Identifying Carotid Artery Atheromas on Pantomographs
These routine dental radiographs may help clinicians recognize calcified buildups that can signal the need for medical referral.
This course was published in the September 2017 issue and expires September 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Describe atherosclerotic processes involving the carotid artery, and the dental professional’s role in identifying this condition.
- Explain how dental panoramic imaging can be used in the detection of calcified carotid artery atheromas, and its controversial role in diagnosing these lesions.
- In the context of carotid artery atheromas, discuss related consequences and complications of arterial stenosis.
Although there is considerable debate about the significance of calcified carotid artery atheromas, oral health practitioners should be able to recognize them on a panoramic radiograph, understand associated risk factors, educate patients, and offer referrals to a primary care physician for appropriate examination and follow-up.1,2,5,6
Cerebrovascular accident (stroke) is a specific type of cardiovascular disease affecting the arteries leading to, and within, the brain. Stroke can occur when a blood vessel carrying oxygen and nutrients to the brain becomes compromised and circulation is impeded. Strokes are defined as either an ischemic attack, in which a vessel becomes blocked, or as an intracerebral hemorrhage, where a blood vessel in the brain bursts and blood leaks into the brain. Deprived of necessary oxygen, brain tissue necrosis can take place.7 Each year, approximately 795,000 Americans experience a new or recurrent stroke, making it the fifth leading cause of death in the United States. Among these individuals, African-Americans are more affected than any other racial group. Of all strokes, 87% stem from ischemic causes, while 10% are due to intracerebral hemorrhage. More women than men suffer strokes each year, in part due to a propensity for greater longevity.8
RISK FACTORS
Accelerated atherosclerosis may exacerbate the prevalence of stroke and other conditions, including coronary artery disease, heart failure and peripheral arterial disease.9 Obesity, high blood pressure, alcoholism, diabetes mellitus, chronic renal disease and menopause are high-risk conditions associated with atherosclerosis. Sedentary lifestyle, stress, radiotherapy of the head and neck, obstructive sleep apnea, advanced age, and male gender are also related, albeit to a lesser degree.10
Diabetes is a powerful and independent risk factor for coronary artery disease, stroke and peripheral artery disease. In addition, major complications include accelerated atherosclerosis and microvascular disease.11–13 Diabetes is often diagnosed among those older than 40 with metabolic and vascular manifestations. Patients with poorly controlled diabetes tend to develop an advanced form of vascular disorder affecting both small blood vessels (microvascular disease) and large blood vessels (macrovascular disease).14,15 Macrovascular disease characterized by atherosclerotic changes is the major cause of morbidity and mortality in individuals with type 2 diabetes.14,15 Effects include angina and myocardial infarction, gangrene in the lower extremities, and carotid artery-associated stroke. Atherosclerosis of the cervical portion of the carotid artery in individuals with type 2 diabetes is caused by associated hyperglycemia, hyperlipidemia and hypertension.14,15
Obesity may increase the level of triglycerides and low density lipoproteins (LDL) in the blood, while high density lipoproteins (HDL) levels may be reduced. The resulting accumulation of fatty substances on vascular walls increases susceptibility to atherosclerosis.1 Increased arterial pressure has deleterious effects on the endothelium. Hypertension-induced atherosclerosis is related to an increase in LDL in the intimae (endothelial wall). These LDLs promote or exacerbate endothelial dysfunction.16 Associated inflammation of the vascular endothelial lining plays a major role in the development of atherosclerosis and arterial hypertension.17
Smoking is a major risk factor for stroke.18 Chronic smoking is associated with functional and structural vascular changes that contribute to plaque development and rupture observed in stroke.19 Tobacco use may increase the risk of arterial contractions and damage to arterial wall linings. In addition, smokers have been shown to have increased LDL cholesterol (the main source of cholesterol buildup and arterial blockage), and reduced HDL cholesterol (which helps remove cholesterol from the arteries).20
Alcohol consumption may affect cardiovascular health negatively or positively. This cause-effect association differs by stroke subtype — slightly lowering the risk of ischemic stroke, but raising the risk of hemorrhagic stroke.21 Hypertension and coagulation disorders caused by alcohol use, as well as alcohol’s anticoagulant effects, may increase the risk of hemorrhagic stroke.22 Heavy alcohol consumption is associated with a high prevalence of atheromatous plaques. Conversely, slight to moderate intake appears to increase HDL cholesterol, decrease LDL cholesterol, inhibit platelet function, decrease coagulation activity, and increase fibrinolysis activity.23
Atherosclerosis is a common feature of chronic kidney disease. Chronic renal disease promotes hypertension and dyslipidemia and increases the risk of endothelial dysfunction and progressive atherosclerosis.24 Arterial calcification, a complication of end-stage renal disease, is a strong predictor of cardiovascular disease.25,26 A high prevalence of carotid artery calcification evident on dental panoramic radiographs has been reported on end-stage renal disease patients undergoing hemodialysis and renal transplant.26 Higher mortality rates among these patients may be associated with an increased occurrence of occlusive lesions and generalized atherosclerosis.26
As women age, risk factors for atherosclerosis may increase, including poor lipid profile and weight gain. Menopausal decreases in estrogen levels have been linked to endothelial dysfunction and susceptibility to associated adverse vascular changes.1 Studies have reported the risk of stroke resulting from atherosclerosis of the carotid artery increases in postmenopausal women.27,28 Reduced estrogen levels are associated with an increase in hepatic lipase activity and a decrease in LDL catabolism. Atherogenic risk factors observed in postmenopausal women include an increase in total cholesterol, reduced HDL levels, an increase in thrombic tendency, and the occasional development of insulin resistance.28,29
Although associated with aging, atherosclerosis may be seen in younger individuals with elevated cholesterol.30 Factors that can harm the vascular endothelium include abnormal metabolic, hypertensive or nutritional events, and viral and/or bacterial infection. Pathology occurs when the inflammatory environment promotes an accumulation of LDL cholesterol and superimposition of calcium deposits in the intimate layer of the endothelium. Platelets, T lymphocytes, macrophages, smooth muscle cells, adhesion molecules and genetic components subsequently interact, forming atheromatous plaque.1,31
RECOGNITION AND REFERRAL
As previously noted, calcified plaques formed at the bifurcation of the internal and external carotids are often visible in panoramic radiographs. A calcified atheroma may appear as an irregularly shaped radiopaque mass or as a radiopaque vertical line located approximately 2.5 cm posterior to inferior, and posterior to the angle of the mandible, adjacent to the space between vertebrae C3 and C4 (Figure 1). This anatomical region is frequently viewable in a properly positioned panoramic image.32 Although pantomographs should not be taken as the primary screening tool for this condition, considering the number that are exposed each year to facilitate diagnosis of dental conditions, secondary findings of calcification should not be ignored.5
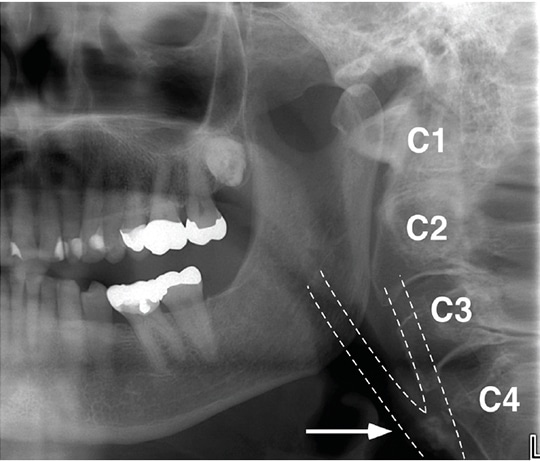
approximately 2.5 cm posterior to the angle of the mandible, adjacent to the space
between vertebrae C3 and C4.
The significance of panoramic imaging in the diagnosis of calcified carotid artery atheromas as a risk for stroke has been discussed at length and remains controversial. While panoramic radiography may have a function in identifying an atheroma, it is not useful in determining the exact location and degree of occlusion.2 Referral to a physician for further diagnostics is necessary to determine calcification and stenosis of extracranial carotid vasculature, and associated risk in patients with atherosclerotic disease.3
The literature does not draw a consistent correlation between calcified carotid atheromas and stoke. Mupparapu and Kim6 performed a critical review of the literature to evaluate evidence linking calcified carotid artery atheroma seen in pantomographs to increased precipitation of stroke. Their findings indicate that “panoramic radiography may demonstrate that carotid artery atheromas calcify over time, but there is little evidence-based information that [such atheromas] are risk predictors for the diagnosis of cerebrovascular disease.” Thus, the utility of using this imaging modality to detect calcified carotid atheromas is limited due to the high potential for a false positive.6 More case-controlled or cohort studies are needed to prove the association between calcified carotid atheroma and stoke, as well as the significance of panoramic radiography as a diagnostic tool.6
Some authors suggest that clinicians should not estimate the risk of stroke with incidental finding of atheroma in the carotid artery alone, but, rather, consider a more comprehensive set of factors, such as age, smoking, cholesterol and hypertension.6 Considering that oral health professionals review their patients’ health histories on a regular basis, this provides an opportunity to recognize and offer counseling on the oral-systemic risk factors previously noted. By understanding and assessing these risk factors — in addition to observing a possible association between radiographic findings and atherosclerotic disease — clinicians may be better able to identify patients at high risk of stroke and refer them to a physician.
CASE REPORT
A 78-year-old woman who was receiving regular dental care expressed concern about the appearance of her severely crowded anterior dentition and the challenges it created during oral self-care. No other dental concerns were reported. The patient’s health history indicated elevated weight, as well as hypertension and high cholesterol, which were controlled by diet and medication. The family history revealed a maternal death due to cerebrovascular accident. A panoramic radiograph taken in anticipation of orthodontic consultation revealed bilateral radiopaque nodules in the area of the carotid bifurcation (Figure 2).

area of the carotid bifurcation in a 78-year-old female patient.
Given the patient’s health history and risk factors, the general dentist consulted with a maxillofacial radiologist. The resulting radiographic interpretation confirmed bilateral appearance of calcification in the carotid area. Further evaluation was recommended, as such calcifications might suggest atheromas in the carotid arteries. Collateral, unrelated radiographic findings indicated external resorption in the coronal aspect of impacted teeth #16 and #32, degenerative joint disease in the cervical spine, and temporomandibular joints that were within normal limits.
After examination, the patient’s primary care physician advised that while carotid bruits (i.e., the sound of blood pulsing through the carotid artery area) were noted while listening with a stethoscope, no other symptoms were present; thus, no further treatment was recommended. Two years later, in consultation preliminary to minor surgery, bruits were again noted by the patient’s general surgeon. A follow-up carotid ultrasound study was recommended. Subsequent results noted moderate plaque bilaterally in the internal carotid arteries, with 50% to 70% stenosis. The patient continued to be asymptomatic. Noting the combined risk factors, family history and ultrasound findings, the surgeon recommended a six-month follow-up. The patient was advised that if blockage increased and/or symptoms developed, a stent might be recommended.
CONCLUSION
Among the core competencies for dental professionals are health promotion and disease prevention.33,34 Dentists and dental hygienists are trained to recognize high-risk groups and individual risk factors through medical histories and oral and systemic findings. As members of the extended health care team, they play an important role in developing strategies to help patients achieve and maintain optimum oral and systemic health.
Recognition of panoramic findings and systemic risk factors related to carotid artery calcification is an important component of effective care. Any findings should be explored with patients to determine the need for referral to a physician for definitive diagnosis, treatment and follow-up, as needed. As with all developing research, oral health professionals should follow ongoing literature in this area in order to make appropriate and evidence-based interprofessional referrals.
REFERENCES
- Guimarães Henriques JC, Kreich EM, Helena Baldani M, Luciano M, Cezar de Melo Castilho J, Cesar de Moraes L. Panoramic radiography in the diagnosis of carotid artery atheromas and the associated risk factors. Open Dent J. 2011;5:79–83.
- Friedlander AH, El Saden SM, Hazboun RC, Chang TI, Wong WK, Garrett NR. Detection of carotid artery calcification on the panoramic images of post-menopausal females is significantly associated with severe abdominal aortic calcification: a risk indicator of future adverse vascular events. Dentomaxillofac Radiol. May 6, 2015. Epub ahead of print.
- Bayer S, Helfgen EH, Bös C, Kraus D, Enkling N, Mues S. Prevalence of findings compatible with carotid artery calcifications on dental panoramic radiographs. Clin Oral Invest. 2011;15:563–569.
- Friedlander AH, Garrett NR, Chin EE, Baker JD. Ultrasonic confirmation of carotid artery atheromas diagnosed via panoramic radiography. J Am Dent Assoc. 2005;136:635–640.
- American Dental Association Council on Scientific Affairs. The use of dental radiographs: update and recommendations. J Am Dent Assoc. 2006;137:1304–1312.
- Mupparapu M, Kim IH. Calcified carotid artery atheroma and stroke: a systematic review. J Am Dent Assoc. 2007;138:483–492.
- American Heart Association/American Stroke Association. About Stroke. Available at: strokeassociation.org/STROKEORG/About Stroke/AboutStroke_UCM_308529_SubHomePage.jsp. Accessed August 3, 2017.
- American Heart Association/American Stroke Association. Impact of Stroke (Stroke Statistics). Available at: strokeassociation.org/ STROKEORG/AboutStroke/Impact-of-Stroke-Stroke-statistics_UCM_310728_Article.jsp#.WX3_isaZOWY. Accessed August 3, 2017.
- Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease: effects on the cardiovascular system. Circulation. 2007;116:85–97.
- Friedlander AH, Cohen SN. Panoramic radiographic atheromas portend adverse vascular events. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:830–835.
- Schwartz CJ, Valente AJ, Sprague EA, Kelley JL, Cayatte AJ, Rozek MM. Pathogenesis of the atherosclerotic lesion. Implications for diabetes mellitus. Diabetes Care. 1992;15:1156–1167.
- Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16:434–444.
- Basta G, Schmidt AM, De Caterina R. Advanced glycation end products and vascular inflammation: implications for accelerated atherosclerosis in diabetes. Cardiovasc Res. 2004;63:582–592.
- Friedlander AH, Maeder LA. The prevalence of calcified carotid artery atheromas on the panoramic radiographs of patients with type 2 diabetes mellitus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:420–424.
- Andersson DK, Svärdsudd K. Long-term glycemic control relates to mortality in type II diabetes. Diabetes Care. 1995;18:1534–1543.
- Dilic M, Dzubur A, Kusljugic Z, Balic S, Pepic E. Correlation of arterial hypertension and type 2 diabetes mellitus with type of polyvascular atherosclerotic disease. Med Arh. 2010;64:264–268.
- Trepels T, Zeiher AM, Fichtlscherer S. The endothelium and inflammation. Endothelium. 2006;13:423–429.
- Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917–932.
- Kumagai M, Yamagishi T, Fukui N, Chiba M. Long-term cigarette smoking increases the prevalence of carotid artery calcification seen on panoramic dental radiographs in male patients. Tohoku J Exp Med. 2007;212:21–25.
- Forey BA, Fry JS, Lee PN, Thornton AJ, Coombs KJ. The effect of quitting smoking on HDL-cholesterol — a review based on within-subject changes. Biomark Res. 2013;1:26.
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671.
- Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J. Alcohol consumption and risk of stroke: a meta-analysis. JAMA. 2003;289:579–588.
- Wakabayashi I. Associations between alcohol drinking and multiple risk factors for atherosclerosis in smokers and nonsmokers. Angiology. 2010;61:495–503.
- Olechnowicz-Tietz S, Gluba A, Paradowska A, Banach M, Rysz J. The risk of atherosclerosis in patients with chronic kidney disease. Int Urol Nephrol. 2013;45:1605–1612.
- Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension. 2001;38:938–942.
- Kansu O, Ozbek M, Avcu N, Gençtoy G, Kansu H, Turgan C. The prevalence of carotid artery calcification on the panoramic radiographs of patients with renal disease. Dentomaxillofac Radiol. 2005;34:16–19.
- Rothwell PM, Slattery J, Warlow CP. Clinical and angiographic predictors of stroke and death from carotid endarterectomy: systematic review. BMJ. 1997;315:1571–1577.
- Taheri JB, Moshfeghi M. Prevalence of calcified carotid artery on panoramic radiographs in postmenopausal women. J Dent Res Dent Clin Dent Prospects. 2009;3:46–51.
- Kritz-Silverstein D, Barrett-Connor E, Wingard DL. Hysterectomy, oophorectomy, and heart disease risk factors in older women. Am J Public Health. 1997;87:676–680.
- Tuzcu EM, Kapadia SR, Tutar E, et al. High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: evidence from intravascular ultrasound. Circulation. 2001;103:2705–2710.
- Hansson GK. Atherosclerosis — an immune disease: the Anitschkov Lecture 2007. Atherosclerosis. 2009;202:2–10.
- Damaskos S, Griniatsos J, Tsekouras N, et al. Reliability of panoramic radiograph for carotid atheroma detection: a study in patients who fulfill the criteria for carotid endarterectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:736–742.
- ADEA competencies for the new general dentist (As approved by the 2008 ADEA House of Delegates). J Dent Educ. 2011;75:932–935.
- ADEA competencies for entry into the allied dental professions (As approved by the 2011 ADEA House of Delegates). J Dent Educ. 2011;75:941–948.
Featured Image by BRANIMIR76/E+/GETTY IMAGES PLUS
From Decisions in Dentistry. September 2017;3(9):42–45.




