Dental Management of Patients With Psoriasis
Customizing treatment, anticipating complications, and providing education about self-care techniques can help this patient cohort achieve and maintain optimal oral health.
This course was published in the April 2023 issue and expires April 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define psoriasis and explain its chief characteristics.
- Identify the oral manifestations of this condition.
- Discuss oral care strategies when managing patients with psoriasis.
Psoriasis is a common, chronic, immune-mediated, systemic inflammatory disease that primarily affects the skin and joints. While the exact etiology of this multisystem disease is unknown, it is likely a combination of genetic, environmental and immunologic factors.1-3 This condition is also associated with a variety of systemic comorbidities, oral manifestations, and an overall greater risk of mortality. Due to the systemic inflammatory nature of psoriasis, a multidisciplinary collaborative approach is necessary to effectively manage outcomes.2,3 Oral health professionals who are well versed in psoriasis will be more effective in making treatment decisions and in optimizing oral care for this patient cohort.
Approximately 125 million people (or 2% to 3% of the world’s population) are affected by psoriasis.4,5 In addition, 3% of Americans older than age 20 are impacted by psoriasis, making it one of the most widespread systemic immune-mediated diseases among adults.6 Men and women are affected equally, and the incidence of psoriasis among older adults is higher.6 While psoriasis alone is not life-threatening, research suggests patients with severe psoriasis are at 50% greater risk of mortality compared to patients with milder psoriasis; this may be attributed to an association with systemic diseases.3,4
This papulosquamous disease has highly variable morphology, distribution, severity, and course that varies by phenotype. Once diagnosed, the disease is characterized by chronic progression, with spontaneous remission in some patients.7 Typically, mild psoriasis affects less than 5% of body surface area (BSA); moderate disease affects approximately 5% to 10% of BSA; and severe disease impacts greater than 10% of BSA, and/or lesions are present on the hands, feet, face, scalp or genitals.2
CLINICAL PHENOTYPES
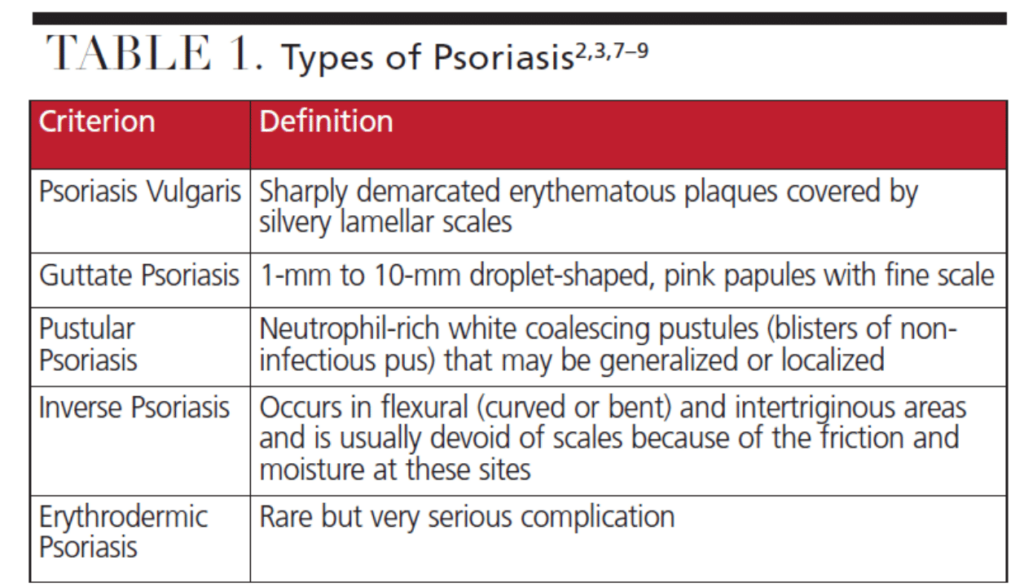
Psoriasis has several clinical phenotypes (Table 1).2–4 Plaque psoriasis, or psoriasis vulgaris, is the most common type and accounts for 90% of cases. It is characterized by well-demarcated, erythematous, symmetric plaques, with an overlying silvery-white scale that may manifest on the scalp, trunk, buttocks, skin folds, nails or palmoplantar regions.2,3,7,8 Inverse psoriasis is site-specific and causes inflamed deep-red smooth skin in flexural and intertriginous areas, such as the underarms, buttocks and genitals, and may not have scales due to friction and moisture at these sites.2
Acute and rare, guttate psoriasis is characterized by 1- to 10-mm droplet-shaped pink papules with a fine scale, and is primarily seen in patients younger than 30. The guttate variety often appears following a ß-hemolytic or group-α streptococcal infection, tonsillitis, pharyngitis or viral infection.2,7,8
Relatively rare, pustular psoriasis is characterized by neutrophil-rich, white coalescing pustules that may be generalized or localized to the palms and soles of the feet, nails, and tips of the fingers and toes, or both. Any form of psoriasis may become erythrodermic, causing intense redness and shedding of the skin in layers — a rare, but potentially life-threatening complication.2,8,9
Psoriatic arthritis is a chronic inflammatory disease defined by peripheral joint inflammation associated with psoriasis. Approximately 10% to 40% of patients with cutaneous psoriasis will develop psoriatic arthritis within five to 10 years of cutaneous onset.7,10 Characterized by joint erosion, joint space narrowing, bony proliferation, pencil-in-cup-deformity, ankylosis, and pain and swelling, psoriatic arthritis may impact physical function and daily activities and can lead to significant morbidity.2,7,8,10,11
INFLAMMATION’S ROLE
Inflammation is essential in the development of psoriasis and may be a shared characteristic underlying the association between psoriasis and comorbidities.8 Compared to the general population, patients with psoriasis may be at increased risk for stroke, adverse cardiovascular events and related mortality.12–14 There may also be a greater prevalence of obesity, hyperlipidemia, hypertension and Type 2 diabetes among individuals with psoriasis compared to the general public.8,15–17 Chronic exposure to smoking and alcohol may also influence the development of psoriasis, affect clinical expression, and increase mortality by interfering with cell-mediated immunity. Research suggests both current and ex-smokers are at an increased risk of psoriasis compared to people who have never smoked; in addition, heavy drinkers tend to have more severe psoriatic disease. The relationship between stress, depression and psoriasis is also complex, as psoriatic lesions may be precipitated or exacerbated by stress, and lesions may negatively affect quality of life, leading to significant psychological problems. Self-esteem and body image can be negatively affected by psoriasis.18,19
As noted, while the etiology of psoriasis is largely unknown, it has a strong genetic predisposition and is thought to be a T-cell-mediated immune dermatosis in which T-cells and dendritic cells are inappropriately activated, causing the release of inflammatory cytokines.20 Infectious pathogens that may provoke or exacerbate psoriasis include Streptococcus pyogenes, Staphylococcus aureus, Malassezia, Candida albicans, papillomaviruses, retroviruses, and endogenous retroviruses. Certain drugs — including lithium, beta blockers, nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme inhibitors, and antimalarial agents — may also be associated with the initiation or aggravation of psoriatic disease.2,21
While there is no cure for psoriasis, patient-centered treatment options are available. Psoriasis is a chronically relapsing disease that often requires long-term therapy. Treatment should consider severity, presence of psoriatic arthritis and other medical conditions, patient preference, clinical needs, benefits, risks, and cost effectiveness.7–9
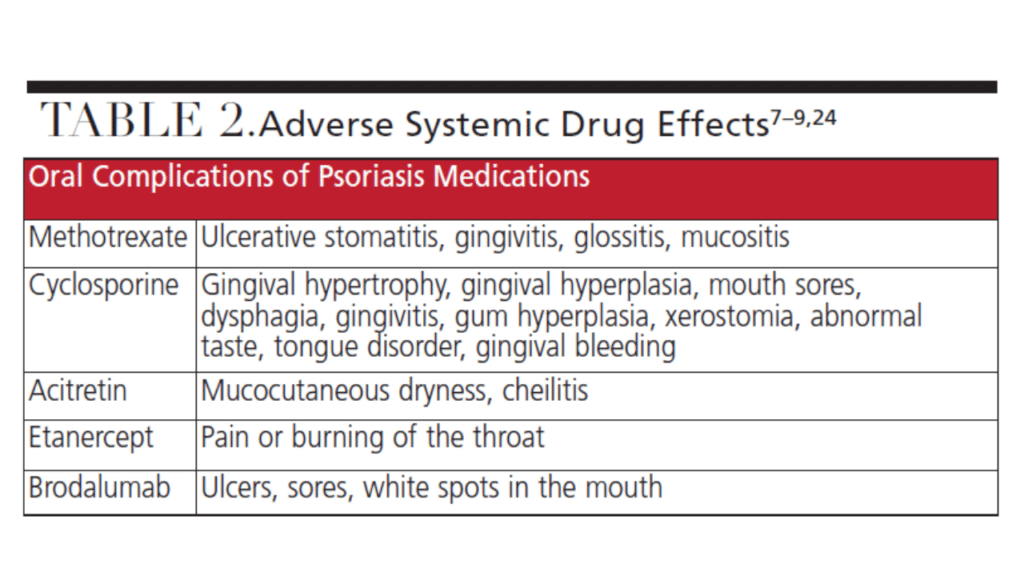
Corticosteroid topical treatment is often used for mild to moderate cases. Systemic treatments — including phototherapy and immunosuppressives, such as methotrexate, cyclosporin and biologics — are often used to treat moderate to severe psoriasis or when topical therapy is ineffective.22 Table 2 lists the adverse reactions of systemic medications commonly used to treat mild to severe psoriasis.
CHARACTERISTICS OF ORAL PSORIASIS
Data regarding oral manifestations of psoriasis are limited; however, oral complications of psoriasis can occur. The clinical appearance of oral psoriasis may be misleading, as it may resemble more common lesions, including atrophic candidiasis, stomatitis, diffuse oral erythema, geographic tongue, fissured tongue, erythema migraine, angular cheilitis, Reiter syndrome, erythema circinate, lichen planus, pemphigoid or leukoplakia.3,23,24 Oral psoriasis lesions are typically asymptomatic; thus, biopsies are rarely done, so lesions are often not reported.25 If an oral lesion is detected and treated, an inadequate response to topical or systemic treatments or a biopsy may lead to a differential diagnosis of oral psoriasis.3,23
Oral psoriatic lesions may affect different areas of the oral cavity, including the lips, tongue, palate, buccal mucosa and gingiva.24,25 The buccal mucosa is most frequently involved, while lesions affecting the vermillion border, gingiva and palate are less common.3,24 Oral manifestations vary in duration or location in conjunction with clinical fluctuations of the cutaneous disease.
Clinically, oral psoriasis may be classified into four categories: well-defined gray to yellowish-white round to oval lesions on the mucosa or tongue that are independent of cutaneous lesions; lacy, circinate, white elevated lesions that parallel cutaneous lesions; intense erythema of the entire oral mucosa; and benign migratory glossitis. Fissured tongue and geographic tongue may be the most common oral findings in this patient population, as these conditions occur in 33%, and 10% to 14% of psoriasis cases, respectively.3,23–25
ORAL HEALTH MANAGEMENT
Dental teams must be cognizant of management techniques to identify and treat the oral manifestations of psoriasis. A thorough patient interview using open-ended questioning to allow the patient to divulge pertinent medical information is necessary, and updates to the medical history should include any medication changes, as these can trigger or aggravate psoriasis. Patients should be educated about medication interactions and their potential effect on cutaneous lesions.7,21 Blood pressure should also be documented at each appointment due to increased risk of adverse cardiovascular events among patients with psoriasis.16 In addition, consultation with the patient’s primary care physician may be useful to clarify medical issues that could require modifications in dental management.5
Several systemic drugs approved to treat psoriasis may have side effects on oral tissues (Table 2).22,25 Drug-induced xerostomia should be treated by recommending increased water intake, use of adjuncts that stimulate salivary production or saliva replacements, and avoidance of products containing alcohol, which can further dry oral mucosa. Patients with psoriasis who experience stomatitis, mucositis and glossitis should be advised to avoid irritants — including hot or spicy foods, alcohol and tobacco — and use palliative treatments, such as mucosal protectants or topical anesthetic agents.25
Patients presenting with gingival hyperplasia may require more frequent oral prophylaxis and more rigorous self-care, including increased flossing in an effort to reduce bacterial biofilm. Full-mouth scaling and root planing, followed by mouthrinsing with 0.2% chlorhexidine gluconate solution for two minutes, and subgingival irrigation of pockets with a 1% chlorhexidine gel may result in significant clinical improvements for patients experiencing drug-induced gingival overgrowth.26
During the medical history, clinicians should ask questions regarding lifestyle habits, including tobacco and alcohol use, diet and exercise. Patients should be encouraged to adopt healthy lifestyle changes, including smoking cessation, which may prevent onset and alleviate psoriasis disease severity, improve quality of life, and lengthen life span.16,27 Additionally, alcohol abstinence may induce remission of psoriatic lesions.28 Patients should also be encouraged to minimize their cardiovascular risk factors to prevent incidents that may cause damage to the heart muscle.
To identify oral psoriatic lesions or changes in the oral environment, a thorough examination of oral tissues — including the lips, tongue, palate, buccal mucosa and gingiva — should be completed at every appointment. Oral manifestations suggestive of psoriasis may include small whitish papules, red and whitish plaques, or bright red patches. Clinicians should document the size, shape, location, severity, and duration of any findings in the patient record, and also notify the patient. In the event a lesion cannot be definitively diagnosed, the provider should consider a referral for a histological assessment to rule out differentiating pathology.25
If an oral lesion is detected or if a patient reports adverse oral effects from systemic psoriasis treatments, clinicians may recommend palliative treatments, such as topical anesthetic agents, topical corticosteroids, emollient toothpaste as a mucosal protectant, or saliva substitutes to reduce irritation. Dental teams should focus on removing irritants and biofilm, provide restorative treatment for caries lesions, adjust poorly fitting prostheses, and ensure the integrity of existing teeth to improve or maintain clinical outcomes.25
The temporomandibular joint (TMJ) of patients with psoriasis should also be evaluated at each appointment by performing a thorough extraoral examination. This may include an evaluation of the patient’s ability to open and close, palpation of the TMJ and masticatory and cervical muscles to detect tenderness and nodularity, and asking open-ended questions concerning symptoms. Clinicians may also consider recommending imaging techniques, including radiographs, computed tomography, scintigraphy, ultrasound, or magnetic resonance imaging, to diagnose or evaluate the extent of TMJ disorder related to psoriatic arthritis.29
Patients who experience TMJ symptoms due to psoriatic arthritis may present with limited opening and jaw fatigue. A mouth prop, multiple breaks and shorter appointments may make dental treatment more comfortable. Management options include biologics, disease-modifying antirheumatic drugs, NSAIDs, jaw rest with a soft diet, avoidance of wide mouth opening, and physiotherapy to slow or prevent the degradation of the TMJ.29 A custom nightguard or soft occlusal splint may also be prescribed as a palliative treatment or to prevent further damage to the TMJ.
ADDITIONAL CONSIDERATIONS
Oral health professionals should also be aware of the emotional toll psoriasis may take on patients and encourage them to pursue stress-relieving activities. Self-esteem and body image issues related to visible psoriatic lesions may impact both self-care habits and scheduling of dental appointments. If the clinician notes the patient is experiencing significant distress, it is important to explore the issue and decide whether referral to a mental health professional or dermatologic support group might help. Additionally, patients should be educated about the relationship between stress and cutaneous lesions.
Patients with cutaneous psoriasis may experience cracked, itching, sore or bleeding skin, which can make oral self-care difficult.25 Moreover, patients with psoriatic arthritis may have inflammation of the interphalangeal and metacarpophalangeal joints of the hands or ankylosis of the wrist in late stages, which can affect dexterity and fine motor skills.30
Clinicians should evaluate the ability of these patients to complete self-care by asking questions about dexterity, observing oral hygiene techniques, and assessing plaque and calculus accretion levels. Dental teams should also consider recommending products or appropriate adjuncts that may assist in effective oral self-care. Manual toothbrush adaptations, including brushes with a widened or elongated handle, may assist with more effective biofilm control. Self-care may also be improved for patients with dexterity issues by recommending a powered toothbrush or flosser, use of an interproximal oral irrigator, or using a long-handled floss holder instead of string floss.
Due to the association of systemic inflammation and psoriatic disease exacerbation, reducing oral inflammation is imperative. Patients should be educated about the importance of meticulous self-care and strategies to promote effective daily biofilm removal. Controlling oral inflammation with nonsurgical periodontal therapy and excellent self-care should be considered a vital management strategy for patients with psoriasis and periodontitis.31
A thorough clinical inspection of the alveolar tissue, as well as periodontal evaluation, at each appointment will allow providers to assess any signs of inflammation, bleeding and disease progression, which may indicate worsening of the periodontal status. More frequent recare appointments (every three to four months) or referral to a periodontist to address periodontal instability should be considered.
CONCLUSION
Psoriasis is a complex immune-mediated disorder of the skin, nails, scalp and joints. It is associated with several systemic comorbidities and overall increased mortality. Oral psoriasis may reveal mucosal lesions, affect the periodontium, and cause joint inflammation, which can compromise the patient’s quality of life and ability to perform self-care. Moreover, medications used to treat psoriasis may negatively impact oral tissues. Dental teams should be aware of psoriatic conditions in order to modify treatment (as needed), anticipate complications, and educate patients about lifestyle and self-care modifications that will support optimal oral health.
References
- Younai FS, Phelan JA. Oral mucositis with features of psoriasis: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:61–67.
- Menter A. Psoriasis and psoriatic arthritis overview. Am J Manag Care. 2016;22(Suppl 8):s216–s224.
- Fatahzadeh M. Manifestation of psoriasis in the oral cavity. Quintessence Int. 2016;47:241–247.
- Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361:496–509.
- Brooks JK. Psoriasis: a review of systemic comorbidities and dental management considerations. Quintessence Int. 2018;49:209–217.
- National Psoriasis Foundation. About Psoriasis. Available at: https://www.psoriasis.org/about-psoriasis/. Accessed February 27, 2023.
- Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. Lancet. 2021;397:1301–1315.
- Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20:1475.
- Kim WB, Jerome D, Yeung J. Diagnosis and management of psoriasis. Can Fam Physician. 2017;63:278–285.
- Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423–441.
- Langenbruch A, Radtke MA, Krensel M, Jacobi A, Reich K, Augustin M. Nail involvement as a predictor of concomitant psoriatic arthritis in patients with psoriasis. Br J Dermatol. 2014;171:1123–1128.
- Gelfand JM, Dommasch ED, Shin DB, et al. The risk of stroke in patients with psoriasis. J Invest Dermatol. 2009;129:2411–2418.
- Shahwan KT, Kimball AB. Psoriasis and cardiovascular disease. Med Clin North Am. 2015;99:1227–1242.
- Wu JJ, Choi YM, Bebchuk JD. Risk of myocardial infarction in psoriasis patients: a retrospective cohort study. J Dermatolog Treat. 2015;26:230–234.
- Armesto S, Santos-Juanes J, Galache-Osuna C, Martinez-Camblor P, Coto E, Coto-Segura P. Psoriasis and type 2 diabetes risk among psoriatic patients in a Spanish population. Australas J Dermatol. 2012;53:128–130.
- Salihbegovic EM, Hadzigrahic N, Suljagic E, et al. Psoriasis and dyslipidemia. Mater Sociomed. 2015;27:15–17.
- Onumah N, Kircik LH. Psoriasis and its comorbidities. J Drugs Dermatol. 2012;11(Suppl 5):s5–s10.
- Herron MD, Hinckley M, Hoffman MS, et al. Impact of obesity and smoking on psoriasis presentation and management. Arch Dermatol. 2005;141:1527–1534.
- Naldi L, Chatenoud L, Linder D, et al. Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: results from an Italian case-control study. J Invest Dermatol. 2005;125:61–67.
- Nussbaum L, Chen YL, Ogg GS. Role of regulatory T cells in psoriasis pathogenesis and treatment. Br J Dermatol. 2021;184:14–24.
- Fry L, Baker BS. Triggering psoriasis: the role of infections and medications. Clin Dermatol. 2007;25:606–615.
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445–1486.
- Daneshpazhooh M, Moslehi H, Akhyani M, Etesami M. Tongue lesions in psoriasis: a controlled study. BMC Dermatol. 2004;4:16.
- Yesudian PD, Chalmers RJ, Warren RB, Griffiths CE. In search of oral psoriasis. Arch Dermatol Res. 2012;304:1–5.
- Dreyer LN, Brown GC. Oral manifestations of psoriasis. Clinical presentation and management. N Y State Dent J. 2012;78:14–18.
- Pundir AJ, Pundir S, Yeltiwar RK, Farista S, Gopinath V, Srinivas TS. Treatment of drug-induced gingival overgrowth by full-mouth disinfection: A non-surgical approach. J Indian Soc Periodontol. 2014;18:311–315.
- Poikolainen K, Karvonen J, Pukkala E. Excess mortality related to alcohol and smoking among hospital-treated patients with psoriasis. Arch Dermatol. 1999;135:1490–1493.
- Higgins E. Alcohol, smoking and psoriasis. Clin Exp Dermatol. 2000;25:107–110.
- National Psoriasis Foundation. When PSA Invades the Jaw. Available at: https://www.psoriasis.org/advance/when-psa-invades-the-jaw/. Accessed February 27, 2023.
- Sankowski AJ, Lebkowska UM, Cwikła J, Walecka I, Walecki J. Psoriatic arthritis. Pol J Radiol. 2013;78:7–17.
- Ucan Yarkac F, Ogrum A, Gokturk O. Effects of non-surgical periodontal therapy on inflammatory markers of psoriasis: a randomized controlled trial. J Clin Periodontol. 2020;47:193–201.
From Decisions in Dentistry. April 2023;9(4):34-36,39.