
Treating Bruxism in Children
Although bruxing is common in pediatric patients, there is no consensus on practice guidelines — thus, clinicians should consider the following when planning treatment.
This course was published in the February 2018 issue and expires February 2021. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
- Discuss bruxism, as well as clinical considerations when treating bruxing in pediatric patients.
- Explain its prevalence, and possible etiologies for bruxing in this population.
- List clinical challenges to diagnosis and treatment of bruxism in children and adolescents.
Derived from the Greek word brychein, bruxism means tooth grinding. The term was introduced in 1931 to describe involuntary, excessive grinding, clenching or rubbing of the teeth during nonfunctional movements of the masticatory system. More recently, it has been further defined as a diurnal (when it happens during the day) or nocturnal (when it happens at night) parafunctional activity. It refers to movements of the jaw that are beyond the normal functional activity of the teeth and jaws (e.g., speaking, chewing or swallowing).
Children are susceptible to habits conducted without consciousness, such as nail and cheek biting or nonnutritive sucking. In children, diurnal bruxing — which manifests as clenching of the teeth — often occurs without any cognitive awareness, especially during stressful situations or intense concentration. When the child is made aware of the activity, the bruxing can be stopped or modified. On the other hand, sleep bruxism, which presents as grinding or clenching of the teeth, cannot be consciously stopped. In 2005, the International Classification of Sleep Disorders reclassified sleep bruxism as a sleep-related movement disorder, rather than its previous classification as a parasomnia, which is an undesirable movement occurring during sleep. This puts it in the same category as restless leg syndrome and sleepwalking.
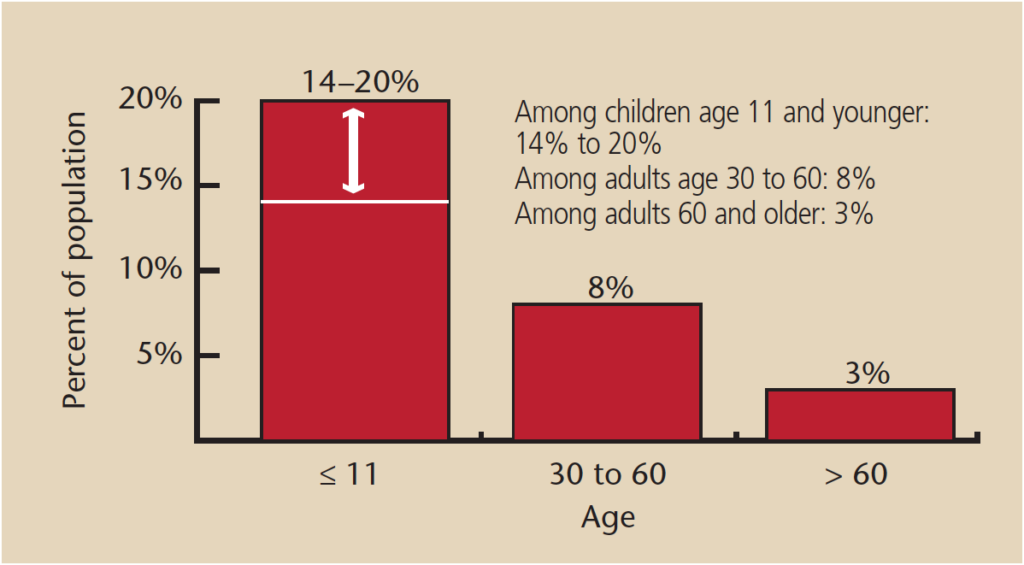
The prevalence of bruxing in children is difficult to determine because estimates are generally based on parental reporting or clinical findings of tooth wear. Its occurrence may be variable over time, so finding tooth wear is not necessarily indicative of current tooth grinding. Its prevalence in children varies greatly: estimates range from 7% to 88%.1 Children younger than 11 are most often affected, with a reported prevalence of 14% to 20%.1 In healthy infants, sleep bruxism typically starts around age 1, soon after the eruption of the primary incisors. Bruxism appears in approximately 13% of 18- to 29-year-olds,1 and then significantly decreases with age (Figure 1).2
Research is not definitive on the role of gender in the prevalence of this behavior. While most studies indicate there is no significant gender effect, others report that girls are more frequently affected.1,3 It does appear to be more common in individuals with developmental disabilities, particularly those with profound intellectual disabilities, autism spectrum disorder or Down syndrome.4
The role of genetics in bruxing is also unclear, although an association appears to exist between child and parental bruxism. Based on self-reports, 20% to 50% of sleep bruxism patients have an immediate family member who experienced tooth grinding in childhood.5 Bruxing shares a common genetic background with sleep talking, a parasomnia.6 Although recent publications favor the role of genetics in the etiology of bruxism, the exact genetic mechanism has yet to be identified. Toward that goal, a study by Abe et al7 identified one allele that has been associated with bruxism.
ETIOLOGY
Although the etiology of bruxism remains controversial, consensus is that it is multifactorial. Current literature suggests that sleep bruxism is regulated centrally (by pathophysiological and psychological factors), and not peripherally (via morphological factors).8 Morphological factors include occlusal discrepancies and anomalies of articulation of the orofacial region. That noted, research shows that eliminating interferences in occlusion and articulation has no influence on bruxism activities.9 Moreover, experimentally placed deflective occlusal contacts do not seem to elicit bruxing.9 Therefore, not every child with bruxism has occlusal interferences, and not all children with such interferences are bruxers.10
In children, it is often difficult to determine whether tooth attrition is due to bruxing because the occlusal surfaces of primary teeth become ground physiologically. One theory about how bruxism starts in children is occlusion instability created during the replacement of the primary teeth by the permanent dentition. However, research has failed to show a significant role of occlusal discrepancies in the genesis of sleep bruxism, and there is no evidence of the role of occlusion and articulation in its etiology.10
BRUXISM AND SLEEP
Pathophysiological factors are believed to play a role in the precipitation of bruxism. In younger children, bruxing may be due to the immaturity of the masticatory neuromuscular system. Current thinking is that bruxism is part of an arousal response; that is, a sudden change in the depth of sleep, during which the individual either arrives at a stage of lighter sleep or wakes up. In young adults, more than 80% of sleep bruxism episodes occur during sleep stages 1 and 2 of non-rapid eye movement (NREM or light sleep stages), and 5% to 10% in REM (deep sleep stages).5 Many bruxing episodes lead to a shift in sleep stage, usually toward lighter sleep or awakening.
Considering there is increased cortical and autonomic cardiac activity preceding bruxing, there appears to be a relationship with the autonomic nervous system. Bruxism is often seen in patients with altered states of consciousness, and is a common complication in children who have sustained traumatic brain injury. Resolution is often associated with improvement in consciousness in patients who were initially comatose, but subsequently returned to sleep-wake cycles. Bruxing appears at several levels of consciousness, but it usually only disappears after a substantial improvement in consciousness occurs.
The dopaminergic system may play a role in sleep bruxism, but this idea remains controversial. The long-term use of medications that exert an indirect influence on the dopaminergic system — such as antidepressant drugs, including selective serotonin reuptake inhibitors — may cause bruxing. The number of children taking these types of drugs is growing, which is an important factor to consider when treating children with bruxism. Hyperactivity is associated with bruxing, and the amphetamines used for managing attention deficit hyperactivity disorder can also cause bruxism.3
RESPIRATORY FACTORS
Bruxism and habitual snoring are closely related. Pediatric sleep bruxism is a frequent complaint of parents of children who are mouth breathers. One theory suggests there is a correlation between bruxing and upper airway obstruction, with obstructive sleep apnea causing sleep bruxism. Bruxing does appear to be more prevalent when sleeping in a supine position, which correlates with a greater possibility of airway obstruction. A link has also been made between bruxing and tonsillar hypertrophy, which is strongly correlated to upper airway obstruction. Adenotonsillectomy surgery has been shown to improve bruxism in some children.11 Bruxing may also be caused by allergic processes, such as asthma or respiratory airway infections.12
PATHOPHYSIOLOGICAL CONSIDERATIONS
Pathophysiological factors implicated in bruxing among adolescents include smoking, alcohol, illicit drugs, trauma, disease and medications. Heavy exposure to secondhand smoke has been shown to have a strong association to sleep bruxism in children. Other risk factors for sleep bruxism include problems during sleeping, along with sleep disturbances, such as noise in the room, sleeping for ≤ 8 hours per night, and sleeping with a light on.13 In addition, a host of diseases among pediatric patients has been linked to bruxing, including basal ganglia infarction, cerebral palsy, Down syndrome, epilepsy, Leigh disease, meningococcal septicemia, multiple system atrophy, gastroesophageal reflux and Rett syndrome.
Bruxing and clenching are common in comatose patients. These behaviors can inflict injuries to the teeth and soft tissues, often requiring an intervention that may include mouth props, prosthetic appliances, or botulinum-A injections delivered intraorally to relieve muscle spasticity. These treatments can be discontinued when consciousness is regained.
PSYCHOLOGICAL INFLUENCES
Stress and personality have been implicated in the etiology of bruxing. Bruxism, either clenching while awake or grinding during sleep, is associated with stress and anxiety. The exact mechanism by which these and other psychological factors contribute to the etiology is still unknown. Emotionally stressful states are often manifested physiologically by an increase in the endogenous release of catecholamines (epinephrine, norepinephrine and dopamine). In comparison to patients who don’t brux, individuals with bruxism have elevated levels of catecholamines in their urine.14 But most data about the association between psychosocial disorders and bruxing come from studies that use clinical or self-reporting to achieve their diagnosis (as opposed to sleep laboratory investigations).
One investigative team15 studied bruxism as it relates to other factors, such as aggression and somatization (the process by which psychological distress is expressed as physical symptoms). The report indicated that an increased amount of aggression and somatization can already be found in bruxing 5- and 6-year-olds. A study by Restrepo et al16 investigated the effectiveness of psychological techniques in children with bruxism. The authors used various psychological techniques, including directed muscle relaxation, for six months in children ages 3 to 6 who had a history of bruxing. They found the psychological techniques used were effective in reducing the signs of bruxism in children with primary teeth. A report by Antonio et al17 described two cases of children who had tooth wear attributed to bruxism. In both cases, the condition was believed to be triggered by psychological disturbances resulting from harrowing experiences. Based on the emotional problems of the children, they were referred for psychological monitoring.
Bruxism is found in those who suffer from post-traumatic stress disorder, further suggesting that a psychological etiology may be involved. A systematic review by Manfredini and Lobbezoo18 concluded that while wake clenching seems to be associated with psychological factors and a number of psychopathological symptoms, they found no evidence to implicate these factors in sleep bruxism.
SYMPTOMS
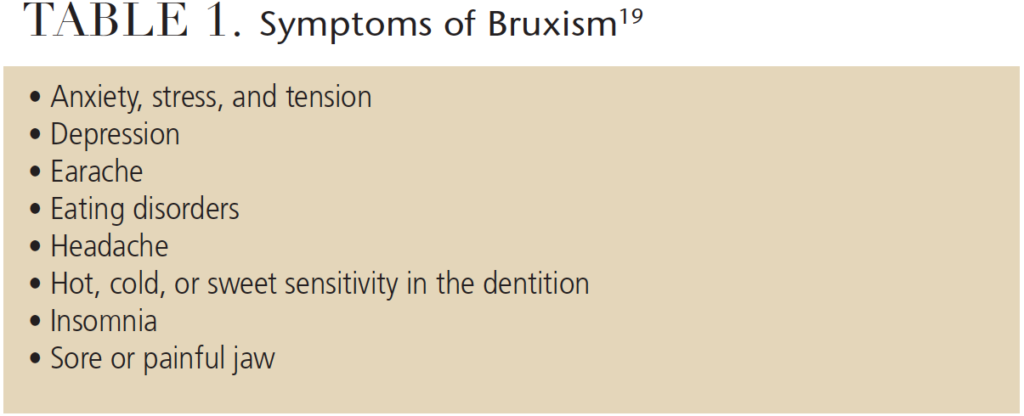
Table 1 lists common symptoms of bruxism.19 Assessment is fraught with methodological problems, however. For example, while questionnaires and interviews, observation of tooth wear, electromyography, and muscle symptoms are used, there are inherent problems with these methods. Questionnaires and interviews rely on recall and may lead to under- or overreporting; in a similar vein, dental wear may be evident, but it may not indicate a current bruxing habit. Thus, there is no consensus on the ideal method for recording this parafunction. It is also difficult to determine if the wear found in children in the primary dentition is from bruxism alone, or the involvement of other variables, such as diet or endogenous factors.
The relationship between temporomandibular disorders (TMD) and bruxism is controversial and unclear.3 Although research has demonstrated an association between bruxing and signs and symptoms of TMD in children and adolescents, other studies have not. Sleep bruxism has been associated with frequent headaches and migraines in children. Because there may be overlap with forms of TMD-type pain and headache and the frequency of sleep bruxing, a correlation between them remains controversial.20 The unreliability of the clinical assessment of bruxism also calls into question conclusions about this relationship. Bruxism in children and adolescents could be associated with muscular disorders, but there is little evidence to link it with disk displacement or other joint pathologies.
CLINICAL TREATMENT
Bruxism in children is so common that it is often considered normal behavior. It is only when a child has severe tooth damage and reports pain, sleep is interrupted, or the noise is sufficient to disturb parents that it may become a pathological condition. Others assert that bruxism cannot be considered normal, even during the beginning of the mixed dentition.21 In addition, the literature does not provide adequate support to treat bruxism in children; this includes use of a rigid occlusal splint for primary dentition — the most common treatment in other patient populations.
Local therapies to consider in bruxing children include avoiding chewing gum, sleeping without a pillow, wet heat, and no television before bedtime.22 Because children generally outgrow the condition, treatment is not recommended. Pediatric patients with upper airway obstructions or severe psychological problems should be referred to specialists. In children or adolescents who are taking medications for conditions that may cause bruxism, other options should be discussed with the patient’s primary care provider.
Treatment of bruxism in children with developmental disabilities may be even more challenging. Given the negative impact and high prevalence of bruxism in developmental disability populations, treatment for this disorder is a priority. According to Lang et al,4 intervention approaches for this population may include prosthodontics, oral surgery, behavior modification, music therapy, massage or the injection of botulinum-A toxin. However, Lang et al4 concluded the evidence base is extremely limited, and no definitive statements regarding treatment efficacy can be made.
CONCLUSION
Although bruxism in children is common, the literature on its diagnosis and treatment is not yet extensive enough for evidence-based clinical practice guidelines. Until the etiology of bruxism is definitively determined, treatment options will remain based on anecdotal evidence. Clearly, well-designed studies on the management of bruxism in children are needed.
REFERENCES
- Cheifetz AT, Osganian SK, Allred EN, Needleman HL. Prevalence of bruxism and associated correlates in children as reported by parents.i. 2005;72:67–73.
- Macedo CR, Silva AB, Machado MA, Saconato H, Prado GF. Occlusal splints for treating sleep bruxism (tooth grinding). Cochrane Database Syst Rev. 2007;4:CD005514.
- Barbosa Tde S, Miyakoda LS, Pocztaruk Rde L, Rocha CP, Gavião MB. Temporomandibular disorders and bruxism in childhood and adolescence: review of the literature. Int J Pediatr Otorhinolaryngol. 2008;72:299–314.
- Lang R, White PJ, Machalicek W, et al. Treatment of bruxism in individuals with developmental disabilities: a systematic review. Res Dev Disabil. 2009;30:809–818.
- Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil.
2008;35:476–494. - Hublin C, Kaprio J, Partinen M, Koskenvu M. Parasomnias: co-occurrence and genetics. Psychiatr Genet. 2001;11:65–70.
- Abe Y, Suganuma T, Ishii M, et al. Association of genetic, psychological and behavioral factors with sleep bruxism in a Japanese population.
J Sleep Res. 2012;21:289–296. - Yap AU, Chua AP. Sleep bruxism: current knowledge and contemporary management. J Conserv Dent.
2016;19:383–389. - Negoro T, Briggs J, Plesh O, Nielsen I, McNeill C, Miller AJ. Bruxing patterns in children compared to intercuspal clenching and chewing as assessed with dental models, electromyography, and incisor jaw tracing: preliminary study. ASDC J Dent Child. 1998;65:449–458.
- Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil. 2001;28: 1085–1091.
- DiFrancesco RC, Junqueira PA, Trezza PM, de Faria ME, Frizzarini R, Zerati FE. Improvement of bruxism after T & A surgery. Int J Pediatr Otorhinolaryngol. 2004;68:441–445.
- Grechi TH, Trawitzki LVV, de Felício CM, Valera FCP, Alnselmo-Lima WT. Bruxism in children with nasal obstruction. Int J Pediatr Otorhinolaryngol. 2008;72:391–396.
- Castroflorio T, Bargellini A, Rossini G, Cugliari G, Rainoldi A, Deregibus A. Risk factors related to sleep bruxism in children: a systematic literature review. Arch Oral Biol. 2015;60:1618–1624.
- Vanderas AP, Menenakou M, Kouimtzis T, Papagiannoulis L. Urinary catecholamine levels and bruxism in children. J Oral Rehabil. 1999;26:103–110.
- Kuch EV, Till MJ, Messer LB. Bruxing and non-bruxing children: A comparison of their personality traits. Pediatr Dent. 1979;1:182–187.
- Restrepo CC, Alvarez E, Jaramillo C, Velez C, Valencia I. Effects of psychological techniques on bruxism in children with primary teeth. J Oral Rehabil. 2001;28:354–360.
- Antonio AG, Pierro VS, Maia LC. Bruxism in children: a warning sign for psychological problems. J Can Dent Assoc. 2006;72:155–160.
- Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23:153–166.
- Medline Plus. Bruxism. Available at: nlm.nih.gov/medlineplus/ency/article/001 413.htm. Accessed January 11, 2018.
- Carra MC, Bruni O, Huynh N. Topical review: sleep bruxism, headaches, and sleep-disordered breathing in children and adolescents. J Orofac Pain. 2012;26:267–276.
- Restrepo C, Gomez S, Manrique R. Treatment of bruxism in children: A systematic review. Quintessence Int. 2009;40:849–855.
- Paesani DA. Bruxism: Theory and Practice. United Kingdom: Quintessence Publishing; 2010.
The author has no commercial conflicts of interest to disclose.
FEATURED IMAGE BY GALITSKAYA/ISTOCK/GETTY IMAGES PLUS
From Decisions in Dentistry. February 2018;4(2):53-56.




