 Raycat / iStock / Getty Images Plus
Raycat / iStock / Getty Images Plus
Uncovering the Mystery
Ascertaining the exact etiology of endodontic-periodontal lesions is no easy feat.
Determining the precise etiology of an endodontic-periodontal lesion can be challenging because these lesions can present with similar signs and symptoms. Because successful treatment ultimately relies on an accurate diagnosis, it is critical that the primary etiology be identified before therapy is initiated.
The root canal system and periodontium are interconnected.1 The primary mode of communication between the root canal system and periodontium is through the apical foramina because these openings are the largest, and bacteria and/or their by-products can freely pass through them.

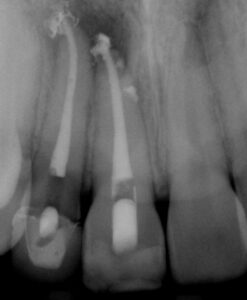
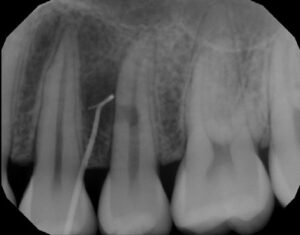
The smaller lateral and/or accessory canals can also act as a mode of communication between the root canal system and periodontium. Lateral and accessory canals are formed during tooth development due to a disturbance in the Hertwig’s epithelial root sheath and subsequent entrapment of blood vessels and connective tissue.2 The incidence of lateral canals varies with root location, with a lower frequency occurring coronally and a higher frequency occurring apically (Figure 1A and Figure 1B).3 Accessory canals can also occur in the furcation region of mandibular molars. One investigator injected ink into molars under pressure and found the presence of furcation canals in 28% of teeth examined; however, the incidence of accessory furcation canals may be as high as 76%.4,5


Dentinal tubules are another potential mode of communication between the root canal system and periodontium. These tubules are usually covered with cementum that acts as a physical barrier. However, the cementum can be physically removed during periodontal treatment; in addition, a congenital absence of cementum is also possible. When the cementoenamel junction (CEJ) was studied using a scanning electron microscope, 18% of teeth were found to have exposed dentinal tubules at the CEJ due to a congenital absence of cementum.6

When the dental pulp is vital, there is an outward flow of dentinal fluid, which contains immunoglobulins that can help prevent bacteria and/or their by-products from entering the root canal system.7 However, when the pulp becomes necrotic or the tooth has been previously treated, there is a lack of dentinal fluid, and this allows bacteria or their by-products to invade the root canal system more readily through the exposed dentinal tubules.
Vertical root fractures are yet another potential means of communication between the root canal system and periodontium. Clinical signs of a vertical root fracture include:
- A tooth that was previously treated endodontically
- J-shaped or “halo” radiolucency
- Deep, isolated periodontal pocket
- Coronally located sinus tract
The presence of two sinus tracts on both the buccal and lingual aspects are considered pathognomonic for a vertical root fracture.8 Although cone-beam computed tomography has a low specificity for visualization of such fractures, there are common features that can be observed from cone beam imaging.9 These include:
- Loss of bone in the mid-root area, with intact bone coronal and apical to the defect
- Absence of the entire buccal plate of bone
- Radiolucency at the terminus of a post
- Space between the buccal and/or lingual plate of the bone and the root surface
- Visualization of the vertical root fracture10

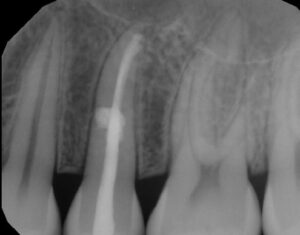
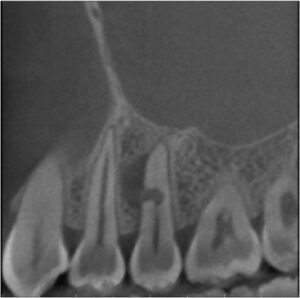
Developmental malformations, such as vertical radicular grooves, can result in extensive periodontal attachment loss and bone destruction. As the groove becomes contaminated with bacteria and biofilm along its length, periodontal destruction continues until the periodontal pocket eventually reaches the apex of the tooth (Figure 2A through Figure 2D).1
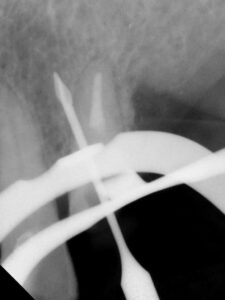
Other potential avenues of communication between the root canal system and periodontium include internal and external resorption (Figure 3A through Figure 3E), perforations (Figure 4), and horizontal root fractures (Figure 5).

References
- Rotstein I, Simon JH. The endo-perio lesion: a critical appraisal of the disease condition. Endod Topics. 2006;13:34–56.
- Kuroiwa M, Kodaka T, Abe M, Higashi S. Three-dimensional observations of accessory canals in mature and developing rat molar teeth. Acta Anat. 1992;143:130–138.
- DeDeus QD. Frequency, location, and direction of the lateral, secondary and accessory canals. J Endod. 1975;1:361–366.
- Gutmann JL. Prevalence, location, and patency of accessory canals in the furcation region of molars. J Periodontol. 1978;49:21–26.
- Burch JG, Hulen S. A study of the presence of accessory foramina and the topography of molar furcations. Oral Surg Oral Med Oral Pathol. 1974;38:451–455.
- Neuvald L, Consolaro A. Cementoenamel junction: Microscopic analysis and external cervical resorption. J Endod. 2000;26:503–508.
- Hahn CL, Overton B. The effects of immunoglobulins on the convective permeability of human dentine in vitro. Arch Oral Biol. 1997;42:835–843.
- Tamse A. Vertical root fractures in endodontically treated teeth: diagnostic signs and clinical management. Endod Topics. 2006;13:84–94.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, Arockiam S, Maheswari TNU, Natanasabapathy V. Diagnosis of vertical root fractures by come beam computed tomography in root filled teeth with confirmation by direct visualization: A systematic review and meta–analysis. J Endod. 2021;47:1198–1214.
- Fayad MI, Ashkenaz PJ, Johnson BR. Different representations of vertical root fractures detected by cone-beam volumetric tomography: A case series report. J Endod. 2012;38:1435–1442.
This information originally appeared in Dunlap CA, Lundergan WP, Dunlap BC. Diagnosis of endodontic-periodontal lesions. Decisions in Dentistry. 2023;9(2):42-45.


