 BRIAN / ISTOCK / GETTY IMAGES PLUS
BRIAN / ISTOCK / GETTY IMAGES PLUS
Adolescent Opioid Exposure in Dentistry
Clinicians should consider nonopioid analgesics when managing adolescent postoperative pain — especially given these patients’ risk for inappropriate substance use.
This course was published in the May 2022 issue and expires May 2025. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the impacts of prescribing opioids to adolescents and young adults when managing postoperative dental pain.
- Explain trends in dentists’ opioid prescribing patterns, the reasons behind these changes, and typical procedures that might result in opioid scripts.
- Discuss effective strategies for managing postprocedural discomfort — including use of opioid alternatives — in this patient population.
Dentists often play a significant role in prescribing opioids to adolescent patients, especially when removing third molars. While these analgesics remain an important tool in the postoperative armamentarium, their use can usually be avoided. Utilizing alternate pain management strategies is particularly important when treating adolescents, as this patient demographic is more susceptible to substance use disorder as the prefrontal cortex develops and matures. With the goal of minimizing unwanted and unnecessary exposure to opioids, this article will explore safe and effective options in managing postoperative discomfort in young patients.
NEUROBIOLOGICAL IMPLICATIONS
Neurobiological and behavioral changes occur during adolescent opioid use, and these may be compounded if used in combination with nicotine, alcohol, cannabis and/or other drugs. The resulting behavioral changes may manifest as novelty seeking, impulsivity and/or reward performance. These may include increased risk for developing cognitive defects, psychopathology, or later substance use disorders that result in structural and functional changes in the brain.1 The rate of substance use increases among adolescents ages 12 to 18 and is associated with abnormalities in brain function and neurocognition over time. Such changes include brain structure volume, white matter quality, and cognitive task abnormalities. Alcohol and substance use is significant among the U.S. adolescent population; 73% of youth have used alcohol and 48% have used illicit drugs by their senior year in high school.2 In 2006, 23% of youth met the diagnostic criteria for a substance use disorder (alcohol or drug abuse/dependence) by age 20.3 This represents approximately one in five adolescent Americans (or 74 million young people).4,5
The adolescent period is often associated with the struggle between increased rates of substance use versus ongoing neuromaturation of the brain. This results in spatial, inhibitory, learning, memory functioning, and performance deficits.6 Evidence shows that while adolescent brain development from childhood may be more resilient to the neurotoxic effects from alcohol and drugs, there may be cognitive discrepancies resulting in subsequent educational, occupational, and social functioning deficits from substance use or abuse.7–10
It has been suggested that normal adolescent brain development, including synaptic refinement and myelination, is crucial for the prefrontal and temporal cortices to form. This increased myelination is critical for smoother, more efficient communication between the frontal-subcortical brain regions, resulting in better cognitive control and decision-making.11 However, adolescent substance use has been associated with transformations in the prefrontal regions and limbic system that may contribute to increased risk-taking and novelty/sensation-seeking behaviors.12,13 These neurochemical and neuromaturation changes have been hypothesized to contribute to adolescents’ increased tendency for alcohol and drug use.14 Such behaviors may have deleterious effects on adolescent neurocognitive functioning, including declines in memory,15 attention and information processing,16,17 as well as executive functioning.18–20 Specific deficits associated with executive functioning are poor future planning, difficulties in abstract reasoning, and an inability to formulate new solutions to problems.18
RESEARCH AND HISTORY
Dentistry has a history and reputation for prescribing opioids for pain. In the 1990s, dentists were the top prescribers of immediate-release opioids, issuing 15.5% of all opioid scripts written by healthcare providers. The number of immediate-release opioid prescriptions from dentists dropped to 8% in 2009, and by 2012 the rate across all healthcare specialties had fallen to 6.8%.21–23 One study of dental patients with private insurance found that opioid prescribing rates from 2010 to 2015 increased slightly, with the greatest rise seen in adolescents ages 11 to 18.24 Almost one-third of the opioid prescriptions written by dentists were related to nonsurgical visits. The remaining two-thirds were associated with surgical procedures.24
In today’s practice, dentists continue to make strides in reducing opioid scripts by recommending the use of nonopioid analgesics, such as ibuprofen or ibuprofen/acetaminophen combinations. As an additional cautionary mechanism, many states require providers to review the patient’s medication history, found in the prescription drug monitoring program, before prescribing an opioid24 — a strategy that is intended to help identify and mitigate potential abuse.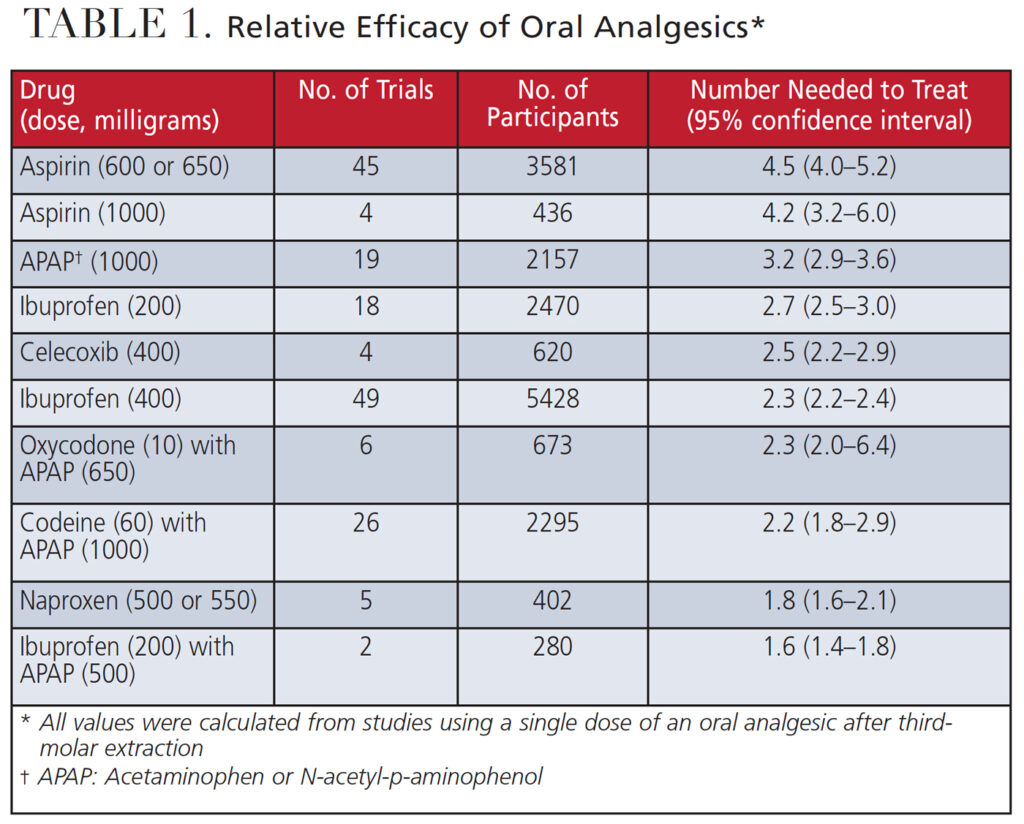
OPIOID USE IN ADOLESCENTS
The opioid epidemic continues to affect the U.S. population, with drug overdoses reaching new heights in 2021. An estimated 100,306 drug overdose deaths occurred during a 12-month period ending in April 2021. This represents an increase of 28.5% from the 78,056 deaths during the same period the year prior. Of those deaths, an estimated 75,673 opioid fatalities occurred in the 12-month period ending in April 2021.25,26 While there has been a decrease in prescribing from physicians by 44% from 2011 to 202027 and a 37.1% decrease from 2013 to 2019,28 dentists remain a significant source of prescription opioids. Oral surgery (extractions, for example), implant therapy, and root canal procedures have been associated with the highest rates of opioid prescribing.29
In 2009, dentists were the main prescribers of opioids, writing ~700,000 scripts (30.8% of all opioid prescriptions) for patients ages 10 to 19 years. This was followed by primary care physicians, who wrote 13.1% (~300,000) of all opioid prescriptions, and emergency medicine physicians, who issued 12.3% (~300,000) of opioids scripts for this age group.30 A 2016 study reported that 11.2% of dentist-prescribed opioids were written for patients younger than 21 years.31 When considering drug choices, it is important to remember that children younger than 12 should not be prescribed codeine or tramadol.32 Research suggests that adolescents’ nonmedical use of prescription opioids is a strong predictor of heroin use in adolescence and young adulthood, with peak heroin usage starting at ages 17 to 18, regardless of race, ethnicity or income group.33 Focusing on adolescents who use prescription opioids for nonmedical (i.e., recreational) purposes may have a positive effect on mitigating or preventing heroin use in adulthood.34,35
FAMILIAL CONSIDERATIONS
Before prescribing opioids to adolescents and young adults, clinicians should consider all risk factors — including long-term opioid use history among the patient’s family. Research reveals that opioid-naïve adolescents and young adults with a familial history of long-term opioid use may be at risk of substance abuse if exposed to postoperative opioids. It is incumbent that dentists compile a thorough family history of drug use and/or abuse in order to reduce the possibility of opioid dependency developing in opioid-naïve adolescents or young adults.36,37 There is also an association with future misuse if an adolescent is prescribed opioids before the 12th grade, even if the patient has little personal drug experience and disapproves of illegal drug use.38 This underscores the importance of patient education — as prevention is critical to mitigating future drug use.38
In fact, a 2021 study showed that a single, short, low-dose opioid prescription can have a profound impact on adolescents, and may be related to risks of persistent use of opioids.39 Another report indicated that more than 50% of all dental prescriptions remain unused three weeks after a surgical extraction. These unused prescriptions may lead to nonmedical use.40 Moreover, it has been reported that up to 1500 deaths annually are due to opioid prescriptions written by U.S. dentists.41 Thus, the dental community is encouraged to seriously reconsider prescribing opioid medications for postoperative analgesia.31,42,43
ADOLESCENT POSTOPERATIVE PHARMACOTHERAPEUTICS
Number needed to treat (NNT) is a measure that reflects an analgesic’s efficacy in providing 50% pain relief. Compared to controls in a clinical trial, this value reflects the number of patients who need to be treated for one of them to benefit from the drug. The best NNT is reflected when a patient takes 400 mg ibuprofen plus 1000 mg acetaminophen (NNT = 1.5) or 200 mg ibuprofen plus 500 mg acetaminophen (NNT = 1.6). (See Table 1 for NNTs of other medications.)
As part of efforts to reduce dental opioid prescriptions, it is helpful to know that adolescents typically respond well to nonopioid analgesics, such as ibuprofen or ibuprofen/acetaminophen combinations. With the understanding that lower NNT values signify more effective pain management, assuming no contraindications, a combination of ibuprofen and acetaminophen has the lowest NNT. Thus, this approach may be the best option for controlling postoperative pain resulting from dental procedures, including third molar extractions.44
For patients in whom severe pain persists after using the recommended ibuprofen/acetaminophen doses, it may be clinically appropriate to add an opioid. However, adding an opioid to an ibuprofen/acetaminophen combination for adolescents should be viewed as the exception, not a normal expectation.
SUMMARY
It is imperative for oral health professionals to understand the significant impact and potential danger of prescribing opioids as a first response to adolescent postoperative discomfort. Consequently, clinicians are encouraged to respond with appropriate measures when prescribing analgesics — and the efficacy of alternative pain management strategies is a major reason not to view opioids as a first choice for acute postoperative pain.
Considering the literature indicates that ibuprofen, with or without acetaminophen, provides pain relief equal or superior to that of opioid-containing medications,45 opioids can often be avoided altogether when managing acute pain in today’s practice.
REFERENCES
- Hamidullah S, Thorpe HHA, Frie JA, McCurdy RD, Khokhar JY. Adolescent substance use and the brain: Behavioral, cognitive and neuroimaging correlates. Available at: https://www.frontiersin.org/article/葖.3389/fnhum.2020.00298. Accessed April 12, 2022.
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national results on adolescent drug use: Overview of key findings, 2007. Available at: https://deepblue.lib.umich.edu/handle/떛.42/. Accessed April 12, 2022.
- Substance Abuse and Mental Health Services Administration. Results From the 2006 National Survey on Drug Use and Health: National Findings. Available at: https://files.eric.ed.gov/fulltext/ED498206.pdf. Accessed April 12, 2022.
- National Center for Education Statistics. Back to School Statistics. Available at: https://nces.ed.gov/fastfacts/display.asp?id=372. Accessed April 12, 2022.
- U.S. Census Bureau. Quick Facts United States. Available at: https://www.census.gov/quickfacts/fact/table/US/PST045219. Accessed April 12, 2022.
- Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci. 2009;40:31–38.
- Clark DB, Thatcher DL, Tapert SF. Alcohol, psychological dysregulation, and adolescent brain development. Alcohol Clin Exp Res. 2008;32:375–385.
- Crews F, He J, Hodge C. Adolescent cortical development: A critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86:189–199.
- Spear LP, Varlinskaya EI. Adolescence. Alcohol sensitivity, tolerance, and intake. Recent Dev Alcohol. 2005;17:143–159.
- Tapert SF, Granholm E, Leedy NG, Brown SA. Substance use and withdrawal: neuropsychological functioning over 8 years in youth. J Int Neuropsychol Soc. 2002;8:873–883.
- Luna B, Sweeney JA. The emergence of collaborative brain function: FMRI studies of the development of response inhibition. Ann NY Acad Sci. 2004;1021:296–309.
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–463.
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann NY Acad Sci. 2008;1124:111–126.
- Chambers RA, Potenza MN. Neurodevelopment, impulsivity, and adolescent gambling. J Gambl Stud. 2003;19:53–84.
- Brown SA, Tapert SF, Granholm E, Delis DC. Neurocognitive functioning of adolescents: effects of protracted alcohol use. Alcohol Clin Exp Res. 2000;24:164–171.
- Tapert SF, Brown SA. Substance dependence, family history of alcohol dependence and neuropsychological functioning in adolescence. Addiction. 2000;95:1043–1053.
- Tarter RE, Mezzich AC, Hsieh Y-C, Parks SM. Cognitive capacity in female adolescent substance abusers. Drug Alcohol Depen. 1995;39:15–21.
- Giancola PR, Mezzich AC, Tarter RE. Executive cognitive functioning, temperament, and antisocial behavior in conduct-disordered adolescent females. J Abnorm Psychol. 1998;107:629–641.
- Giancola PR, Shoal GD, Mezzich AC. Constructive thinking, executive functioning, antisocial behavior, and drug use involvement in adolescent females with a substance use disorder. Exp Clin Psychopharmacol. 2001;9:215–227.
- Moss HB, Kirisci L, Gordon HW, Tarter RE. A neuropsychologic profile of adolescent alcoholics. Alcohol Clin Exp Res. 1994;18:159–163.
- Rigoni GC. Drug utilization for immediate and modified release opioids in the U.S. Silver Spring, MD: Division of Surveillance, Research and Communication Support, Office of Drug Safety. U.S. Food and Drug Administration. 2003.
- Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SRB. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305:1299–1301.
- Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic-prescribing rates by specialty, US, 2007–2012. Am J Prev Med. 2015;49:409–413.
- Gupta N, Vujicic M, Blatz A. Opioid prescribing practices from 2010 through 2015 among dentists in the United States: What do claims data tell us? J Am Dent Assoc. 2018;149:237–245.e6.
- National Center for Health Statistics. Drug Overdose Deaths in the U.S. Top 100,000 Annually. Available at: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/떕/Ⴍ.htm/. Accessed April 12, 2022.
- National Center for Health Statistics. Provisional Drug Overdose Death Counts. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed April 12, 2022.
- American Medical Association. Report shows decreases in opioid prescribing, increase in overdoses. Available at: https://www.ama-assn.org/press-center/press-releases/report-shows-decreases-opioid-prescribing-increase-overdoses. Accessed April 12, 2022.
- American Medical Association. Opioid Task Force 2020 Progress Report. Physicians’ progress toward ending the nation’s drug overdose and death epidemic. Available at: https://www.ama-assn.org/system/files/떔-07/opioid-task-force progress-report.pdf. Accessed April 12, 2022.
- Steinmetz CN, Zheng C, Okunseri E, Szabo A, Okunseri C. Opioid analgesic prescribing practices of dental professionals in the United States. JDR Clin Trans Res. 2017;2:241–248.
- Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305:1299–1301.
- McCauley JL, Hyer JM, Ramakrishnan VR, et al. Dental opioid prescribing and multiple opioid prescriptions among dental patients: administrative data from the South Carolina prescription drug monitoring program. J Am Dent Assoc. 2016;147:537–544.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA restricts use of prescription codeine pain and cough medicines and tramadol pain medicines in children; recommends against use in breastfeeding women. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-restricts-use-prescription-codeine-pain-and-cough-medicines-and. Accessed April 12, 2022.
- Cerdá M, Santaella J, Marshall BDL, Kim JH, Martins SS. Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: a national study. J Pediatr. 2015;167:605–612.e1–2.
- Lankenau SE, Schrager SM, Silva K, et al. Misuse of prescription and illicit drugs among high-risk young adults in Los Angeles and New York. J Public Health Res. 2012;1:22–30.
- Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers — United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132:95–100.
- Harbaugh CM, Lee JS, Chua K-P, et al. Association between long-term opioid use in family members and persistent opioid use after surgery among adolescents and young adults. JAMA Surg. 2019;154:e185838.
- Schroeder AR, Dehghan M, Newman TB, Bentley JP, Park KT. Association of opioid prescriptions from dental clinicians for US adolescents and young adults with subsequent opioid use and abuse. JAMA Intern Med. 2019;179:145–152.
- Miech R, Johnston L, O’Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136:e1169–e1177.
- Wilson JD, Abebe KZ, Kraemer K, et al. Trajectories of opioid use following first opioid prescription in opioid-naive youths and young adults. JAMA Netw Open. 2021;4:e214552.
- Maughan BC, Hersh EV, Shofer FS, et al. Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug Alcohol Depend. 2016;168:328–334.
- Dionne RA, Gordon SM, Moore PA. Prescribing opioid analgesics for acute dental pain: time to change clinical practices in response to evidence and misperceptions. Compend Contin Educ Dent. 2016;37:372–378.
- Nadeau R, Hasstedt K, Sunstrum AB, Wagner C, Tu H. Addressing the opioid epidemic: impact of opioid prescribing protocol at the University of Minnesota School of Dentistry. Craniomaxillofac Trauma Reconstr. 2018;11:104–110.
- McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. J Adolesc Health. 2013;52:480–485.
- Moore PA, Hersh EV. Combining ibuprofen and acetaminophen for acute pain management after third-molar extractions: translating clinical research to dental practice. J Am Dent Assoc. 2013;144:898–908.
- Moore PA, Ziegler KM, Lipman RD, Aminoshariae A, Carrasco-Labra A, Mariotti A. Benefits and harms associated with analgesic medications used in the management of acute dental pain: An overview of systematic reviews. J Am Dent Assoc. 2018;149(4):256–265.e3. Erratum in: J Am Dent Assoc. 2018;149(6):413. Erratum in: J Am Dent Assoc. 2020;151(3):163.
From Decisions in Dentistry. May 2022;8(5)26-29.




