 SHIDLOVSKI/ISTOCK/GETTY IMAGES PLUS
SHIDLOVSKI/ISTOCK/GETTY IMAGES PLUS
Effects of Estrogen in Temporomandibular Disorders
More prevalent among women during their reproductive years, temporomandibular disorders may be affected by hormonal fluctuations.
This course was published in the February 2020 issue and expires February 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define and describe temporomandibular disorders (TMDs).
- Discuss the significance of estrogen and TMD-related pain.
- Explain effective strategies for caring for patients with TMDs.
Affecting the quality of life for more than 10 million Americans, temporomandibular disorders (TMDs) are musculoskeletal conditions associated with pain and dysfunction of the temporomandibular joint (TMJ) and muscles of mastication.1–3 The fact TMDs are more prevalent among women during their reproductive years suggests estrogen may play a role in TMD pathophysiology.1 Studies describe the potential role of hormonal fluctuations as a contributing risk factor for TMD-related pain.1,2 Furthermore, evidence suggests estrogen is a prominent hormone that influences the inflammatory and pain processes.1,2
The pathogenesis of TMDs is not well understood. Known risk factors include occlusal abnormalities, macrotrauma to the TMJ, parafunctions (e.g., clenching and bruxing), and psychological factors (e.g., stress and anxiety).4 Commonly reported TMD-related symptoms include headaches, orofacial pain, toothaches, difficulty chewing, locking of the TMJ, and/or pain associated with talking.4,5 Oral radiographs, arthroscopy and advanced imaging — such as computed tomography scans and magnetic resonance imaging — are used in diagnostic testing for TMDs. The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) is a reliable, algorithm-based classification system for TMDs.6
The presence and extent of TMD-related pain can complicate caring for patients with TMDs.7 This article will describe the significance of TMDs and potential role of estrogen receptors in TMD-related pain, as well as provide recommendations and limitations for caring for patients with TMDs.4
ESTROGEN’S MECHANISMS OF ACTION
Estrogen can produce inflammation through various mechanisms of action, including stimulation of toll-like receptors (TLR) in the immune system, upregulation of voltage-gated sodium channels, expression of estrogen receptors, or due to genetic variations called polymorphism.1,8–10 Figure 1 illustrates estrogen’s influence on the systemic inflammatory process.
Stimulation of TLR promotes inflammation by signaling leukocytes (monocytes and macrophages) and glial cells (immune cells in the central nervous system) to release pro-inflammatory messenger molecules known as cytokines.1,8,11 In 2009, Deshmane et al12 described how specialized cytokines, called chemokines, direct the migration of monocytes and macrophages to inflamed sites. They also suggested monocyte chemoattractive protein-1 is the primary chemokine that contributes to the initiation and progression of inflammation in the TMJ.
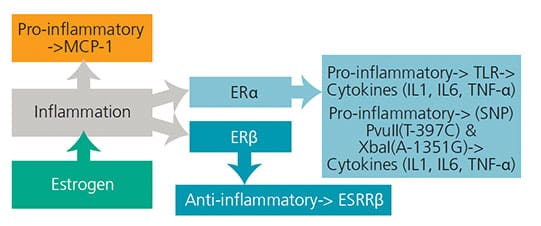
COURTESY TRAN M. LUU, RDH, BSDH
The involvement of TLR in the central nervous system suggests the presence of inflammation, demonstrating the potential for increased chronic pain.11 Estrogen receptors are present in the dorsal root ganglion and trigeminal nerve nucleus,13 and estrogen level fluctuations in these areas may alter the function of the opioid systems, thereby increasing pain perception.8
In 2017, Bi et al10 investigated the correlation between estrogen and upregulation of voltage-gated sodium channels as a source of pain and inflammation in TMDs. In particular, sodium channel 1.7 was theorized to trigger complete loss of pain if disrupted. Researchers found estrogen elevates sodium channel plasma, contributing to increased nociception and hyperalgesia, suggesting that the presence of estrogen may lead to TMD-related pain.10
Estrogen acts by binding two types of steroidal estrogen receptors: estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ). Found in the peripheral nervous system and central nervous system, these receptors are also present in TMJ muscles.8,13 Research shows higher levels of ERα expression could indicate more inflammation, and lower levels of ERβ expression may also lead to increased inflammation.1 Within the synovium of the TMJ, estrogen acts on the central nervous system to regulate the inflammatory process.1,8 Inflammation of the synovium may lead to inadequate lubrication and nourishment of the cartilage and disc.2 ERα has a pro-inflammatory effect on monocytes, as opposed to ERβ, which has anti-inflammatory effects.1 Evidence suggests estrogen is involved in the inflammatory process within the TMJ, particularly in the modification of pain signals.13
Known as single nucleotide polymorphisms, genetic variations on the ERβ increase the risk for TMDs by altering chondrocyte synthesis and releasing interleukin 1 (IL1), interleukin 6 (IL6), and tumor necrosis factor-a.8,9 Therefore, polymorphism offers insight into why estrogen levels affect women differently in terms of TMDs and chronic joint pain. Overall, further research is needed to better understand estrogen’s role in the process of cytokines (particularly IL6) that may exacerbate the inflammation process, and the specific estrogen-induced impact on TMD-related pain.
HORMONAL CONNECTION
Compared to men, Bueno et al14 proposed that women are more predisposed to TMDs, which suggests gender may play a role in the pathophysiology of this condition. Researchers have found estrogen may influence pain receptors, which may highlight the differences between male/female TMD-related pain.14 Fluctuation of estrogen levels occurs before puberty, during menstruation, and after menopause, all of which may impact a woman’s pain threshold.1 Subsequently, pain onset occurs after puberty and peaks in the reproductive years, but tapers after menopause.15 Evidence suggests estrogen inhibits the inflammatory processes associated with TMD-related pain.1 During periods of high estrogen levels, the inflammatory process is inhibited and TMD-related pain decreases.2 In contrast, during the menstrual cycle, post-menopause, and following an ovariectomy, low levels of estrogen occur; consequently, lower levels of estrogen induce pro-inflammatory effects within the TMJ, resulting in higher pain levels.1
A preliminary study by Landi et al16 investigated the relationship between estrogen and TMDs. Results showed that compared to their counterparts, significantly higher serum estrogen levels were found in patients affected by TMDs. Increased serum levels were found in men (p < 0.01) and in the luteal phase of the menstrual cycle in women (p < 0.05). Evidence suggests high serum estrogen levels might play an important role in the physiopathology of TMDs.16
Conversely, other studies report conflicting results, which place into question the extent of correlation between estrogen and TMDs.17,18 For example, in 2005 LeResche et al17 explored the effect of hormonal fluctuations in relation to musculoskeletal pain in the temporomandibular region. Researchers compared pain, depression and somatic symptoms differences between women with musculoskeletal orofacial pain (n = 19) and pain-free women (n = 16) during their pregnancy and 1-year postpartum. The baseline was established at the first trimester with the use of the RDC/TMD algorithm. Study participants completed a self-reported questionnaire and provided a sample of unstimulated saliva at the first, second and third trimester, and 1-year postpartum. The investigators found that both depression and somatic symptoms, excluding pain, changed significantly over time (p ≤ 0.05). Conversely, when assessing women with musculoskeletal orofacial pain and their respective pain-free counterparts, researchers found similar, but statistically insignificant changes (p > 0.05). Nevertheless, women with musculoskeletal orofacial pain demonstrated decreased levels of depression and somatic symptoms 1-year postpartum compared to when they were pregnant (p ≤ 0.05).
In 2018, Ivković et al18 studied the fluctuation of estrogen and its effect on TMDs during normal menstrual cycling, pregnancy and surgically induced menopause. Researchers found that pregnant participants had the lowest pain intensity at the 36th week, while women in surgical menopause experienced significantly higher pain intensity. Even though competing evidence continues to provide an unclear picture of the potential effects of estrogen levels on TMD-related pain, in this study high levels of estrogen appeared to reduce TMD-related pain.
CLINICAL IMPLICATIONS
Treatment modalities for patients experiencing TMD-related pain include self-regulated strategies, anti-inflammatory medications, hormone therapy, botulinum toxin injections, acupuncture and occlusal splint therapy. Surgical interventions can be used to treat peripheral nervous system and central nervous system components of TMD-related pain. Relaxation and biofeedback therapies are commonly used self-regulated strategies for patients with TMD-related pain — however, these therapies are still controversial.
Multiple drugs may also be used for managing TMD pain, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, analgesics, muscle relaxants, anxiolytics, opiates, tricyclic antidepressants, gabapentin and lidocaine patches. When using this approach, clinicians are cautioned to consider the risk of polypharmacy and/or patient dependency. Another consideration is that NSAIDs, often used as a long-term treatment option, only alleviate the symptoms rather than effectively treat TMDs. Topical ointments or creams may be used as an alternative to oral medications that may cause adverse systemic effects.5
Although TMD pain varies throughout the menstrual cycle, it is highest immediately before menses due to low estrogen levels.19 Low levels of estrogen are also present in postmenopausal women, which coincides with an increase in TMD-related pain.1 In 2018, Farzin et al20 found the prevalence and severity of TMD-related pain in menopausal women was higher compared to nonmenopausal women. Specifically, pain in the TMJ and during mandibular movements was more common for menopausal women. Research suggests women with lower estrogen levels benefit from hormone therapy, including the use of continuous oral contraception therapy.19 However, not all patients with TMD-related pain benefit from this therapy, as it is more likely to be effective for women experiencing biological pain rather than mechanical pain (such as clenching and bruxing).19
The use of hormone replacement therapy (HRT) in menopausal women and its relationship on TMD-related care has been studied. In 1997, LeResche et al21 examined the prevalence of TMD-related pain among women who used exogenous forms of hormone replacement. They found that increases in the dosages of estrogen positively correlated with the number of women seeking referral for TMD-related care. These findings suggest that women using a 185-mg annual cumulative estrogen dosage exhibited a 36% increased probability for receiving a referral for TMD-related care. Interestingly, the probability for receiving a referral for TMD-related care escalated to 84% among women using a 220-mg annual cumulative estrogen dosage.
Conversely, some studies suggest the opposite effect.22,23 In 2008, Nekora-Azak et al22 compared the presence of TMD-related signs and symptoms among women who were either using or not using HRT. They found no significant differences between the groups, suggesting there is limited evidence to support an increased prevalence of TMD-related pain in postmenopausal women alone. In 2016, Lora et al23 retrospectively examined the experience of TMD-related pain among postmenopausal women, including those who had or had not used HRT. The team reported no significant difference between the use of HRT and TMD-related pain (p < 0.01).
More recent research, such as Stinson et al,24 supports the idea that future studies should center on the methods of hormone replacement administration. They suggested that differences in results, particularly when it comes to HRT, could be traceable to a change in drug concentration. Research indicates that a rise in estrogen can lead to protective effects, while a decrease in estrogen seems to exacerbate the pain responses.24 Further study is needed on HRT and TMDs in order to better understand this complex relationship.
The use of botulinum toxin-a, a biological exotoxin produced by Clostridium botulinum, has been suggested as a viable treatment for myogenous TMDs.25,26 Research indicates that regardless of type, number of injections or dosage, botulinum toxin-a appears to be effective for TMJ-related muscle disorders.26 In 2019, Sipahi-Calis et al27 studied the efficacy of botulinum toxin injections in treating TMD-related pain. The examination showed that 36% (n = 25) of study participants reported beneficial effects — and no side effects — at the six-month follow-up. Even though these results look encouraging, it also demonstrates this treatment may not be effective for everyone.
Splint therapy and acupuncture are comparable in providing pain relief for this condition. These therapies are more beneficial for myogenous TMDs affecting the muscles, rather than arthogenous TMDs that affect the joints.28 Splint therapy is frequently used with TMDs associated with clenching or bruxing to help correct occlusion and biting forces.5 Acupuncture can also serve as an alternative to managing chronic pain frequently associated with TMDs. The therapeutic effects of acupuncture, such as needle placement and how deep the needle is inserted, can vary among therapists, thus the probability of success may not be the same for all patients.28
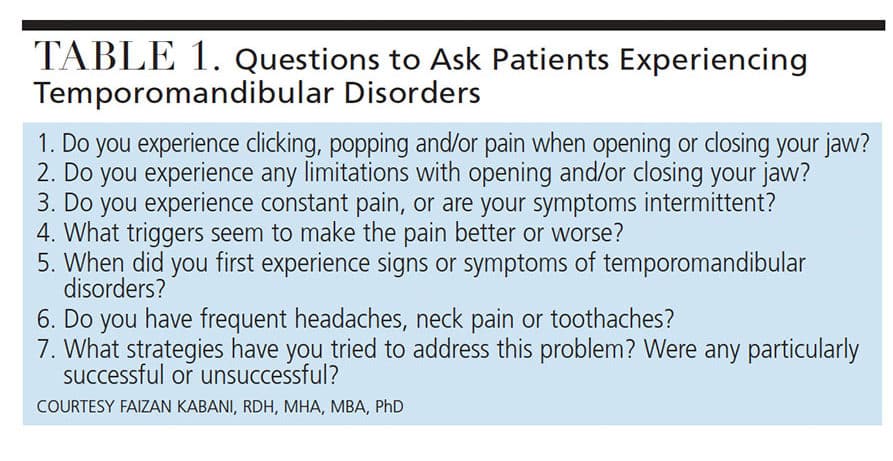
The efficacy of all therapeutic options for patients with TMDs is subjective and should be recommended on a case-by-case basis.28 Advanced surgical interventions — such as arthrocentesis, arthroscopy, modified condylotomy and open-joint surgery — are available, but should only be considered after conservative measures are deemed ineffective. Conservative forms of medical management and rehabilitation are generally recommended over surgical interventions.5 Table 1 lists clinical questions oral health professionals can ask patients regarding the impact of TMDs on quality of life.
CONCLUSION
Despite scientific advances, this is a complex condition1,12,19 with the potential to complicate diagnosis and treatment planning. The evidence indicates hormonal fluctuations may play a significant role in TMD-related pain. Despite mixed evidence on the potential role of estrogen receptors in TMD-related pain, oral health professionals should continue to evaluate patients systemically for other potential contributing factors as part of a comprehensive TMD care strategy.
To date, there is no universally agreed upon gold standard intervention for treating patients with TMD-related pain. While a variety of conservative and surgical treatment modalities exist, clinicians are encouraged to use an evidence-based approach in planning treatment based on the unique needs of each individual patient.5 Current therapies for managing TMD-related pain focus on alleviating symptoms, rather than addressing the root causes of TMDs.5,27,28 Future research is needed on the origins of TMD-related pain and to determine the role estrogen receptors play in targeting inflammation — including how estrogen may be used to alleviate pain associated with TMDs.
Acknowledgement: The authors thank Alfredo Rodriguez, RDH, BSDH, and Amy Heim, RDH, BSDH, for their assistance with this manuscript.
REFERENCES
- Ribeiro-Dasilva MC, Fillingim RB, Wallet SM. Estrogen-induced monocytic response correlates with temporomandibular disorder pain: a case control study. J Dent Res. 2017;96:285–291.
- Furquim BD, Flamengui LM, Conti PC. TMD and chronic pain: a current view. Dental Press J Orthod. 2015;20:127–133.
- National Institute of Dental and Craniofacial Research. TMJ (Temporo-mandibular Joint and Muscle Disorders). Available at: nidcr.nih.gov/health-info/tmj. Accessed December 26, 2019.
- Chisnoiu AM, Picos AM, Popa S, et al. Factors involved in the etiology of temporomandibular disorders — a literature review. Clujul Medical. 2015;88:473–476.
- Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, et al. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res. 2018;11:571–587.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain H. 2014;28:6–27.
- Barros VM, Seraidarian PI, Cortes MI, et al. The impact of orofacial pain on the quality of life of patients with temporomandibular disorder. J Orofac Pain. 2009;23:28–37.
- Ribeiro-Dasilva MC, Peres Line SR, Leme Godoy Dos Santos MC, et al. Estrogen receptor-α polymorphisms and predisposition to TMJ disorder. J Pain. 2009;10:527–533.
- Quinelato V, Bonato LL, Vieira AR, Granjeiro JM, Tesch R, Casado PL. Association between polymorphisms in the genes of estrogen receptors and the presence of temporomandibular disorders and chronic arthralgia. J Oral Maxillofac Surg. 2018;76:314.e1–314.e9.
- Bi RY, Meng Z, Zhang P, et al. Estradiol upregulates voltage-gated sodium channel 1.7 in trigeminal ganglion contributing to hyperalgesia of inflamed TMJ. PLoS One. 2017;12:1–16.
- Nicotra L, Loram L, Watkins L, et al. Toll-like receptors in chronic pain. Expl Neurol. 2012;234:316–329.
- Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res. 2009;29:313–326.
- Berger M, Szalewski L, Bakalczuk M, et al. Association between estrogen levels and temporomandibular disorders: a systematic literature review. Prz Menopauzalny. 2015;14:260–270.
- Bueno CH, Pereira DD, Pattussi MP, et al. Gender differences in temporo-mandibular disorders in adult populational studies: a systematic review and meta‐analysis. J Oral Rehabil. 2018;45:720–722.
- Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs. 2001;169:187–192.
- Landi N, Lombardi I, Manfredini D, et al. Sexual hormone serum levels and temporomandibular disorders. A preliminary study. Gynecol Endocrinol. 2005;20:99–103.
- LeResche L, Sherman JJ, Huggins K, et al. Musculoskeletal orofacial pain and other signs and symptoms of temporo-mandibular disorders during pregnancy: a prospective study. J Orofac Pain. 2005;19:193–201.
- Ivković N, Racic M, Lecic R, et al. Relationship between symptoms of temporomandibular disorders and estrogen levels in women with different menstrual status. J Orofac Pain. 2018;32:151–158.
- Turner JA, Mancl L, Huggins KH, et al. Targeting temporomandibular disorder pain treatment to hormonal fluctuations: a randomized clinical trial. J Pain. 2011;152:2074–2084.
- Farzin M, Taghva M, Bambooie M. Comparison of temporomandibular disorders between menopausal and non-menopausal women. J Korean Assoc Oral Maxillofac Surg. 2018;44:232–236.
- LeResche L, Saunders K, Von-Korff MR, et al. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain. 1997;69:153–160.
- Nekora-Azak A, Evlioglu G, Ceyhan A, et al. Estrogen replacement therapy among postmenopausal women and its effects on signs and symptoms of temporomandibular disorders. Cranio. 2014;26:211–215.
- Lora VR, Canales-Gde L, Goncalves LM, et al. Prevalence of temporomandibular disorders in postmenopausal women and relationship with pain and HRT. Braz Oral Res. 2016;30:100.
- Stinson C, Beliinger LL, Puri J, et al. Estrogenic effects on temporomandibular disorder and pain. J Appl Biobehav Res. 2019;24:12164.
- Bogucki ZA, Kownacka M. Clinical aspects of the use of botulinum toxin type a in the treatment of dysfunction of the masticatory system. Adv Clin Exp Med. 2016;25:569–573.
- Ataran R, Bahramian A, Jamali Z, et al. The role of botulinum toxin a in treatment of temporomandibular joint disorders: a review. J Dent (Shiraz). 2017;18:157–164.
- Sipahi-Calis A, Colakoglu Z, Gunbay S. The use of botulinum toxin-a in the treatment of muscular temporomandibular joint disorders. J Stomatol Oral Maxillofac Surg. 2019;120:322–325.
- Wu JY, Zhang C, Xu YP, et al. Acupuncture therapy in the management of the clinical outcomes for temporomandibular disorders: a prisma-compliant meta-analysis. Medicine (Baltimore). 2017;96:e6064.
From Decisions in Dentistry. February 2020;6(2):32—35.





This is a very thorough and well-structured article.