SOUTH_AGENCY/E+/GETTY IMAGES PLUS
SOUTH_AGENCY/E+/GETTY IMAGES PLUS
Caries Prevention and Management in Light of The COVID-19 Pandemic
The following strategies for caries prevention and management will help reduce the risk of SARS-CoV-2 transmission during routine dental care.
The current COVID-19 pandemic is the worst global health crisis in more than a century. It has impacted a wide range of small to large businesses, including nonurgent health care services — such as those delivered by dentists. Oral health providers were thought to be at increased risk of COVID-19 exposure in clinic due to high salivary titres of SARS-CoV-2 and bioaerosols produced during aerosol-generating procedures (AGPs).1 A recent study, however, discovered that saliva of several asymptomatic patients contained only low copy numbers of SARS-CoV-2, while no viral particles were detected in the aerosols emitted from these patients.2 This suggests dental procedures — such as caries prevention and management — are moderately low risk if appropriate infection control measures are implemented.2
This is corroborated by a recent a study in the Journal of the American Dental Association that reported the prevalence of COVID-19 infection among dentists as less than 1%.3 Thus, available evidence indicates infection prevention protocols have been effective in limiting transmisson in dental settings. While there is evidence that aerosol risk is minimal, the supporting study is limited by its small sample size;2 thus, dental providers should not lower their guard until additional evidence is available. Toward this goal, the U.S. Centers for Disease Control and Prevention (CDC) and American Dental Association recommend focusing on early stage caries prevention and nonsurgical, nonaerosolizing caries management measures to further reduce the risk.4,5
As one example, the University of California, San Francisco School of Dentistry used these strategies as the first line of defense during the pandemic. Private practices, however, may bear conflicting perspectives because their predominantly business-type compensation model can be a potential barrier to embracing inexpensive or non-insured preventive and nonsurgical approaches. As a result, reimbursement policies must be revised to ensure the financial viability of nonoperative, nonaerosolizing treatments.
The advent of COVID-19 presents unique challenges to oral health care. Among these are implementing new infection prevention measures, reorganizing the dental setup at clinics, and addressing the burden of oral diseases that worsened after some patients delayed care due to pandemic-driven clinic shutdowns and/or fear of transmission during treatment. In response, the dental community has collaborated to develop safer delivery methods. This pandemic has increased awareness of the dangers posed by COVID variants and other airborne viruses capable of causing outbreaks. In the future, the profession must be prepared to deal with such scenarios.
The goal of this article is to serve as a road map for reducing the amount of aerosols emitted during caries prevention and management therapies. These approaches are feasible for implementation during and after the pandemic; consequently, dentists may wish to consider these techniques while planning care based on specific patient needs and operator expertise. Ultimately, these modalities are valuable conservative tools in the armamentarium for general dental care.
INFECTION PREVENTION
Dental caries that necessitate the use of high-speed handpieces and air-water sprays have the potential to disperse aerosols and spread infection. Thus, besides ensuring proper personal protective equipment, clinicians are advised to minimize risk during AGPs by using a combination of dental dams, suction devices, and four-handed dentistry with the help of a trained assistant.4,5 Due to their high efficacy in minimizing bioaerosols, high-volume evacuators become an obligatory requirement.6 Although some preprocedural oral rinses have been shown to reduce contamination by nearly 64.8%, additional evidence is needed to support this claim.7
Other measures, such as high efficiency particulate air filters, proper ventilation and other engineering controls, should be implemented to reduce risk of infection via bioaerosols. Reorganizing daily appointments to segregate AGPs and non-AGPs, and using faster techniques when possible, can shorten interaction times and optimize in-person visits. Additionally, patients’ COVID-19 vaccination records can be verified and uploaded into medical records prior to dental visits. For unvaccinated individuals, a negative COVID test can be mandated one to 72 hours prior to undertaking AGPs. Furthermore, dentists may consider using rapid antigen screening to test patients before administering elective treatment. Similarly, vaccination of dentists and auxiliaries is advocated. As per updated CDC guidelines, asymptomatic dental personnel, regardless of vaccination status, should take a series of two SARS-CoV-2 viral tests immediately, and five to seven days after, a potential high-risk exposure to AGPs.8
It is essential that caries prevention remains at the forefront of dental care to enable patients to be as self-sufficient as possible. Clinicians should use their judgement to propose sustainable modalities according to patient needs and preferences, and consistently reinforce preventive education.
CONVENTIONAL CARIES PREVENTION STRATEGIES
Health behavior modifications: Irrespective of the lesion or clinical situation, patients should be counselled on using fluoridated toothpaste, exercising dietary control, and appropriate biofilm management techniques to improve oral hygiene and reduce cariogenic factors.
Biological approach: Community water fluoridation, fluoride supplements and topical fluorides — such as 2% sodium fluoride (NaF), 1.23% acidulated phosphate fluoride gels, and 5% NaF varnishes — are proven strategies for decreasing the incidence and prevalence of caries. These remain the gold standard for caries prevention.9 Supported by a large body of evidence, their ease of administration, short application time, and limited aerosol risk (without the need for prior prophylaxis) make them suitable candidates for caries prevention during the current pandemic and beyond.
ADDITIONAL MEANS OF PREVENTION
Non-fluoride agents: Arginine toothpastes, chlorhexidine/thymol varnishes, xylitol lozenges, chewing gum and syrups, triclosan, casein phosphopeptide-amorphous calcium phosphate, and toothpastes containing bioactive glass are suggested to provide a synergistic action in the caries-preventive effect of fluorides.10,11 These agents are recommended for children and higher caries-risk adults as adjuncts to primary preventive strategies.11
Ecological approach: An ecological shift within the plaque biofilm contributes to initiation and progression of caries. Consequently, clinicians may recommend antimicrobial polypeptides to control and modify biofilms, prebiotics and probiotics (such milk and naturally occurring oral commensals) to promote growth and dominance of oral commensal species, and quorum sensing targets (such as methanol extracts) to disturb cell-to-cell communication.12,13 Natural products — including licorice, propolis, cranberry extract and phytochemicals — inhibit bacterial growth, glucan synthesis and bacterial adhesion.12,13 Targeted replacement of Streptococcus mutans with less virulent “designer” bacteria within the same ecological niche could reduce overall cariogenicity of the biofilm.12 These products have shown promising results in maintaining a healthy, non-cariogenic plaque ecology and can be incorporated in toothpaste, mouthrinse or food products. Many are still in experimental phases, with controversial evidence, and at present are costly for wide-scale implementation. However, if thoroughly explored, these approaches have the potential to bring about a paradigm shift in long-term caries prevention to a more biological model.12
Technological approach: Ozone therapy reduces the cariogenic bacterial load on a biofilm, slows caries progression and accelerates remineralization.14 If considered for use, delivery in an ozonated oil or water form may be safer than a gas form in the interest of reducing bioaerosols during the pandemic. Together with conventional techniques, carbon dioxide, neodymium-doped yttrium aluminum garnet (Nd:YAG), erbium-doped yttrium aluminum garnet (Er:YAG), erbium chromium yttrium scandium gallium garnet (Er,Cr:YSGG) and argon lasers used at subablative levels have shown promising results in reducing caries incidence by increasing acid resistance of enamel and improving sealant retention.15 The use of Er,Cr:YSGG lasers for caries preparation seems to generate fewer aerosols than high-speed rotary instruments, reducing the risk of aerosol transmission.16
The increased use of teledentistry offers opportunities for dentists to safely maintain efforts in consulting, triaging, educating and motivating patients during and after the pandemic. Similar to telehealth models, teledentistry can be implemented via synchronous, asynchronous, mobile health and remote patient monitoring modalities.17 Prior telescreening of patients through secure platforms can reduce face-to-face interactions and allow for planning and optimization of treatment visits. In some cases, smartphones, tablets and laptops can serve as caries detection tools and reinforce preventive education in the COVID-19 era.
CARIES MANAGEMENT
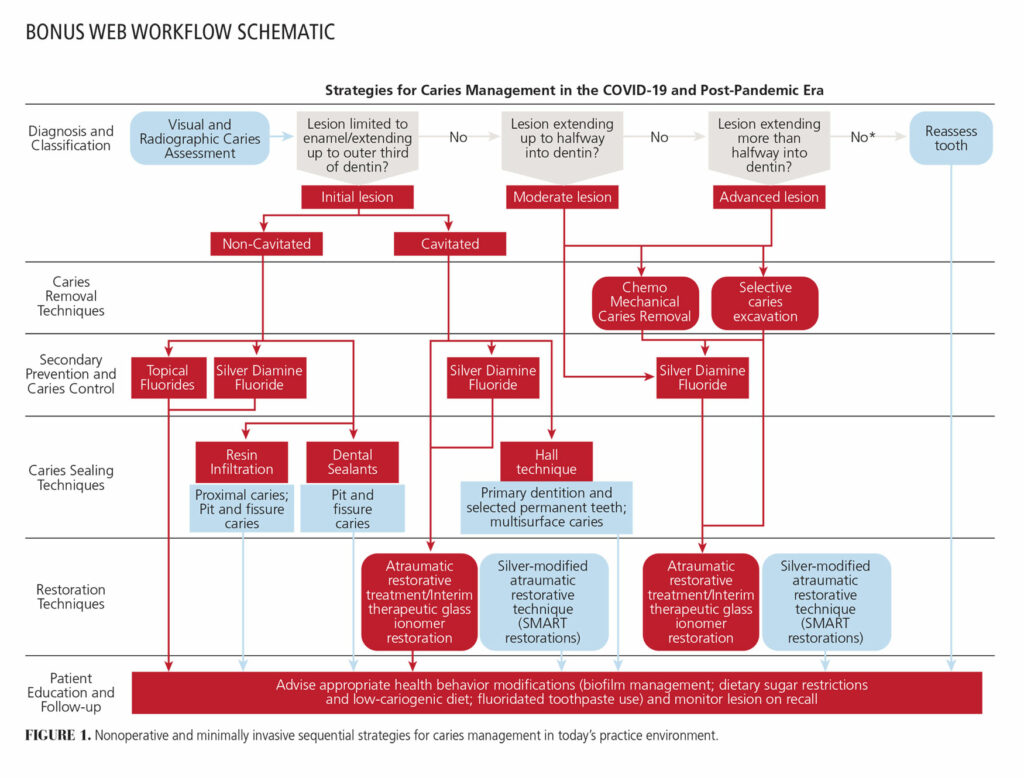
Depending on the situation and patient needs, it may be beneficial to employ nonoperative, nonaerosolizing approaches to caries management before attempting operative interventions. Available exclusively in the online version of this article, a workflow schematic outlines minimally invasive sequential management strategies for consideration during the COVID-19 pandemic and beyond. Evidence-based rationales behind the selection of technique should be discussed with patients to encourage shared decision-making.
Silver diamine fluoride (SDF): The application of SDF, a caries arresting agent, can be helpful in managing early stage lesions, cavitated dentin lesions, root caries, and multi-surface lesions requiring caries control.18,19 Its efficacy in arresting caries in primary dentition and preventing root caries in older adults has been widely proven.20 Evidence suggests SDF performs superiorly in anterior applications,19 but the material’s unesthetic staining potential can incite refusals from patients. Clinicians must wrestle with matching evidence to patient preferences in such scenarios.
Because it requires no drilling or caries removal, SDF may be advantageous in limiting aerosol risk. It is inexpensive, compatible with several caries management techniques, and can be quickly applied with a microbrush, reducing chairtime. Silver-modified atraumatic restorative therapy or SMART restorations21 involve immediate restoration of a carious tooth after SDF application in a single sitting, thus maximizing the clinical benefits of the patient visit. Nevertheless, meticulous follow-up is needed to ensure adequate caries arrest and restoration integrity.
Sealing techniques — resin infiltration: In this technique, a low-viscosity resin is infiltrated into microporosities of the affected enamel surface in a single visit. This provides mechanical stability to the microcavitated enamel, limits caries progression, and improves the esthetics of white spot lesions by partially masking discolorations.22,23 This approach carries a moderate-strength recommendation for initial proximal lesions.24 Although use of the air-water syringe in this technique adds a low risk of producing aerosols, when coupled with rubber dams and high-volume evacuators, infiltration is still plausible for use during the pandemic.
Sealing techniques — dental sealants: Application of dental sealants can prevent caries and halt lesion progression by mechanically sealing deep fissures and inhibiting the ingress of microorganisms without the need for tooth removal, especially in initial enamel lesions.25 The choice between resin-based sealants and glass ionomer sealants is significant with respect to aerosol generation, as resin-based sealants require rinsing using an air-water syringe. Glass ionomers are a promising alternative despite their lower retention rates,25 as they reduce aerosol risk and also provide a fluoride-releasing caries preventive effect.
Sealing techniques — Hall technique: This method follows the hypothesis that complete coronal coverage under a preformed metal crown will seal caries from the external cariogenic environment and thus prevent further progression.26 With no need for drilling, it is beneficial during the pandemic. In primary teeth, the Hall technique demonstrates a high evidence of success in managing multi-surface caries not involving the pulp.26
However, insufficient evidence and concerns regarding a lack of occlusal equilibration post-insertion limit its application in permanent teeth. Nevertheless, this approach may be worth considering for older adults during the pandemic, as these crowns may be used to treat initial lesions on attrited carious teeth, and serve as interim options for permanent teeth with no opposing dentition before any definitive prosthetic rehabilitation can be provided. Contrary to primary teeth, Hall crowns are usually considered as a temporary solution in permanent dentition, and future visits requiring AGPs may be needed for more definitive treatment.
CARIES REMOVAL METHODS
Chemomechanical caries removal (CMCR): This approach employs enzymatic or chemical caries removal agents to alter dentinal tissue containing bacterially loaded, disorganized collagen structure, leaving structurally remineralized dentin unaltered. Altered dentin can be scooped out using dental excavators and specialized hand instruments. Although CMCR is time-consuming, resulting in longer appointments, use of this technique may be justified, as CMCR with enzyme-based agents requires shorter excavation time compared to using only hand instruments.27
Selective caries excavation: This minimally invasive concept involves partial excavation of caries up to soft or leathery dentin in deep carious lesions, or up to firm dentin in lesions that are limited to the inner third of dentin prior to restoration.28 It is imperative that all caries on the preparation walls and cavosurface are removed to ensure a proper marginal seal.
RESTORATIVE TECHNIQUES
Atraumatic restorative treatment (ART) and interim therapeutic restorations (ITR): While the goals for ART and ITR differ, they share a similar approach. Use of ITRs can be adapted to resemble ART for the pandemic by hand excavation and direct restoration with glass ionomers; this eliminates AGPs. Although both modalities are good short-term alternatives for stabilizing the dentition, these restorations may need to be revisited for more definitive treatment with conventional restorative techniques. This is especially true for primary teeth due to reported higher failure rates29 and for management of multi-surface caries due to the limited clinical data on the long-term performance of multi-surface restorations.30
CONCLUSION
While evidence suggests the risk of COVID-19 transmission in dental settings is low, clinicians must not become complacent. Airtight infection prevention protocols must be maintained to prevent additional waves of the outbreak or newer mutations. With the advent of vaccinations, and as daily activities return to some semblance of normal, practitioners can expect an increase in service utilization by patients who previously postponed care. Under this scenario, untreated caries and advancing lesions are likely to be among the most common cases to manage.
The current pandemic presents an opportunity for dentists to explore prevention-centric and minimally invasive caries management approaches in accordance with evidence, patient needs, and clinical situations before resorting to the “drill and fill” mindset.
Key Takeaways
- Evidence suggests dental treatment — such as caries prevention and management — is moderately low risk for SARS-CoV-2 transmission if appropriate infection control measures are implemented.2
- In today’s practice setting, the U.S. Centers for Disease Control and Prevention and American Dental Association recommend focusing on early stage caries prevention and nonsurgical, nonaerosolizing caries management measures to further reduce the risk of transmission posed by dental aerosols.4,5
- This article serves as a road map for reducing the amount of aerosols emitted during caries prevention and management therapies.
- While these approaches are feasible for implementation during and after the pandemic, ultimately, these techniques are valuable conservative tools in the armamentarium for general dental care.
- Depending on the clinical situation and patient needs, it may be beneficial to employ effective nonoperative, nonaerosolizing approaches to caries management before attempting operative interventions.
- Evidence-based rationales behind the selection of technique should be discussed with patients to encourage shared clinical decision-making.
REFERENCES
- Wyllie AL, Fournier J, Casanovas-Massana A, et al. Saliva or nasopharyngeal swab specimens for detection of SARS-CoV-2. N Engl J Med. 2020;383:1283–1286.
- Meethil AP, Saraswat S, Chaudhary PP, Dabdoub SM, Kumar PS. Sources of SARS-CoV-2 and other microorganisms in dental aerosols. J Dent Res. 2021;100:817–823.
- Estrich C, Mikkelsen M, Morrissey R, et al. Estimating COVID-19 prevalence and infection control practices among U.S.dentists. J Am Dent Assoc. 2020;151:815–824.
- U.S. Centers for Disease Control and Prevention. Guidance for Dental Settings. Available at: www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html. Accessed August 4, 2021.
- American Dental Association. Summary of ADA Guidance During the COVID-19 Crisis. Available at: https://www.wsda.org/docs/librariesprovider52/default-document-library/summary-of-ada-guidance-during-the-sars-cov-2-crisis.pdf?sfvrsn=0. Accessed August 4, 2021.
- Samaranayake LP, Fakhruddin KS, Buranawat B, Panduwawala C. The efficacy of bio-aerosol reducing procedures used in dentistry: a systematic review. Acta Odontol Scand. 2021;79:69–80.
- Marui VC, Souto ML, Rovai ES, Romito GA, Chambrone L, Pannuti CM. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: a systematic review. J Am Dent Assoc. 2019;150:1015–1026.e1.
- U.S. Centers for Disease Control and Prevention. Updated Healthcare Infection Prevention and Control Recommendations in Response to COVID-19 Vaccination. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-after-vaccination.html. Accessed August 4, 2021.
- Recommendations for using fluoride to prevent and control dental caries in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2001;50(RR-14):1–42.
- Wang Y, Li J, Sun W, Li H, Cannon RD, Mei L. Effect of non-fluoride agents on the prevention of dental caries in primary dentition: a systematic review. PLoS One. 2017;12:e0182221.
- Rethman MP, Beltrán-Aguilar ED, Billings RJ, et al. Nonfluoride caries-preventive agents: executive summary of evidence-based clinical recommendations. J Am Dent Assoc. 2011;142:1065–1071.
- Philip N, Suneja B, Walsh LJ. Ecological approaches to dental caries prevention: paradigm shift or shibboleth? Caries Res. 2018;52:153–165.
- Chen X, Daliri EB, Kim N, Kim JR, Yoo D, Oh DH. Microbial etiology and prevention of dental caries: exploiting natural products to inhibit cariogenic biofilms. Pathogens. 2020;9:569.
- Almaz ME, Sönmez IŞ. Ozone therapy in the management and prevention of caries. J Formos Med Assoc. 2015;114:3–11.
- Pagano S, Lombardo G, Orso M, Abraha I, Capobianco B, Cianetti S. Lasers to prevent dental caries: a systematic review. BMJ Open. 2020;10:e038638.
- Abdelkarim-Elafifi H, Arnabat-Artés C, Parada-Avendaño I, Polonsky M, Arnabat-Domínguez J. Aerosols generation using Er,Cr:YSGG laser compared to rotary instruments in conservative dentistry: a preliminary study. J Clin Exp Dent. 2021;13:e30–e36.
- American Dental Association. ADA policy on teledentistry. Available at: www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-teledentistry. Accessed August 4, 2021.
- Horst JA, Ellenikiotis H, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc. 2016;44:16–28.
- Fung MH, Duangthip D, Wong MC, Lo EC, Chu CH. Randomized clinical trial of 12% and 38% silver diamine fluoride treatment. J Dent Res. 2018;97:171–178.
- Seifo N, Cassie H, Radford JR, Innes NP. Silver diamine fluoride for managing carious lesions: an umbrella review. BMC Oral Health. 2019;19:145.
- Alvear Fa B, Jew JA, Wong A, Young D. Silver modified atraumatic restorative technique (SMART): an alternative caries prevention tool. Stomatology Edu J. 2016;3:243–248.
- Doméjean S, Ducamp R, Léger S, Holmgren C. Resin infiltration of non-cavitated caries lesions: a systematic review. Med Princ Pract. 2015;24:216–221.
- Borges AB, Caneppele TM, Masterson D, Maia LC. Is resin infiltration an effective esthetic treatment for enamel development defects and white spot lesions? A systematic review. J Dent. 2017;56:11–18.
- Schwendicke F, Splieth CH, Bottenberg P, et al. How to intervene in the caries process in adults: proximal and secondary caries? An EFCD-ORCA-DGZ expert Delphi consensus statement. Clin Oral Investig. 2020;24:3315–3321.
- Wright JT, Tampi MP, Graham L, et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars. Pediatr Dent. 2016;38:282–308.
- Innes NP, Evans DJ, Bonifacio CC, et al. The Hall technique 10 years on: questions and answers. Br Dent J. 2017;222:478–483.
- Schwendicke F. Chemomechanical excavation is more time-consuming than rotary, but not necessarily hand excavation. J Evid Based Dent Pract. 2015;15:190–192.
- Schwendicke F, Frencken JE, Bjørndal L, et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res. 2016;28:58–67.
- Dorri M, Martinez-Zapata MJ, Walsh T, Marinho VC, Sheiham A, Zaror C. Atraumatic restorative treatment versus conventional restorative treatment for managing dental caries. Cochrane Database Syst Rev. 2017;12:CD008072.
- de Amorim RG, Frencken JE, Raggio DP, Chen X, Hu X, Leal SC. Survival percentages of atraumatic restorative treatment (ART) restorations and sealants in posterior teeth: an updated systematic review and meta-analysis. Clin Oral Investig. 2018;22:2703–2725.
From Decisions in Dentistry. September 2021;7(9):10-13.