and lead the clinical operations at UMSOD. Brandon K. Perry has held leadership roles with UMSOD and the Michigan Dental Association in our profession’s response to the pandemic. This has provided us with an interesting comparison of providing dental care during a global pandemic between India and the US, specifically Michigan.
COVID-19 in India
India has more than 32 million cases of COVID-19 and close to 400,000 deaths1 while the US has experienced more than 36 million cases and over 600,000 deaths.2 Although India has been broadly criticized for its approach to the second wave of the pandemic, it was much more successful in managing the initial threat posed by the novel coronavirus.
As an aggressive preventive measure to pandemic, the Indian government announced nationwide shelter-in-place orders on the March 24, 2020, for 21 days. At that time, only 500 confirmed cases of COVID-19 were identified in a country of 1.3 billion people. The 21-day lockdown was further extended by some Indian state governments which, in aggregate, totalled up to 90 days of disruption to “normal life” in some states. Although there were huge financial consequences, most agree that the lockdowns slowed the spread of the virus and prevented hospitals from being overwhelmed. Meanwhile, the additional time helped the Indian government to better plan and prioritize its resources to handle such a calamity with a lack of apt infrastructure.
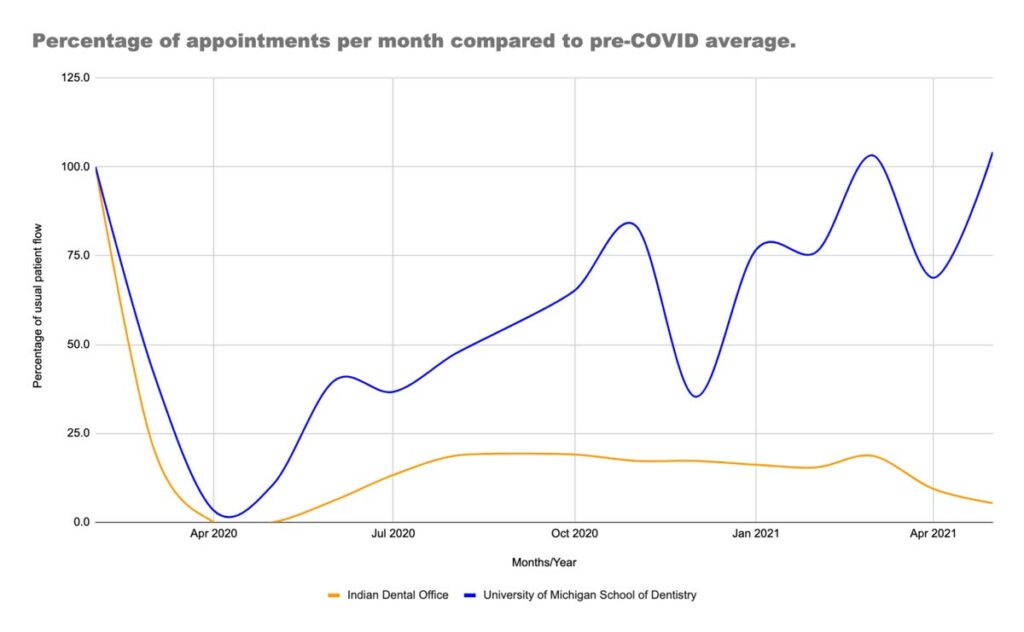
During these extended lockdowns, elective dental procedures were prohibited and practices were limited to emergency services only. The Indian dental profession was one of the worst hit businesses, with up to 3 months of closures in some states. The practice of Mhay serves mostly Indian expatriates who prefer to return to India for their dental treatment due to their advantage in the exchange rate. Since COVID-19, international travel bans and patient hesitance have devastated Mhay’s dental office, which is experiencing huge financial losses. During this time, Mhay continued to deliver emergency care in his practice. Figure 1 demonstrates his monthly patient flow. Patient flow rate has fallen to as low as 5% of normal levels in the recent month and sustained reductions in revenues by about 83%.
Figure 1.
As the Indian lockdowns ended in July and August of 2020, dentists were allowed to deliver routine elective procedures. The devastated economy, however, meant that people had bigger concerns than the state of their oral health and were not ready to return to the dentist. Activity in India has not returned to historic norms and many dental offices are struggling financially. The pandemic has so devastated Indian dentistry that many dentists have left the profession to pursue other sources of income. Mhay has a colleague who was laid off as an associate dentist and gained employment as a medical transcriptionist.
As Indian dental offices reopen, the Indian Dental Association (IDA) issued guidelines for treating dental patients based on guidelines from the World Health Organization, Australian Dental Association, US Centers for Disease Control and Prevention (CDC), American Dental Association (ADA), and US Occupational, Safety and Health Administration. In India, the IDA has facilitated the safe resumption of routine dental care through guidelines and recommendations. The Dental Council of India holds dentists accountable to standards and conducts checks on providers for quality assurance. Finally, legislation that relates to dental care delivery is determined by the Indian Ministry of Health and Welfare.
Table 1. COVID-19 recommendations for Indian vs United States dentists to facilitate safe return to patient care.
|
Protocols required or formally suggested within the Indian dental profession |
Protocols required or formally suggested within the US dental profession |
|
|
COVID-19 changes recommended to facilitate safe return to care |
|
|
Table 1 shows that the CDC and Michigan regulations were much more prescriptive in their orders related to dental practice in the pandemic. It’s important to note that Indian dentists followed almost all of the same protocols but were not required to through their governing bodies.
Evidence has shown that COVID-19 transmission in outdoor settings is extremely limited and, thanks to consistently warm weather, Indian dentists are able to open windows to allow natural ventilation. During colder months in the midwest region of the US, this is not an option. Instead, US dentists have turned to HEPA filtration units and chairside scavenger units to capture aerosols. Some larger practices have made changes to heating, ventilation, and air conditioning (HVAC). Some examples of HVAC changes include increasing the air exchanges per hour or increasing the proportion of outside air brought into the HVAC system to mix with recycled air.
In India, the pandemic will have long lasting impacts on the dental profession and the oral health of the nation. Around 51% of the Indian population have periodontal diseases.3 India also has a high rate of oral cancer, and a lack of preventive and routine dental care could have severe downstream consequences in India. Indian news sources report a 63% decrease in preventive dental care since last year.4
The Pandemic in the United States
In contrast to India, the US has been widely criticized for its piecemeal approach to the initial threat of COVID-19 but has done much better with subsequent waves largely due to rapid vaccine deployment. However, mandated shelter-in-place orders impacted dental offices throughout the US. The blue line in Figure 1 reflects appointment data at the University of Michigan School of Dentistry. We used an average of January and February 2020 to estimate a “normal month” pre-COVID as a reference point (100% appointments) and compared all subsequent months to that average.
UMSOD decided to limit activity to emergency services 1 week before the Michigan state mandate (March 21, 2020).5 As can be observed, UMSOD is now above 100% of pre-COVID capacity, however, this varies by clinic. Each dental school clinic (DSC) has a different mixture of patients, payers, and providers, which leads to different recovery rates. For example, the predoctoral clinics are around 85% of pre-COVID capacity while our private practice, Dental Faculty Associates, is well above 100% like many dental offices in Michigan that have returned to normal pre-COVID patient volumes. Unfortunately, this is in complete contrast to our colleagues in India. In Michigan, the pandemic resulted in dental office closures from March to June 2020, and difficulty accessing adequate personal protective equipment (PPE) caused a slow ramp up in late summer and early fall of 2020. Although Michigan has had several waves of COVID-19, broadly accessible vaccines have facilitated a reduction in cases and a return to somewhat normal activity in dental offices throughout this state.6
The ADA anticipates up to a 66% decrease in dental spending in 2020.7 During US shutdowns, 79% of offices remained open for emergency services only while 18% shutdown altogether.7 The situation in India may be even worse as COVID-19 numbers continue to rise, however, no nationwide data are available to confirm or refute this.
Future Outlook
In contrast to the first wave in India in 2020, the second wave of COVID-19 has been even more devastating in 2021. The fatality rates and contagious nature of the disease have shaken up the healthcare system causing social and economic fallout. In addition to being an already stressful profession, rise in the fear of being exposed and transmitting the infection has left many oral health professionals with psychological burnout, depression, and anxiety. One important point to note is that there is no clear evidence of clinical transmission of COVID-19 in dental practices in India or the US. However, there is evidence that oral health professionals are at higher risk.8 Along with these fears, employment and economic instability further add to oral health professionals’ woes. Also, in India, there is no dental insurance. With the surging cost of care, it is possible that more and more people will face financial challenges in accessing dental services in India. This could lead to the formation of dental insurance companies to spread the risk of high-cost care among many insurance company members.
While dental practices recover in the US with a positive outlook for the remainder of 2021 and ahead, we believe that dentistry in India is about to go through its darkest hours with economic losses for dentists and a growing burden of disease for patients.
References
- Johns Hopkins University Coronavirus Resource Center. India. Click here.
-
Johns Hopkins University Coronavirus Resource Center. COVID-19 Data in Motion. Click here.
-
Janakiram C, Mehta A, Venkitachalam R. Prevalence of periodontal disease among adults in India: A systemic review and meta-analysis. J Oral Biol Craniofac Res. 2020;10:800–806.
-
Awasthi P. Preventive dental treatments fall 63.7% due to COVID-19. The Hindu Business Line. Click here.
-
The Office of Governor Gretchen Whitmer. Executive Order 2020-17: Temporary restrictions on non-essential medical and dental procedures. Click here.
-
Coronavirus tracker. Bridge Michigan Magazine. Click here.
-
Nasseh K, Vujicic M. Modeling the impact of COVID-19 on US dental spending. Click here.
-
Meethil AP, Saraswat S, Chaudhary PP, Dabdoub SM, Kumar PS. Sources of SARS-CoV-2 and other microorganisms in dental aerosols. J Dent Res. 2021;100:817–823.