PETR SMAGIN/ISTOCK/GETTY IMAGES PLUS
PETR SMAGIN/ISTOCK/GETTY IMAGES PLUS
Dermal Fillers in the Dental Setting
While utilization of these cosmetic enhancements has become more prevalent in dental care, their use is not without risk.
This course was published in the January 2022 issue and expires January 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the types of dermal fillers available and their indications for use.
- List the most common complications following injection of dermal fillers.
- Discuss the prevention and management of the most common complications of dermal filler use.
Injectable dermal fillers are widely used in nonsurgical cosmetic dermatology and plastic surgery. A report by the American Society of Plastic Surgeons projects an annual increase of 3% in sales of these soft tissue fillers.1 Among cosmetic procedures, dermal fillers rank second in popularity behind botulinum-toxin injections.2 Along with a continued upward trend in dermal filler use, the type of provider who can administer such injections has also broadened, and currently includes dental professionals. Like any medical procedure, however, there are inherent risks.
Dermal fillers are injected into the mid and deep dermal layers to correct moderate to severe wrinkles and folds, such as the nasolabial folds, marionette grooves and deep scars.3 Current fillers can rebalance facial proportions, increase symmetry, and reduce wrinkles and volume loss.4 In dentistry, dermal fillers are used to improve perioral soft tissues as an alternative to esthetic crown lengthening, especially to correct “gummy smile.” Creating an esthetic smile line with fuller lips can help mask excess gingival display. Reconstruction of the lip volume contributes to proper phonetics and retention of removable prostheses.5 Additionally, fillers are implemented to reduce the unesthetic black triangles formed between anterior teeth following gingival recession and to enhance the interdental papillae noninvasively.6,7 A few clinical reports have shown promising esthetic results using fillers for reconstruction of interproximal papilla.8–12 They have also been used to manage angular cheilitis by filling the perioral tissues.13
CLASSIFICATION OF DERMAL FILLERS
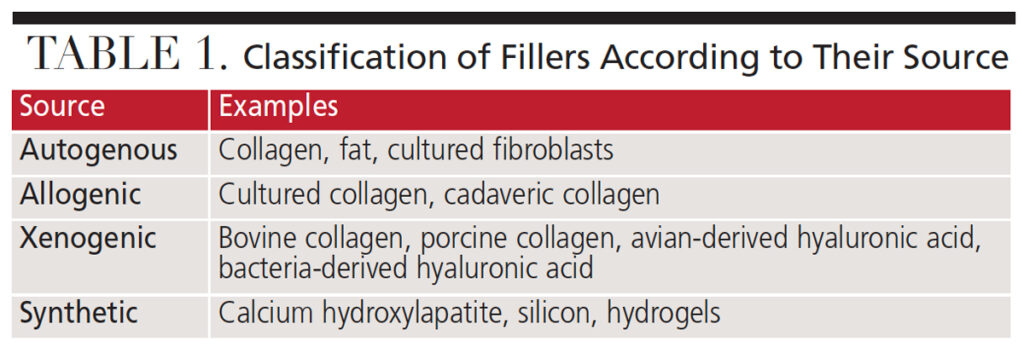
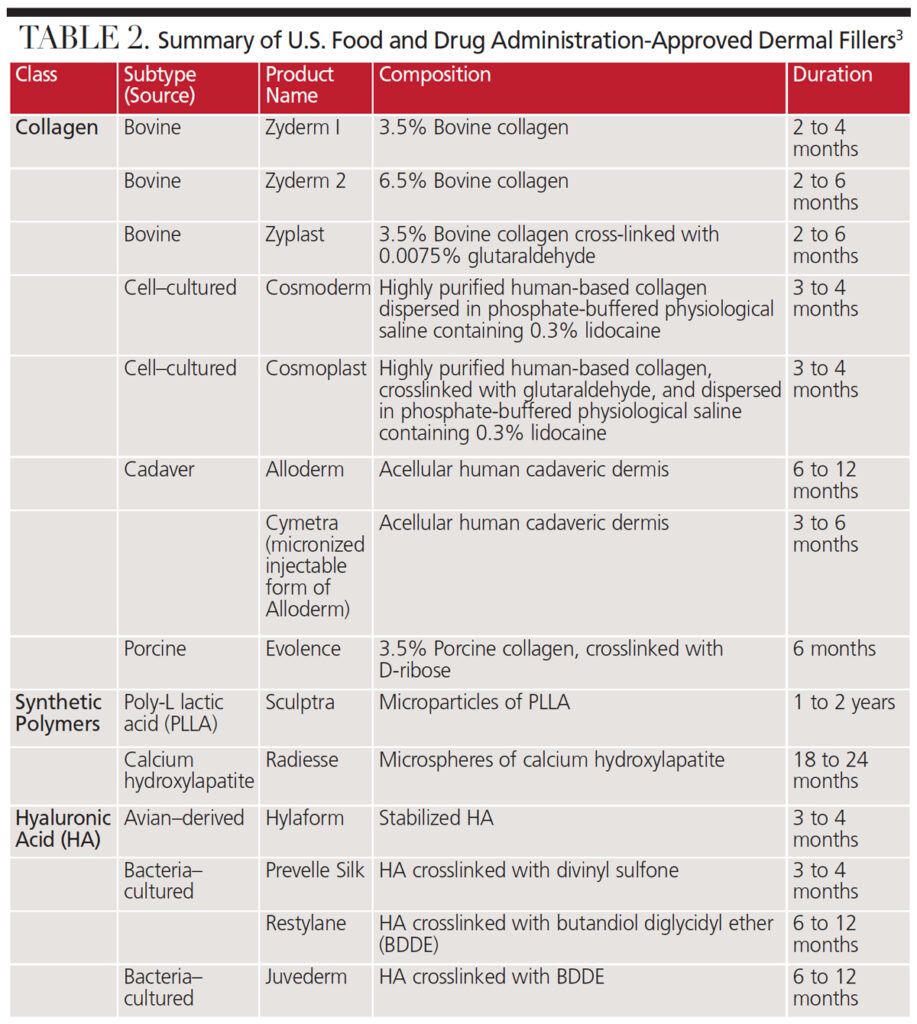
The ideal dermal filler should be safe and simple to use, cost effective, nonmigratory to adjacent structures, and yield predictable and lasting results.14 Currently, no dermal filler meets all these criteria. These products are divided into four major categories based on their source of origin (Table 1). Table 2 lists the U.S. Food and Drug Administration (FDA)-approved dermal fillers in three categories.3
Autogenous Fat — Adipose tissue has been used as an injectable autogenous graft in corrective and plastic surgery since the late 1800s, typically harvested from the abdomen or buttocks.15 Autogenous fat grafts require two surgical sites: donor and recipient. The procured fatty material is also viscous, requiring a large bore needle for its proper delivery, resulting in bruising, swelling and tenderness at the recipient sites.16 Fatty filler’s most significant disadvantage is its low 30% survival rate at one-year post-procedure.17 Most of it is resorbed into the body after that time. It is also associated with an increased risk for vascular complications.18 Due to these shortcomings, autogenous fat is rarely used as a filler in the facial region.
Collagen — A group of proteins found exclusively in the skin and connective tissues of animals, collagen is the major structural component of the skin and oral mucosa. Bovine collagen was the first generation of tissue fillers approved by the FDA. Collagen-based filler products are generally a mixture of type I and type III collagen, and are suspended in a phosphate-buffered physiologic saline solution containing 0.3% lidocaine, which provides anesthesia during injection. However, approximately 3% to 5% of patients may experience a delayed-type hypersensitivity reaction following bovine collagen injection.19 To minimize this risk, two skin sensitivity tests are performed two weeks apart, with the last one done at least four weeks preoperatively. Other forms of collagen fillers are human bioengineered or porcine collagen. Human collagens are either derived from cadaver skin or from tissue culture of human fibroblasts. These products significantly reduce the risk of allergy compared with bovine collagen. Despite these improvements, collagen fillers have been replaced by newer product types.
Biosynthetic Polymers — The second generation of dermal fillers includes a group of biosynthetic polymers (poly-L-lactic acid [PLLA], calcium hydroxylapatite, and polymethylmethacrylate, combined with a variety of injectable carriers, such as hydrogels, beads and liquids.20 As compared to allogenic collagen, they induce the host fibroblasts to produce native collagen for a long duration postoperatively. The most popular products in this group are calcium hydroxylapatite and PLLA. They do not require allergy testing; however, due to their highly viscous nature, intradermal placement can lead to nodule formation (as high as 20% in the lips) and should be avoided.21 As calcium hydroxylapatite and PLLA are slowly resorbed, any placement mistake may have a lasting negative cosmetic outcome. Additionally, with the many advantages of hyaluronic acid (HA), synthetic fillers are no longer widely used.
Hyaluronic Acid — Encompassing the third generation of dermal fillers, HA is currently used in 78.3% of injectable filler products, with an expected annual increase of 7.5%, according to the American Society of Plastic Surgeons.1 This agent is the main polysaccharide in the extracellular matrix of the human connective tissue naturally found in skin and other tissues. It serves both physical and chemical functions.22 Additionally, since it has an affinity to water, HA volumizes, softens, and hydrates the skin. The effects of HA products last up to six to 12 months, depending on the extent of the crosslinking, concentration of the HA, and particle size of various products.23
ADVERSE REACTIONS AND COMPLICATIONS
As noted, the use of dermal fillers is not without risk. Although the incidence of complications is relatively low and most cases are mild, the increase in the number of cosmetic procedures has resulted in a concurrent growth in complications.24 For clarity, these complications are classified according to their clinical manifestations: mild, moderate or severe; pathologic process (ischemic versus nonischemic); and time of onset (early or late). Early onset complications typically appear hours to several days postoperatively, while delayed onset complications usually develop weeks to years post-injection.
Injection Site Complications — The most common side effects associated with filler injections, injection site complications can manifest as edema, erythema, itching, ecchymosis, pain and the Tyndall effect. Typically mild, these adverse effects usually last less than a week.25 Pain complications can be greatly reduced with the use of a small needle gauge, along with topical anesthetic agents and application of ice prior to and after the injection. After consulting with the patient’s primary care provider, having the patient discontinue aspirin and other nonsteroidal anti-inflammatory drugs, along with dietary supplements containing ginkgo biloba, vitamin E, omega-3, fish oil, ginseng, and St. John’s wort, at least one week prior to the procedure is strongly recommended.26 Additionally, the use of arnica, topical vitamin K, or bromelin may decrease post-injection ecchymosis if used pre- and post-injection.
The Tyndall effect manifests as a small, but deep bruise; however, it does not recede over time and requires removal. The Tyndall effect may be caused by placing the HA filler too superficially, which will produce a bluish discoloration. It can be treated by injecting 15 to 50 IU of hyaluronidase (a mucolytic enzyme that hydrolyzes both natural and crosslinked HA dermal fillers).27 Subsequent massage is essential to mechanically mix the hyaluronidase with the HA to promote hydrolysis.28
Infections — Postoperative infections are relatively rare and are caused by microscopic injury to the dermal barrier during injection.29 The breakage of surface integrity provides a pathway for various pathogenic microorganisms to invade. Practicing a strict aseptic technique during the procedure is essential. The patient should not wear any makeup either before or immediately after the procedure. Additionally, proper skin sterilization with 2% to 4% chlorhexidine or 70% isopropyl alcohol solution prior to the injection is required. Injections into inflamed or infected skin, or through previous layers of filler, should be avoided.30
Hypersensitivity — Both immediate (type I hypersensitivity) and delayed (type IV hypersensitivity) reactions following injection of dermal fillers have been reported in the literature.31 A type I reaction can occur within minutes or hours following the injections, and is caused by rapid formation of immunoglobulin E-mediated immune response to the dermal filler. It may present as an angioedema or anaphylactic reaction occurring after initial or repeated exposure.32 The angioedema will usually subside within a few days following intake of antihistamines and/or oral steroids. The patient should be closely monitored to rule out possible infection.
Delayed hypersensitivity reactions are characterized by induration, erythema and edema, and are mediated by T-lymphocytes rather than antibodies. They typically occur 48 to 72 hours postoperatively, but may be seen as late as several weeks post-injection and can persist for several months.33 Delayed hypersensitivity reactions do not respond to antihistamines. The most effective approach is to remove the offending allergen (filler). If HA was used, treatment with hyaluronidase is advised. For other types of fillers, a steroid regimen has been suggested until the filler is fully resorbed. Cassuto et al34 recommend the use of laser therapy to liquify the filler, or total excision and removal of the offending agent.
Lumps and Nodules — Injecting too much filling material results in postoperative formation of lumps and nodules. Early lumps that form within days or weeks tend to be painless and are most likely the result of suboptimal injection techniques, such as use of excess filler, superficial placement, or poor choice of product for the indication.35 Lumps occurring in the early stage of healing may respond to frequent massage of the area. A superficial single nodule due to excessive placement of filler is usually easy to treat with a simple incision and drainage. However, for multiple nodules where surgical removal may not be feasible, enzymatic degradation with hyaluronidase is recommended.28
Dysesthesias, Paresthesia and Anesthesia — Inadvertent nerve damage is a rare complication of dermal filler injection, and may result from direct nerve injury caused by the needle or filling material. Some cases of nerve injury may be transient and reversible, while others are permanent. The most common site of nerve injury is the infraorbital foramen. Less frequently, a transient Bell’s palsy of the facial nerve or mandibular nerve dysfunction may last for several weeks.36 However, while 71% of patients with Bell’s palsy experience complete resolution, the remaining 29% exhibit lifelong residual hemifacial weakness. High doses of oral steroids, along with protective strategies of the ocular surface, are recommended for addressing the acute phase of Bell’s palsy.37 Other options include surgical decompression of the meatal segment, antiviral therapy, electrotherapy, physical therapy and acupuncture. Thorough knowledge of the facial anatomy and innervation by the treating provider are essential to prevent and minimize the incidence of such complications.
Vascular Occlusion — While extremely rare, vascular occlusion requires prompt intervention.38 It has two clinical manifestations: a localized effect resulting in skin necrosis, and a distant vascular occlusion causing loss of vision and cerebral ischemic events.39 Arterial occlusion due to intra-arterial injection usually presents with an immediate skin blanching, accompanied by pain. If not treated swiftly, the affected skin will develop reticulated erythema, purpura and ulceration, leading to scarring. Venous occlusion has a more delayed presentation, with persistent, dull aching pain, swelling, and a reticulated erythema of the skin.40
The glabella is the most common site of necrosis, as small vessels branching from the supratrochlear and supraorbital arteries provide the blood supply to the glabellar region, thus, collateral circulation is limited.41 Other high-risk areas include the nasolabial fold, infraorbital foramen and zygomaticofacial foramen.38 If signs of tissue necrosis appear, the injection should be stopped, and an immediate injection of hyaluronidase enzyme is crucial to curtail the necrosis and minimize tissue damage.42,43 Its action is greatly enhanced by topical applications of warm compresses (for five to 10 minutes every hour to two hours) and vigorous massage. Vasodilatation should be stimulated and the filler material should be disbursed.43 The patient should be monitored on a daily basis. If the necrosis is progressing, the patient should undergo hyperbaric oxygen therapy; other measures include topical oxygen therapy, low molecular weight heparin, systemic steroids, and sildenafil platelet-rich plasma. If these measures fail, the filler should be removed, followed by intravenous administration of prostaglandin.
Proper wound care is essential to minimize the risk of scarring. Treatment of the resulting scar involves the use of silicone pads and intralesional steroid injection. If a scar remains, it may be treated with light dermabrasion, surgical revision, or injection with filler to restore the contour.38 A distant vascular occlusion can lead to loss of vision or cerebral ischemic events.39 Rare cases of visual impairment and blindness resulting from injection in the glabellar region have been reported.44 They are caused by retrograde flow of intravascular injected material into the ophthalmic artery, obstructing the blood flow of the distal branches that supply the retina and cornea. Patients may present with a sudden blind spot or visual field deficit. In the case of immediate vision loss or ocular pain, the injection should be stopped, and the patient should see an ophthalmologist or an oculoplastic surgeon for urgent retrobulbar injection of hyaluronidase.
SUMMARY
As the use of dermal fillers increases worldwide, the incidence of complications is likely to follow. In the United States, dental providers in several states are now permitted to administer dermal fillers following completion of approved training courses. This number is expected to increase over the next few years. Patients must be fully aware of the risks of dermal filler injection and provide informed consent for this therapy. A thorough knowledge of anatomy, the properties of the available filling materials, and injection techniques is essential to prevent complications. It is also necessary to detect complications early and manage them effectively to mitigate untoward incidents and improve patient outcomes.
References
- American Society of Plastic Surgeons. Plastic Surgery Statistics. Available at: https://www.plasticsurgery.org/news/plastic-surgery-statistics. Accessed November 30, 2021.
- American Society for Aesthetic Plastic Surgery. Cosmetic (Aesthetic) Surgery National Databank Statistics. Available at: https://www.surgery.org/sites/default/files/ASAPS-Stats2018.pdf. Accessed November 30, 2021.
- Bray D, Hopkins C, Roberts DN. A review of dermal fillers in facial plastic surgery. Curr Opin Otolaryngol Head Neck Surg. 2010;18:295–302.
- de Maio M. The minimal approach: an innovation in facial cosmetic procedures. Aesthetic Plast Surg. 2004;28:295–300.
- Sinha A, Hurakadli M, Yadav P. Botox and derma fillers: the twin-face of cosmetic dentistry. Int J Contemp Dent Med Rev. 2015:131214.
- Tanwar J, Hungund SA. Hyaluronic acid: Hope of light to black triangles. J Int Soc Prev Commun Dent. 2016;6:497–500.
- Spano SJ, Ghilzon R, Lam DK, et al. Subperiosteal papilla augmentation with a non-animal-derived hyaluronic acid overlay technique. Clin Adv Periodontics. 2020;10:4–9.
- Mansouri SS, Ghasemi M, Salmani Z, Shams N. Clinical application of hyaluronic acid gel for reconstruction of interdental papilla at the esthetic zone. Journal of Islamic Dental Association of Iran. 2013;25(3):208–213.
- Becker W, Gabitov I, Stepanov M, Kois J, Smidt AE, Becker B. Minimally invasive treatment for papillae deficiencies in the esthetic zone: a pilot study. Clin Implant Dent Relat Res. 2010;12:1–8.
- Abdelraouf SA, Dahab OA, Elbarbary A, El-Din AM, Mostafa B. Assessment of hyaluronic acid gel injection in the reconstruction of interdental papilla: a randomized clinical trial. Open Access Maced J Med Sci. 2019;7:1834–1840.
- Patil S, Dhalkari C, Indurkar M. Hyaluronic acid: ray of hope for esthetically challenging black triangles: a case series. Contemp Clin Dent. 2020;11:280–284.
- Awartani F, Tatakis D. Interdental papilla loss: treatment by hyaluronic acid gel injection: a case series. Clin Oral Investig. 2016;20:1775–1780.
- Lorenzo-Pouso AI, García-García A, Pérez-Sayáns M. Hyaluronic acid dermal fillers in the management of recurrent angular cheilitis: a case report. Gerodontology. 2018;35:151–154.
- Dastoor SF, Misch CE, Wang H-L. Dermal fillers for facial soft tissue augmentation. J Oral Implantol. 2007;33:191–204.
- Billings E Jr, May JW Jr. Historical review and present status of free fat graft autotransplantation in plastic and reconstructive surgery. Plast Reconstr Surg. 1989;83:368–381.
- Bellini E, Grieco MP, Raposio E. The science behind autologous fat grafting. Ann Med Surg (Lond). 2017;24:65–73.
- Report on autologous fat transplantation. ASPRS Ad-Hoc committee on new procedures. Plast Surg Nurs. 1987;7:140–141.
- Sito G, Manzoni V, Sommariva R. Vascular complications after facial filler injection: a literature review and meta-analysis. J Clin Aesthet Dermatol. 2019;12:E65–E72.
- McCoy JP Jr, Schade WJ, Siegle RJ, et al. Characterization of the humoral immune response to bovine collagen implants. Arch Dermatol. 1985;121:990–994.
- Buck DW 2nd, Alam M, Kim JY. Injectable fillers for facial rejuvenation: a review. J Plast Reconstr Aesthet Surg. 2009;62:11–18.
- Sklar JA, White SM. Radiance FN: a new soft tissue filler. Dermatol Surg. 2004;30:764–768.
- Garg HG, Hales CA. Chemistry and Biology of Hyaluronan. Amsterdam: Elsevier; 2004.
- Narins RS, Brandt FS, Lorenc ZP, et al. Twelve-month persistency of a novel ribose-cross-linked collagen dermal filler. Dermatol Surg. 2008;34(Suppl 1):S31–S39.
- De Boulle K, Heydenrych I. Patient factors influencing dermal filler complications: prevention, assessment, and treatment. Clin Cosmet Investig Dermatol. 2015;8:205–214.
- Lafaille P, Benedetto A. Fillers: contraindications, side effects and precautions. J Cutaneous Aesthet Surg. 2010;3:16–19.
- Gilbert E, Hui A, Meehan S, et al. The basic science of dermal fillers: past and present. Part II: adverse effects. J Drugs Dermatol. 2012;11:1069–1077.
- Douse-Dean T, Jacob CI. Fast and easy treatment for reduction of the Tyndall effect secondary to cosmetic use of hyaluronic acid. J Drugs Dermatol. 2008;7:281–283.
- DeLorenzi C. Complications of injectable fillers, part I. Aesthet Surg J. 2013;33:561–575.
- Cohen JL. Understanding, avoiding, and managing dermal filler complications. Dermatol Surg. 2008;34(Suppl 1):S92–S99.
- Bailey SH, Cohen JL, Kenkel JM. Etiology, prevention, and treatment of dermal filler complications. Aesthet Surg J. 2011;31:110–121.
- Bellman B. Immediate and delayed hypersensitivity reactions to restylane. Aesthet Surg J. 2005;25:489–491.
- Alijotas-Reig J, Fernández-Figueras MT, Puig L. Late-onset inflammatory adverse reactions related to soft tissue filler injections. Clin Rev Allergy Immunol. 2013;45:97–108.
- Arron ST, Neuhaus IM. Persistent delayed-type hypersensitivity reaction to injectable non-animal-stabilized hyaluronic acid. J Cosmet Dermatol. 2007;6:167–171.
- Cassuto D, Marangoni O, De Santis G, et al. Advanced laser techniques for filler-induced complications. Dermatol Surg. 2009;35:1689–1695.
- Sclafani AP, Fagien S. Treatment of injectable soft tissue filler complications. Dermatol Surg. 2009;35:1672–1680.
- Fitzgerald R, Bertucci V, Sykes JM, et al. Adverse reactions to injectable fillers. Facial Plast Surg. 2016;32:532–555.
- Glass GE, Tzafetta K. Optimising treatment of Bell’s palsy in primary care: the need for early appropriate referral. Br J Gen Pract. 2014;64:807–809.
- Souza Felix Bravo B, Klotz De Almeida Balassiano L, Roos Mariano Da Rocha C, et al. Delayed-type necrosis after soft-tissue augmentation with hyaluronic acid. J Clin Aesthet Dermatol. 2015;8:42–47.
- DeLorenzi C. Complications of injectable fillers, part 2: vascular complications. Aesthet Surg J. 2014;34:584–600.
- Sclafani AP, Fagien S. Treatment of injectable soft tissue filler complications. Dermatol Surg. 2009;35:1672–1680.
- Hirsch RJ, Cohen JL, Carruthers JD. Successful management of an unusual presentation of impending necrosis following a hyaluronic acid injection embolus and a proposed algorithm for management with hyaluronidase. Dermatol Surg. 2007;33:357–360.
- Beer K, Downie J, Beer J. A treatment protocol for vascular occlusion from particulate soft tissue augmentation. J Clin Aesthet Dermatol. 2012;5:44–47.
- Kassir R, Kolluru A, Kassir M. Extensive necrosis after injection of hyaluronic acid filler: case report and review of the literature. J Cosmet Dermatol. 2011;10:224–231.
- Kim D, Eom J, Kim JY. Temporary blindness after an anterior chamber cosmetic filler injection. Aesth Plast Surg. 2015;39:428–430.
From Decisions in Dentistry. January 2022;8(1):36-39.