Improve Outcomes by Digitizing Implant Workflows
Understanding the benefits and drawbacks of digitized workflows will improve the accuracy and efficacy of guided implant surgery, thereby minimizing complications.
Digitized workflows have revolutionized the practice of implant dentistry. Surgical guides may offer predictable solutions for implants that were previously aborted due to local, patient and/or esthetic risk factors. Guided surgery improves communication among the surgeon, dentist and technician, and provides a roadmap with the final prosthesis in mind. Several static guide designs are available today, including tooth-, mucosal- and bone-borne. Clinicians can also opt for specially supported guides. In addition, dynamic navigation uses novel technology to provide robotic guidance and real-time feedback during implant surgery.
Despite the obvious benefits of an expedited workflow, surgeons must first be proficient in freehand implant placement. Complications can arise intraoperatively, wherein guides may not fully seat, break or worse, leading to improper placement from malpositioned drill sleeves. This could result from imaging, planning or printing errors.
Consequently, surgical guides will never replace the knowledge of proper hard and soft tissue management, especially in complex implant cases. Understanding the benefits and current drawbacks of digitized workflows will improve the accuracy and efficacy of guided implant surgery and minimize potential complications along the way.

BASICS OF GUIDED IMPLANT SURGERY
Guided implant surgery fosters interdisciplinary collaboration. It reduces surgical and restorative mishaps because the dental team is aligned at each step of the process. Digital planning takes full advantage of the existing ridge dimensions for placement of larger-diameter and longer implants where anatomical limitations exist. Difficult site development and reconstructive surgeries may be avoided, saving the patient additional surgery, time and cost.1 Clinical outcomes are notably improved with digitized workflows, especially in cases involving multiple implants.2 Patients can also visualize the treatment plan on a computer and anticipate any challenges prior to surgery.
Compared to conventional implant placement, a recent randomized controlled clinical trial has shown guided implant surgery to result in greater accuracy, with shortened episodes of postoperative pain and swelling. No significant differences in clinical parameters were observed.3 Accuracy is measured by any deviation at the entry, apex, angle, and final depth points of implant placement. Errors can still occur because guided technology is dependent on multiple steps. In general, measurement errors of less than 0.5 mm have been reported from cone beam computed tomography (CBCT).4 It can also be difficult to interpret these scans; an example would be discerning artifacts from metal restorations.
Patient movement should therefore be minimized during scanning. A bite index is helpful in fully edentulous patients. The resulting digital imaging and communication in medicine (DICOM) file is then read by special planning software. A study that compared multiple, mainstream software packages found no statistically significant differences in implant accuracy.5
Next, a virtual rendering is captured intraorally with a digital impression, or extraorally on a cast. These data are used to generate a stereolithography (.STL) file. The .STL and DICOM files are merged and aligned on an implant planning software to generate a printable guide. Many problems can occur at this stage, especially in inexperienced hands, due to errors in conversion, segmentation, alignment and planning.6 The guide is fabricated through computer-assisted or photo-polymerization techniques. There are no clinically significant differences between thermo-formed and three-dimensionally (3D) printed guides,7 although the latter approach is more accessible, easier to use, and less expensive.

Once the guide is transferred to the surgical field, operator technique and experience dictate final implant positioning. Flapless implant placement should be approached with caution because deviations still occur, even among the most skilled operators.8 Experience does count, however, as research demonstrates that compared to those who have placed more than 500 implants, less seasoned surgeons experience significantly greater positioning errors, even with use of a single guide and multiple fixation screws.9 Still, clinicians should not become reliant on guides, but instead use them to facilitate treatment in more challenging scenarios.

Another consideration is that while digital workflows bring many advantages in dental implant therapy, clinicians looking to step into the digital arena should anticipate significant upfront costs for the necessary software and hardware.10
STATIC SURGICAL GUIDES
Tooth-borne guides rely on the support, stability and retention of teeth and regional anatomy. These are used for single or multiple implants in cases involving implant-supported crowns and bridges. Challenges can arise at posterior sites for patients with limited opening, as guided drill bits are larger for these sites.11 Shorter drill bits can instead be used with the guide for initial osteotomy preparation, then drilled to depth without it. An open sleeve with a buccal or lingual slot helps with drill access in tight interarch spaces.
Mucosal-borne guides depend on soft tissue landmarks only. Unlike their tooth-borne counterparts, they often lack retention due to differences in the amount and thickness of available tissue. In fact, greater mucosal thickness increases implant deviation.12 This can be overcome with specially supported guide designs that use mini-screws and pins with a bite index.13 Partially dentate patients may experience significantly greater implant accuracy because they benefit from the support and stability of the surrounding teeth and tissues during site preparation.14

Bone-borne guides are typically reserved for full-arch cases during or after extractions in the edentulous patient. They are supported by natural bony divergences in load-bearing areas; however, given the extent of flap reflection required, they may be difficult to fabricate and seat. Compared to mucosa-supported guides, a prospective study showed greater movement during site preparation, increasing the number of adjustments and checks needed.15 Furthermore, a recent systematic review and meta-analysis found that bone-supported guides had significant deviations in the angle, entry and apex points.11
To overcome these challenges, stackable guides provide an immobile foundation with pins or screws fixed to the bone. Other guides are then sequentially stacked to aid in bony reduction, and implant positioning and placement. When implants are planned in a terminal dentition, it is helpful, when possible, to use a tooth-borne guide. Extractions are staged, so osteotomy preparation can be made to depth, with alveoloplasty performed thereafter. This reduces surgical time and improves implant accuracy.
DYNAMIC NAVIGATION
When this technology was first introduced, bulky equipment, high costs, and complicated chairside instrumentation made dynamic navigation undesirable. It had long been used in some medical specialties — from ophthalmology to surgical oncology — because, unlike static templates, it can adjust to real-time changes and surgical findings. Clinicians also refer to a computer screen, improving ergonomics over time.16
Dynamic navigation requires a CBCT with a fixed fiducial marker, virtual implant planning, and calibration and registration of markers and implants drills, with an attached tracking array for implant placement.16 These systems rely on optical motion tracking, either by infrared light or reflected infrared light from a source back to a camera. The latter is a passive process more commonly used today. A light is projected onto the proposed implant site, while light is reflected off tracking arrays attached to the patient and handpiece, which allows tracking to determine the proper position according to the initial plan.17

In the dentate patient, the thermoplastic portion of the fiducial clip is supported by at least three teeth. A CBCT is taken with this in place, using a tracker arm attachment on the buccal aspect. It will be replaced during surgery on the same arch to provide guidance without interference. This is more challenging in the edentulous patient, where at least four 4 mm screws need to be placed to facilitate 3D imaging and stabilization. The U.S. Food and Drug Administration currently requires these added steps, but fiducial-free systems are being researched.16 In either scenario, instruments are frequently calibrated. The assembled parts, handpieces, and patient tracking array are placed in front of cameras to “learn” their shape. Special trackers and probes are used in edentulous cases. Calibration accuracy is verified when the drill bit is within 200 micrometers of the fiducial markers and clip.16
A recent systematic review determined the average global platform, apex and angulation deviations were clinically acceptable, with no significant differences between model studies and clinical trials in regression analysis.18 Another prospective study found that angular deviation was the most important improved parameter in dynamic navigation. Any changes from the initial to surgical visit can affect seating of the fiducial clip and tracking.19 There are learning curves associated with both static and dynamic navigation technology.

CASE REPORT
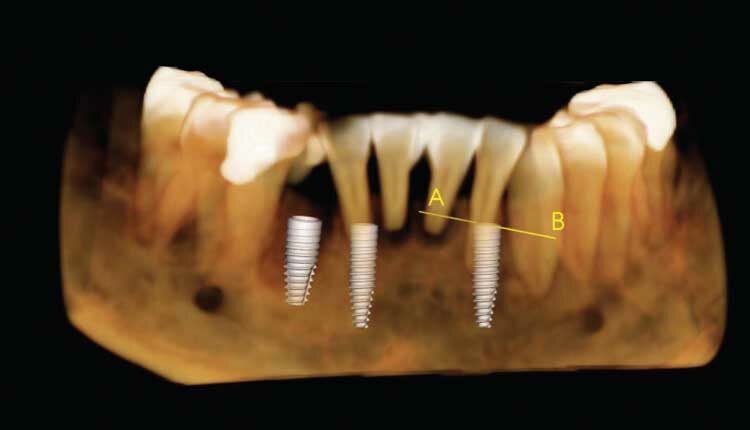
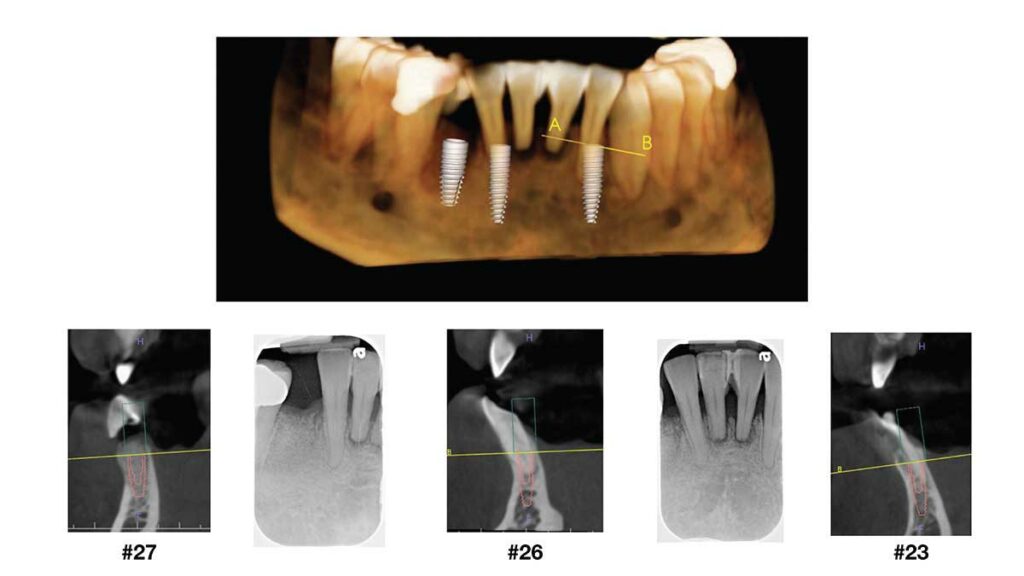
The following case illustrates the use of a digitized workflow for immediate implant placement in the lower anterior mandible. A 54-year-old female presented to the graduate periodontics clinic at the University of Texas Health Science Center at San Antonio School of Dentistry interested in implant therapy (Figure 1 through Figure 16). She had a 7.5-pack-year cigarette smoking history, with no other medical issues. Tobacco cessation was encouraged as part of treatment.
The patient first presented with localized areas of periodontitis around her second molars. This was stabilized with osseous resective surgery and periodontal regeneration, where indicated. After a thorough patient evaluation and review of different techniques and materials, a comprehensive treatment plan was developed, and consents were obtained. Surgical procedures were performed using IV conscious sedation. The treatment plan included:
- Cone-beam imaging, an intraoral scan, and digital wax-up to fabricate a surgical guide
- Extractions of teeth #23 through 26, with immediate implant placement at sites #23, 26 and 27, with contour bone augmentation using a printed surgical guide
- Second-stage implant surgery to uncover implants for fabrication of an implant-supported bridge at sites #23 through 26, and a single implant crown at site #27
One year after periodontal surgery was completed (with regular recall), the patient presented with clinically pink and healthy tissues, with probing depths less than 4 mm. Her oral hygiene compliance was still fair, with moderate deposits of plaque and calculus present throughout. Her chief concern was the hopeless, and now severely mobile, teeth #23 through 26. She worked at a busy law firm in a client-facing role, so her esthetic demand was high, and she had limited time available for treatment. The use of a tooth-supported guide minimized surgical needs, time and cost, as she could forego major site development surgery to increase the native ridge dimensions of the anterior mandible.

An intraoral scan was merged and aligned with the CBCT to design a surgical guide with the end prostheses in mind. An in-house 3D printer was used to fabricate the guide, and a surgical report was used throughout surgery to ensure proper implant positioning and placement. Caution was still taken to ensure complete visualization and careful management of the operative field to prevent surgical complications.
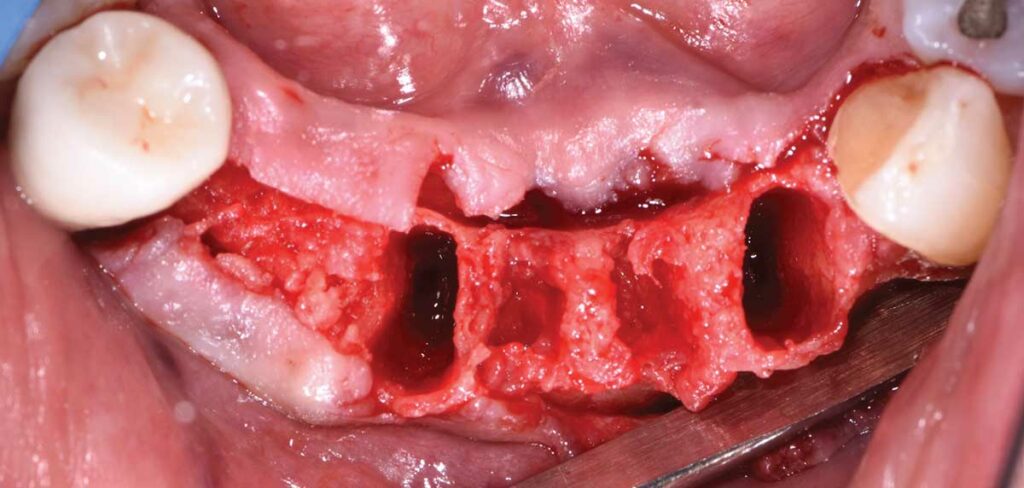
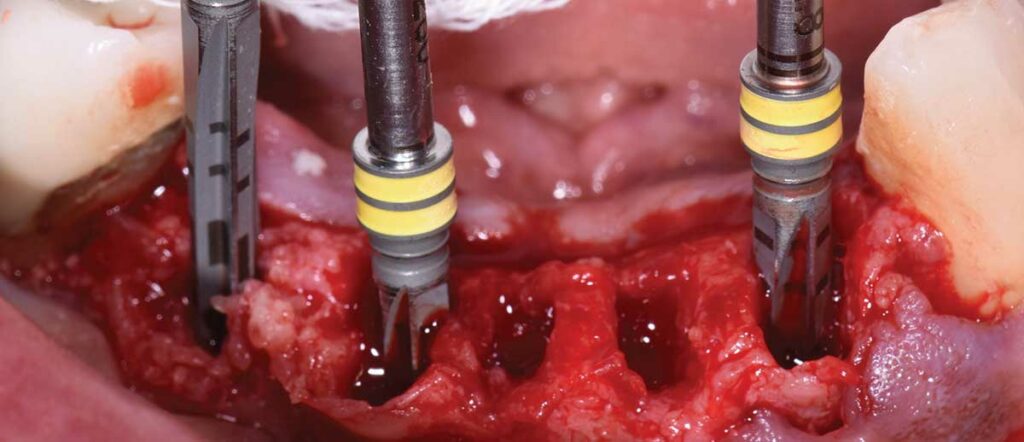
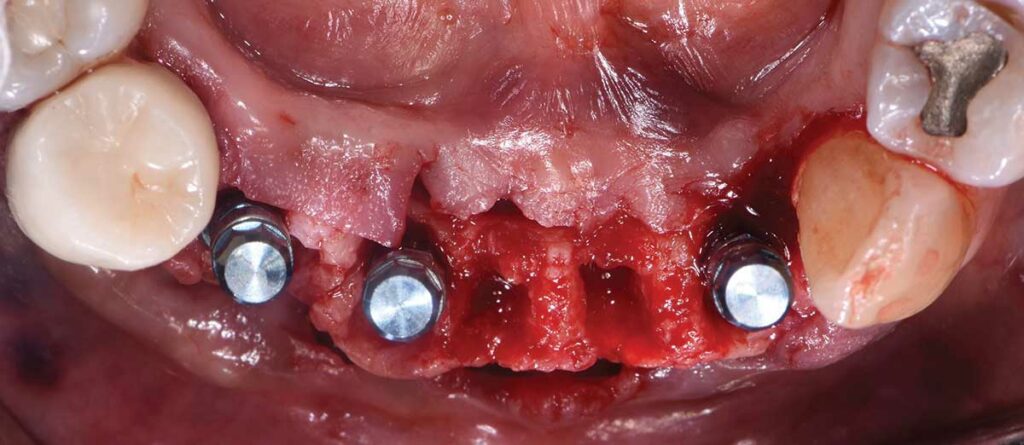
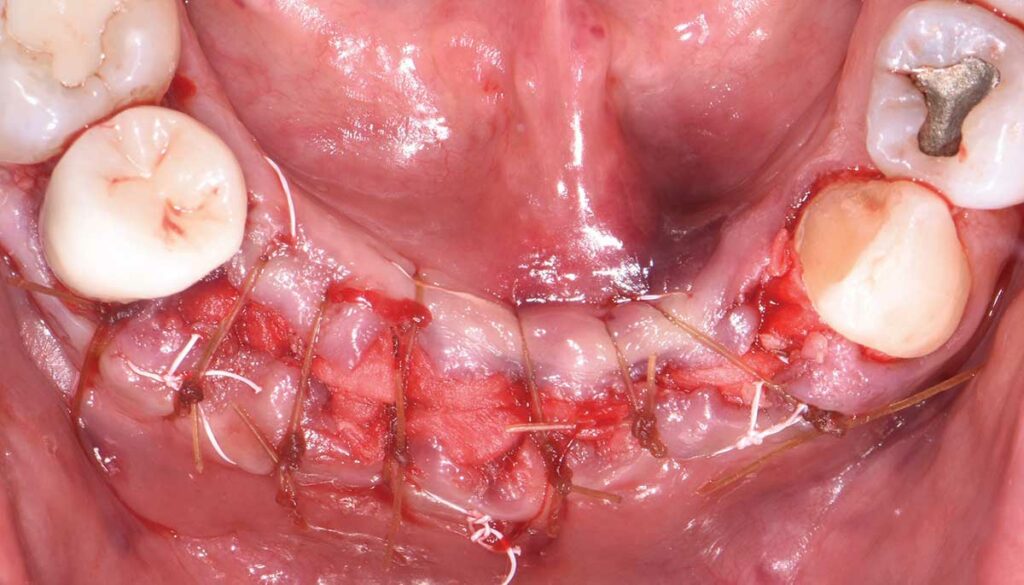
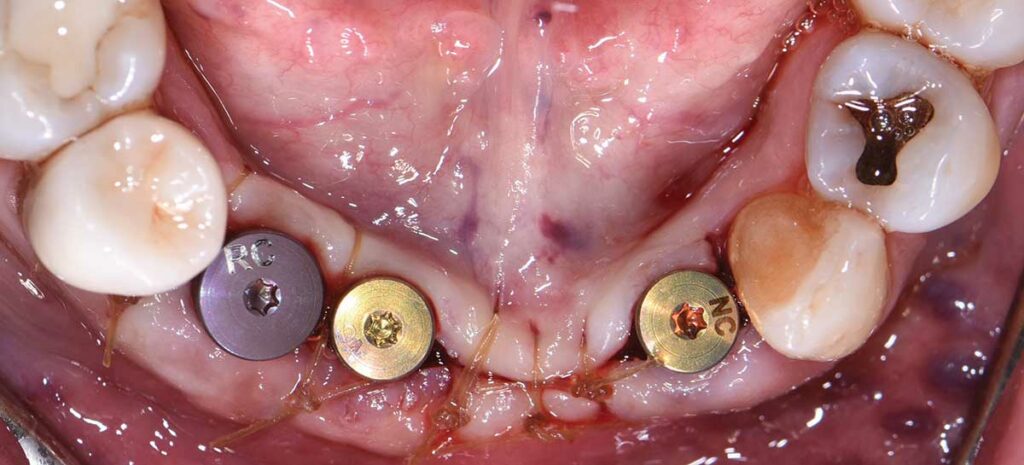
Buccal and lingual sulcular flaps were prepared from teeth #22 to 28, and a full thickness flap was reflected. Teeth #23 through 26 were extracted in minimally traumatic fashion. A printed surgical guide with 2.8 mm drill sleeves was used for implant positioning. Two bone-level, 3.3-mm-wide and 12-mm-long implants were placed at sites #23 and #26, and one bone-level, 4.1-mm-wide and 10-mm-long implant was placed at site #27, per the manufacturer’s recommendations, and primary stability was achieved. Mineralized freeze-dried bone allograft was prepared and placed within the implant-socket gaps and 1 to 2 mm beyond the arch form. Resorbable, collagen membranes were layered over the augmented sites. Flaps were repositioned and secured using a combination of non-resorbable mattress sutures and resorbable simple interrupted sutures. This ensured graft stability and minimized discomfort during suture removal.
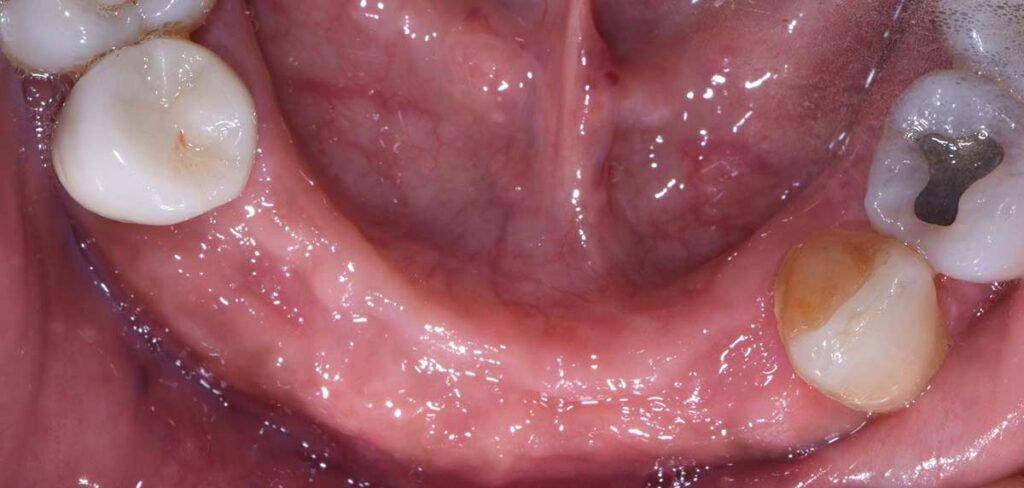
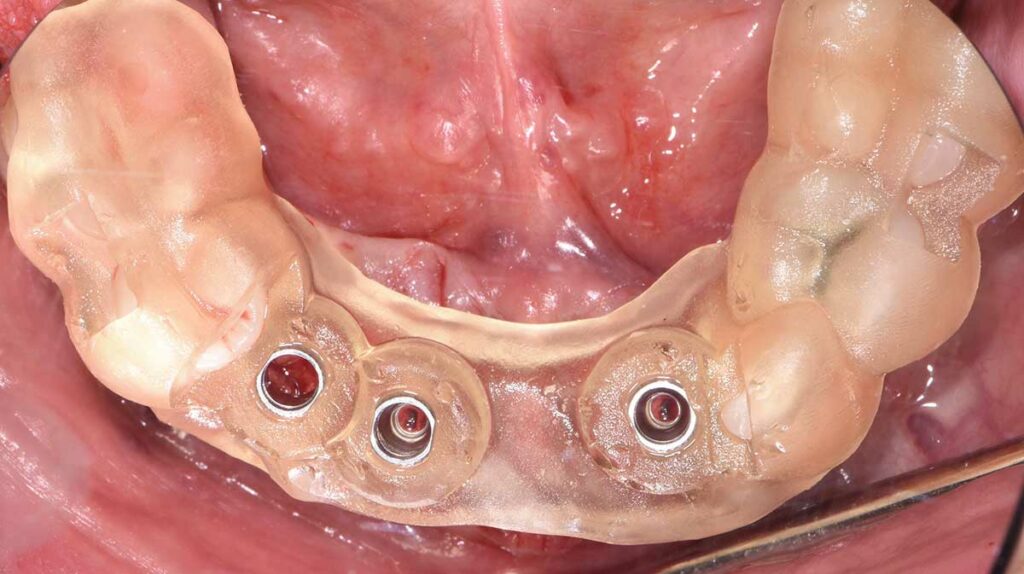
Postoperative instructions were reviewed. The patient was strongly advised to avoid wearing her lower Essix retainer during initial healing to minimize the risk of implant failure. She returned for follow-up at two weeks and eight weeks, and she had composite buccal restorations placed from teeth #7 to 10 for esthetics during this time. Implants were uncovered after three months. The tissues surrounding the implants were healthy, pink and firm, with no signs or symptoms of peri-implant disease. Healing abutments were attached. The patient returned to the clinic for fabrication of her final prostheses and will be seen for yearly recalls.

SUMMARY
The judicious use of static guides and dynamic navigation will continue to overcome challenges in implant dentistry; however, these technologies will never replace a foundational understanding of hard and soft tissue management. Guided surgery improves collaboration among the dental team, often reducing chairtime, surgical needs and cost for the patient. Ultimately, mastering digitized workflows can improve the implant experience and minimize any surgical or prosthetic misadventures.
Key Takeaways
- Digitized workflows are becoming routine in implant dentistry; they help expedite therapy and support successful long-term outcomes.
- The use of surgical guides offers a predictable solution, as guided surgery improves communication among the surgeon, dentist and technician, and provides a roadmap with the final prosthesis in mind
- Another approach is dynamic navigation, which uses novel technology to provide robotic guidance and real-time feedback during implant surgery.
- These modalities reduce surgical and restorative mishaps because the dental team is aligned at each step of the process.
- Despite the benefits of a digital approach, surgical guides and dynamic navigation will never replace the knowledge of proper hard and soft tissue management — especially in complex implant cases.
REFERENCES
- Fortin T, Isidori M, Bouchet H. Placement of posterior maxillary implants in partially edentulous patients with severe bone deficiency using CAD/CAM guidance to avoid sinus grafting: a clinical report of procedure. Int J Oral Maxillofac Implants. 2009;24:96–102.
- Youk SY, Lee JH, Park JM, et al. A survey of the satisfaction of patients who have undergone implant surgery with and without employing a computer–guided implant plate. J Adv Prosthodont. 2014;6:395–405.
- Vercruyssen M, Coucke W, Naert I, Jacobs R, Teughels W, Quirynen M. Depth and lateral deviations in guided implant surgery: an RCT comparing guided surgery with mental navigation or the use of a pilot‐drill template. Clin Oral Implants Res. 2015;26:1315–1320.
- Reddy MS, Mayfield‐Donahoo T, Vanderven FJ, Jeffcoat MK. A comparison of the diagnostic advantages of panoramic radiography and computed tomography scanning for placement of root form dental implants. Clin Oral Implants Res. 1994;5:229–238.
- Ruppin J, Popovic A, Strauss M, Spuntrup E, Steiner A, Stoll C. Evaluation of the accuracy of three different computer aided surgery systems in dental implantology: optical tracking vs. stereolithographic splint systems. Clin Oral Implants Res. 2008;19:709–716.
- Flügge T, Derksen W, te Poel J, Hassan B, Nelson K, Wismeijer D. Registration of cone beam computed tomography data and intraoral surface scans — a prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin Oral Implants Res. 2017;28:1113–1118.
- Matta RE, Bergauer B, Adler W, Wichmann M, Nickenig HJ. The impact of the fabrication method on the three‐dimensional accuracy of an implant surgery template. J Craniomaxillofac Surg. 2017;45:804–808.
- Van de Velde T, Glor F, De Bruyn H. A model study on flapless implant placement by clinicians with a different experience level in implant surgery. Clin Oral Implants Res. 2008;19:66–72.
- Cassetta M, Bellardini M. How much does experience in guided implant surgery play a role in accuracy? A randomized controlled pilot study. Int J Oral Maxillofac Surg. 2017;46:922–930.
- Orentlicher G, Horowitz A, Abboud M. What’s hindering dentistry from the widespread adoption of CT‐guided surgery? Compend Contin Educ Dent. 2015;36:762–764, 766.
- Raico Gallardo YN, da Silva-Olivio IR, Mukai E, Morimoto S, Sesma N, Cordaro L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28:602–612.
- Vasak C, Watzak G, Gahleitner A, Strbac G, Schemper M, Zechner W. Computed tomography‐based evaluation of template (NobelGuide)‐guided implant positions: a prospective radiological study. Clin Oral Implants Res. 2011;22:1157–1163.
- Cassetta M, Di Mambro A, Giansanti M, Stefanelli LV, Barbato E. How does an error in positioning the template affect the accuracy of implants inserted using a single fixed mucosa‐supported stereolithographic surgical guide? Int J Oral Maxillofacl Surg. 2014;43:85–92.
- Pettersson A, Komiyama A, Hultin M, Nasstrom K, Klinge B. Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin Implant Dent Relat Res. 2012;14:527–537.
- Arisan V, Karabuda CZ, Ozdemir T. Implant surgery using bone‐ and mucosa‐supported stereolithographic guides in totally edentulous jaws: surgical and post‐operative outcomes of computer‐aided vs. standard techniques. Clin Oral Implants Res. 2010;21:980–988.
- Panchal N, Mahmood L, Retana A, Emery R 3rd. Dynamic navigation for dental implant surgery. Oral Maxillofac Surg Clin North Am. 2019;31:539–547.
- Strong EB, Rafii A, Holhweg-Majert B, Fuller SC, Metzger MC. Comparison of 3 optical navigation systems for computer-aided maxillofacial surgery. Arch Otolaryngol Head Neck Surg. 2008;134:1080–1084.
- Wei SM, Zhu Y, Wei JX, Zhang CN, Shi JY, Lai HC. Accuracy of dynamic navigation in implant surgery: A systematic review and meta-analysis. Clin Oral Implants Res. 2021;32:383–393.
- Block MS, Emery RW, Cullum DR, Sheikh A. Implant placement is more accurate using dynamic navigation. J Oral Maxillofac Surg. 2017;75:1377–1386.
From Decisions in Dentistry. May 2022;8(5)16-18, 20, 22.


