 ALEKSANDAR JANKOVIC / ISTOCK / GETTY IMAGES PLUS
ALEKSANDAR JANKOVIC / ISTOCK / GETTY IMAGES PLUS
Broadening Clinical Perspectives on Inferior Alveolar Nerve Blocks
In addition to the conventional Halsted inferior alveolar nerve block and two well-known alternatives, this discussion will examine key features of other mandibular block techniques and short needle approaches.
This course was published in the February 2023 issue and expires February 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 340
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the application of the Halsted inferior alveolar nerve block (HIANB)and its clinical success rate.
- Explain factors that can impact the development of anesthesia, as well as the use of HIANB alternatives.
- Describe the short needle inferior alveolar and lingual nerve block technique.
Many clinicians have perfected their HIANB techniques and rarely experience failures. While this level of achievement is commendable, there remains a small window of failure. According to Madan et al,2 “In certain cases … this nerve block fails, even when performed by the most experienced clinician.” When using common techniques, confirmed by contact with the medial ramus near the mandibular foramen, profound anesthesia is not assured. While contacting bone is a common safety step to avoid penetration into the parotid gland, it does not necessarily ensure optimal deposition sites. A variety of factors can impact the development of anesthesia, such as accessory innervation, fibrous tissue resistance and deflection, and variability in the locations of neural, vascular, and bony structures and landmarks.
The abundance of alternative mandibular block techniques in the literature (20 were reviewed for this discussion), highlights the pervasive nature of mandibular anesthesia failure. In addition to the conventional HIANB and two well-known alternatives, this discussion will report key features of a few mandibular block techniques from the global literature. In addition, short needle approaches will be discussed.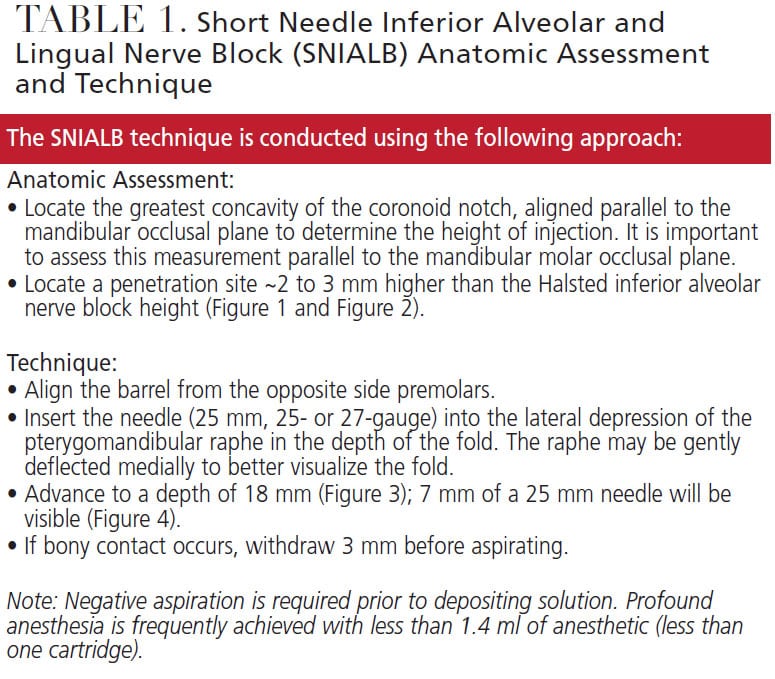
HALSTED INFERIOR ALVEOLAR NERVE BLOCK FAILURE
The HIANB is a common approach to anesthesia in the mandible.3,4 Despite widespread use, failure rates ranging from 15% to 20% or more — even after a second injection — have been reported.5,6 Some studies suggest even higher failure rates. Potocnik and Bajrović7 note that “even when a traditional inferior alveolar technique is employed, clinical studies show that [it] fails in approximately 30% to 40% of cases.”
Numerous sources describe alternative techniques that demonstrate higher success rates, such as the Gow-Gates and Vazirani-Akinosi nerve blocks (97.5% and as high as 95.7%, respectively).6–10 Although these techniques are reportedly more effective than the HIANB, they may not have been included in dental curriculum and, even when included, are less frequently performed compared to the HIANB.11 A study of Harvard School of Dental Medicine graduates, for example, reported that despite instruction in the HIANB, Gow-Gates and Vazirani-Akinosi blocks, most graduates did not incorporate Gow-Gates or Vazirani-Akinosi techniques into their anesthesia routines. The researchers estimated that only 3.7% to 16.1% used Gow-Gates blocks and 0.0% to 3.8% used Vazirani-Akinosi blocks as their method(s) of choice for achieving mandibular anesthesia.11
Most failures occur because anesthetic solution is not deposited into optimal locations within the pterygomandibular space. The most common reasons cited for failure include technique errors related to inaccurate assessment of landmarks and syringe position.3,9 Deposition posterior and/or inferior to nerves, anatomic barriers and variations, accessory innervation, needle deflection, armamentarium issues, and numerous other challenges have been cited, as well.3,9,12–20
In a study of 132 mandibles, Kilarkaje et al17 reported the relationship between the mandibular foramen and mandibular molar occlusal and alveolar crestal planes increases in height with age. As Gow-Gates21 noted, individual anatomic variations of mandibular foramina are described as being located higher than expected in a significant percentage of patients. Gow-Gates also commented that criticism of the HIANB technique “is based on unpredictable results from its use and the false premise that pulpal anesthesia is consistently attained by depositing the anaesthetic solution at the lingula.”21
GLOBAL PERSPECTIVES ON ALTERNATIVE TECHNIQUES
While the Gow-Gates and Vazirani-Akinosi techniques are well-known, from a global perspective there are many lesser-known alternatives to inferior alveolar nerve anesthesia. This article will present several examples to provide insight. It should be noted this review is a limited discussion and is not intended to provide instructions, or illustrations, for performing these techniques.
Kahlil20 discusses seven alternative HIANB techniques, two of which were described by Thangavelu et al.22 The first requires patients to open widely. Approaching from the contralateral side, needle insertion is ~8 to 10 mm posterior to the anterior border of the ramus and continues 6 to 8 mm until contact with bone. The syringe is then moved to the midline and the needle is advanced, making multiple contacts along the ramus. These repeated bony contacts may result in periosteal trauma. At a depth of 21 to 24 mm, the syringe is moved back to the contralateral side. The reported technique success rate is 95%.
The internal oblique ridge is the key landmark for the second Thangavelu et al22 technique. Approaching from the contralateral premolars, with the thumb over the retromolar area, insertion is 6 to 8 mm above the midpoint of the thumb and 2 mm posterior to the internal oblique ridge. Insertion continues until contact with bone. Both inferior alveolar and lingual nerves are anesthetized. The reported success rate is 95%.
A technique described by Boonsiriseth et al23 makes use of the HIANB penetration site; however, the syringe is aligned directly over the occlusal surfaces on the side to be anesthetized. With this technique, 30 mm needles are recommended and no bony contact with the ramus occurs.
Palti et al24 describe the intersection of two wires to predict the location of the mandibular foramen. One wire is positioned over the permanent first molar (or over the second primary molar), along the mesiobuccal groove and midpoint of the mesial slope of the distolingual cusp. The other wire is positioned over the contralateral occlusal plane.
Galdames et al25 recommend depositing anesthetic in the retromolar triangle, essentially accessing the inferior alveolar nerve via neural and vascular canals communicating with the mandibular canal. The success rate of this technique is reported to be 72%. While less successful than the HIANB, it is described as useful in patients on anticoagulant therapy or with bleeding disorders, such as hemophilia.
In Nooh’s and Abdullah’s26 technique, the syringe is aligned over the contralateral premolars and the needle is inserted 15 mm above the occlusal plane and advanced to bony contact. After contact with the ramus, the syringe is relocated to the side of injection over the teeth. The needle is then advanced 30 to 34 mm while remaining in contact with bone. Nooh and Abdullah claim this technique has fewer complications and lower positive aspiration and failure rates than the HIANB.
Takasugi et al27 describe depositing anesthetic solution between the medial pterygoid and temporalis muscles near the anterior border of the ramus, within the pterygomandibular space. This technique is referred to as an anterior inferior alveolar nerve block. Takasugi et al use computed tomography scans to predict syringe location and angle. With the syringe on the contralateral side, the needle is inserted 10 mm above the occlusal plane to a depth of 10 mm. Success is approximately 75%.
LOMA LINDA INFERIOR ALVEOLAR NERVE BLOCK — A SHORT NEEDLE TECHNIQUE
The Local Anesthesia Manual issued by the Loma Linda University School of Dentistry describes an inferior alveolar nerve block technique accomplished with short, 25-gauge needles.28 Key anatomic landmarks include the depth of the coronoid notch, internal oblique ridge, mandibular occlusal plane, pterygomandibular raphe and medial ramus. Inserting the needle to 5 mm, 0.5 ml of anesthetic is deposited for a lingual block. The needle is then advanced — maintaining contact with the ramus — until contact is lost over the lingular notch. Up to 1.0 ml of anesthetic is deposited after contact is lost. The success rate is estimated to be 80% to 85%.
SHORT NEEDLE INFERIOR ALVEOLAR AND LINGUAL NERVE BLOCK DISCUSSION
A short needle approach for inferior alveolar nerve blocks is used by many clinicians. This method follows HIANB penetration site landmarks, inserting short needles of varying gauges to depths anywhere from three-fourths to the full length of the needle (i.e., to the hub). Many learn the technique from colleagues, use it routinely, and anecdotally claim great success.
Despite the technique’s apparent success, deep insertions with short needles and routine penetrations to needle hubs are well-documented safety concerns.3,13,16 When reviewing the risks associated with short needles in deep penetrations, researchers have reported that needle diameter is a significant predisposing factor in needle fracture.13,16 In 31 of 40 cases (77.5%) where diameter was mentioned, 30-gauge needles were involved. While reliably effective, concerns persist over risks associated with deep insertions to the hub of short, and particularly small diameter, needles.3
Using cadavers with intact tissues, Menke and Gowgiel29 compared 25-gauge, 25 mm short needles versus 25-gauge, 36 mm long needles to determine which best approximated the location of the inferior alveolar nerve. Measuring penetration depths from the mucous membrane at the pterygomandibular raphe to the inferior alveolar nerve, the range was found to be 12 to 19 mm. This depth was noted to be within the limits of the short needles used in the study. The authors further observed that needle deflections were more frequent when long needles were used, and that long needles were more likely to deflect in a posterior direction from the mandibular foramen.29 Galbreath and Eklund30 provided evidence that depositions posterior to the foramen are likely to result in lower success rates (~50%) compared to depositions anterior to the foramen (~80%).

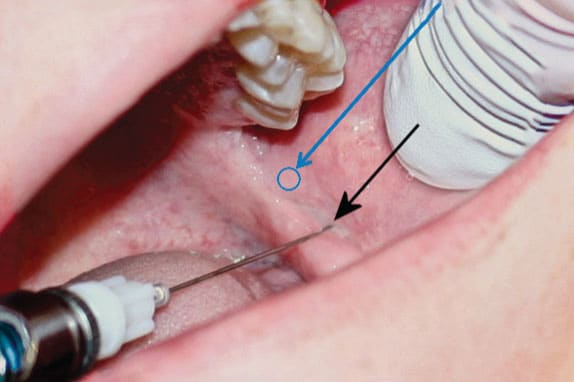
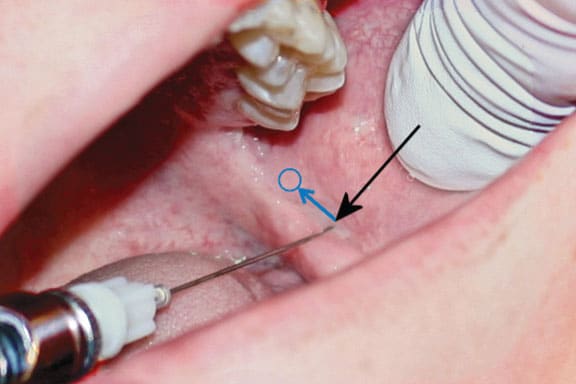
The penetration site recommended for the short needle inferior alveolar and lingual nerve block (SNIALB), based on Gow-Gates’ observation of false premise, is ~2 to 3 mm higher than Halsted penetration site (Figure 1).21,31 At this height, the insertion site is moved ~2 mm medially due to the curvature of the ascending pterygomandibular raphe (Figure 2). The average penetration depth (16 mm) reported by Menke and Gowgiel29 is increased to 18 mm to accommodate this change (Figure 3).
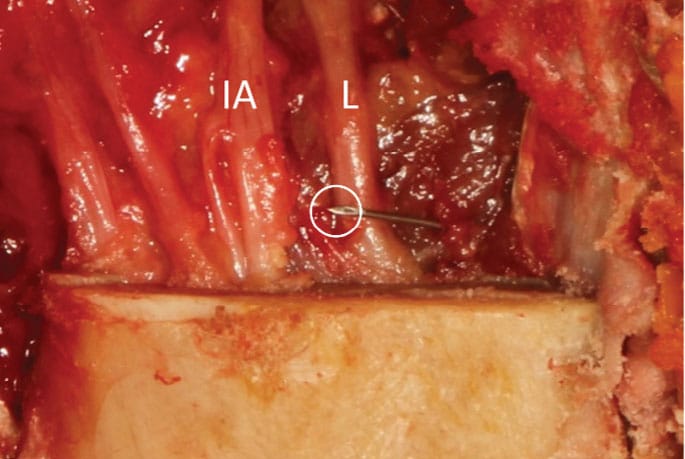
The SNIALB nerve block approach described in Table 1 differs significantly from most other techniques previously discussed. It relies on a high penetration site and shallow insertion depth to deposit solution close to the inferior alveolar nerve. This single deposition site routinely anesthetizes both the inferior alveolar and lingual nerves. Bony contact is not expected. If it occurs, the insertion depth should be decreased prior to deposition. Addressing concerns of inserting needles to the hub and/or the potential for needle fracture, at the recommended insertion depth of 18 mm, 7 mm of a 25 mm, 25-gauge needle (preferred) are exposed (Figure 4).
CLINICAL STUDY: SHORT NEEDLE INFERIOR ALVEOLAR AND LINGUAL NERVE BLOCKS
Menke and Gowgiel29 noted disagreement in the literature regarding the depth of penetration of needles for inferior alveolar nerve blocks. Their study of the actual depths of penetration from the mucous membrane of the penetration site to the inferior alveolar nerve were conducted using cadavers with intact tissues. Anatomic studies that did not account for soft tissue were described by the team as “not totally helpful to a clinician who is administering an inferior alveolar nerve block.”29 A blinded randomized controlled trial comparing the SNIALB to the HIANB is currently under way.
CONCLUSION
Achieving profound anesthesia with a traditional HIANB occurs, on average, 80% to 85% of the time or less. While the HIANB typically succeeds on repeat injection, failure is not uncommon. Clinicians who are unfamiliar with, or reluctant to perform, Gow-Gates or Vazirani-Akinosi blocks often rely on alternatives to supplement anesthesia. In this case, the SNIALB technique may prove clinically relevant.
References
- Mehta V. Key Steps for Success When an Inferior Alveolar Nerve Block Fails. Available at: https://www.speareducation.com/spear-review/떍/葑/key-steps-for-success-when-an-inferior-alveolar-nerve-block-fails?msclkid=b449a5bdce4b11ec834da0663f4edafb. Accessed January 4, 2023.
- Madan GA, Madan SG, Madan AD. Failure of inferior alveolar nerve block: exploring the alternatives. J Am Dent Assoc. 2002;133:843–846.
- Bassett KB, DiMarco AC, Naughton DK. Local Anesthesia for Dental Professionals. 2nd ed. Upper Saddle River, NJ: Pearson Education; 2022.
- Madan N, Kamath KS, Gopinath A, et al. A randomized controlled study comparing efficacy of classical and Gow-Gates technique for providing anesthesia during surgical removal of impacted mandibular third molar: A split mouth design. J Maxillofac Oral Surg. 2017;16:186–191.
- Malamed SF. Is the mandibular nerve block passe? J Am Dent Assoc. 2011;142:3s–7s.
- Kiran SR, Kashyap FM, Uppada UK, Tiwari P, Mishra A, Sachdeva A. Comparison of efficacy of Halstead, Vazirani Akinosi and Gow Gates techniques for mandibular anesthesia. J Maxillofac Oral Surg. 2018;17:570–575.
- Potocnik I, Bajrović F. Failure of inferior alveolar nerve block in endodontics. Endo Dent Traumatol.1999;15:247–251.
- Malamed SF. The Gow-Gates mandibular block. Evaluation after 4,275 cases. Oral Surg Oral Med Oral Pathol. 1981;51:463–467.
- Haas DA. Alternate mandibular block techniques: a review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J Dent Ed. 2011;142(Suppl 3):8S–12S.
- Shinagawa A, Chin VKL, Rabbani SR, Campos AC. A novel approach to intraoral mandibular nerve anesthesia: changing reference planes in the Gow Gates block technique. J Oral Maxillofac Surg. 2009;67:2609–2616.
- Johnson TM, Badovinac R, Shaefer J. Teaching alternatives to the standard inferior alveolar nerve block in dental education: outcomes in clinical practice. J Dent Educ. 2007;71:1145–1152.
- Hochman MN, Friedman MJ. In vitro study of needle deflection: a linear insertion technique versus a bidirectional rotation insertion technique. Quintessence Int. 2000;31:33–39.
- Acham S, Truschnegg A, Rugani P, et al. Needle fracture as a complication of dental local anesthesia: recommendations for prevention and a comprehensive treatment algorithm based on literature from the past four decades. Clin Oral Investig. 2019;23:1109–1119.
- Lopez AB, Diago MP. Failure of locoregional anesthesia in dental practice. Review of the literature. Med Oral Patol Oral Cir Bucal. 2006;11:E510–E513.
- Wolf KT, Brokaw EJ, Bell A, Joy A. Variant inferior alveolar nerves and implications for local anesthesia. Anesth Prog. 2016;63:84–90.
- Augello M, von Jackowski J, Gratz KW, Jacobsen C. Needle breakage during local anesthesia in the oral cavity — a retrospective of the last 50 years with guidelines for treatment and prevention. Clin Oral Investig. 2011;15:3–8.
- Kilarkaje N, Nayak SR, Narayan P, Prabhu LV. The location of the mandibular foramen maintains absolute bilateral symmetry in mandibles of different age-groups. Hong Kong Dent J. 2005;2:35–37.
- Akinosi JO. A new approach to the mandibular nerve block. Br J Oral Surg. 1977; 15:83–87.
- Hawkins M, Bassett K, Royer R. Dental Local Anesthesia: Techniques and Key Features. Available at: https://www.dentallearning.net/course/dental-local-anesthesia-techniques-and-key-features. Accessed January 4, 2023.
- Kahlil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res. 2014;8:3–8.
- Gow-Gates GAE. A new mandibular block technique using extra-oral and intra-oral landmarks. Master’s Thesis. Available at: https://ses.library.usyd.edu.au/handle/뗻/쁰. Accessed January 4, 2023.
- Thangavelu K, Sabita S, Kannan R, Saravanan K. Inferior alveolar nerve block using internal oblique ridge as landmark. SRM J Res Dent Sci. 2012;3:15–18.
- Boonsiriseth K, Sirintawat N, Arunakul K, Wongsirichat N. Comparative study of the novel and conventional injection approach for inferior alveolar nerve block. Int J Oral Maxillofac Surg. 2013;42:852–856.
- Palti DG, de Almeida CM, Rodrigues, AC, Andreo JC, Lima JEO. Anesthetic technique for inferior alveolar nerve block: a new approach. J Appl Oral Sci. 2011;19:11–15.
- Galdames ICS, López MGC, Matamala DAZ. Inferior alveolar nerve block anesthesia via the retromolar triangle, an alternative for patients with blood dyscrasias. Med Oral Patol Oral Cir Buccal. 2008;13:E43–E47.
- Nooh N, Abdullah W. Incidence of complications of inferior alveolar nerve block injection. J Med Biomed Sci. 2010;1:52–56.
- Takasugi Y, Furuya H, Moriya K, Okamoto Y. Clinical evaluation of inferior alveolar nerve block by injection into the pterygomandibular space anterior to the mandibular foramen. Anesth Prog. 2000;47:125–129.
- Krall B. Local Anesthesia Manual: Loma Linda University School of Dentistry. Available at: https://bkanesthesia.com/pdfs/local_anesthesia_manual.pdf. Accessed January 4, 2023.
- Menke RA, Gowgiel JM. Short-needle block anesthesia at the mandibular foramen. J Am Dent Assoc. 1979;99:27–30.
- Galbreath JG, Eklund MK. Tracing the course of the mandibular block injection. Oral Surg Oral Med Oral Pathol. 1970;30:571–582.
- Gow-Gates GA. Mandibular conduction anesthesia: a new technique using extraoral landmarks. Oral Surg Oral Med Oral Pathol. 1973;36:321–328.
FIGURES 1, 2 AND 4: COURTESY LOCAL ANESTHESIA FOR DENTAL PROFESSIONALS; FIGURE 3 COURTESY KATHY BASSETT, RDH, MEd
From Decisions in Dentistry. February 2023;9(2)32-35.




