 ROBERTPRZYBYSZ/ISTOCK/GETTY IMAGES PLUS
ROBERTPRZYBYSZ/ISTOCK/GETTY IMAGES PLUS
Management of Malocclusion In Children and Adolescents
An exploration of the pediatric and general dentist’s role in early intervention in malocclusion involving issue with space management or posterior crossbite.
Part 1 of a two-part series: The first article in this two-part series on treating pediatric malocclusion explores space management and posterior crossbite correction. Appearing in a future issue, Part 2 will focus on managing skeletal problems in this patient population.
Having a strategy to manage an existing or developing dental anomaly or occlusal discrepancy is an integral part of comprehensive pediatric oral care. Children will not outgrow the majority of these issues, and the problems often become worse over time. In cases involving pediatric malocclusion, it is most effective to intervene in primary or early mixed dentition to reduce the severity of dental and occlusal problems and avoid future treatment complications.
Pediatric dentists and general dentists are usually the first to detect a child’s malocclusion. Some well-accepted benefits of early orthodontic treatment are that it can eliminate or reduce the severity of a developing malocclusion, and reduce the length and complexity of future orthodontic treatment. It also has the potential to correct problems in skeletal growth, and may reduce the need for extraction of permanent teeth during Phase II orthodontic treatment. In addition, correcting severely protruded upper anterior teeth can significantly reduce dental trauma. Perhaps most importantly, any of these interventions can promote a child’s self-esteem.
Early management includes preventive and interceptive orthodontic therapies. Early treatment can begin in primary dentition if there is functional deviation, and in early mixed dentition (when all incisors and permanent first molars have erupted) if there are crowding or skeletal problems. Clinicians can also delay treatment until the permanent dentition is in place.
The goal of treatment and the benefits of early versus late intervention must be clearly communicated to patients and parents/caregivers. The core goals of treatment are to intercept malocclusions before they become worse, and guide the outcome toward a positive result.
ORTHODONTIC PROBLEMS IN CHILDREN
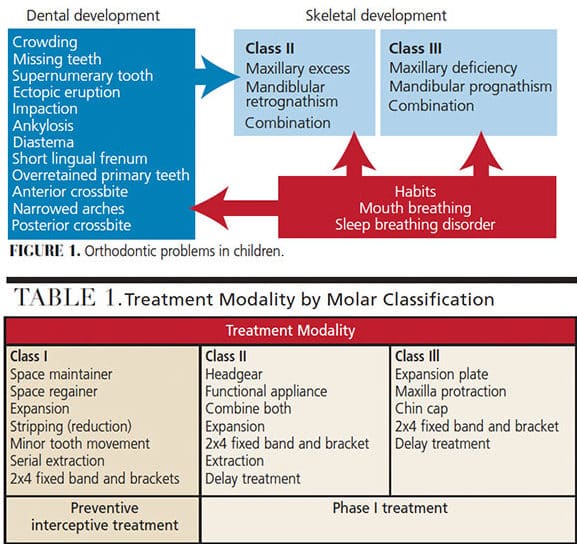
Orthodontic issues can start as early as the eruption of the first tooth. Most dentoalveolar and skeletal problems develop during the mixed dentition period. The soft tissues also play an important role in existing dental or skeletal problems (Figure 1). Treatment modalities can be easily explained in three malocclusion classes: Class I, Class II and Class III (Table 1).
The comprehensive management of early malocclusion in children and adolescents must take into account dental, skeletal and soft tissue problems, and their interrelationships. Successful early orthodontic treatment necessitates a comprehensive evaluation of craniofacial growth, occlusal and dental development, treatment mechanics, the patient’s behavior, and parental/caregiver expectations. Clinicians must develop a thorough diagnosis and definitive treatment plan with clearly set goals.
The treatment protocols can be divided into separate phases. The goal of the first phase (Phase I orthodontic treatment) is to intercept existing abnormalities, or reduce the severity of problems in primary and early mixed dentition. The next phase is a supervision phase after completion of Phase I treatment, with the goal of retaining the first phase results and monitoring occlusal and dental development. The second orthodontic treatment phase (Phase II orthodontics) or comprehensive treatment phase is to make detailed adjustments of the dentition, as needed.
SPACE MANAGEMENT IN PRIMARY DENTITION
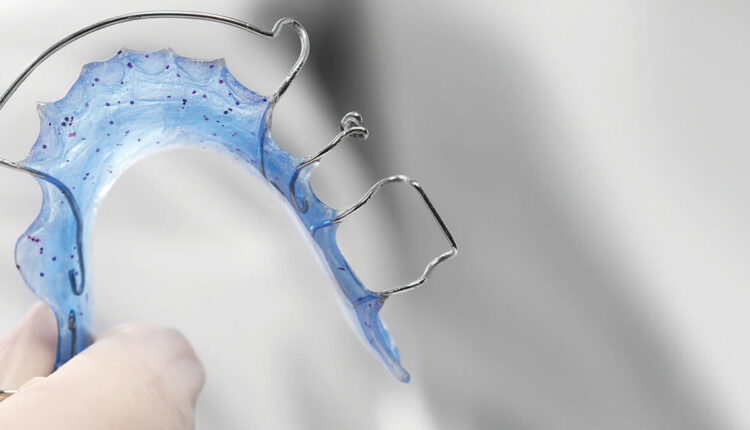
Often, primary incisors are lost due to caries or trauma. This leads to very little change in the primary arch length and does not require space maintenance. An upper lingual arch with teeth, such as the Groper’s appliance, is an option for esthetic concerns, but is not required for orthodontic space maintenance (Figure 2).
When the loss of a primary canine is caused by caries, a space maintainer is not required in this stage. The loss of a primary first molar alone usually does not require a space maintainer in primary dentition when the primary second molar is retained. The loss of primary second molars generally requires a space maintainer, especially when the permanent first molar is actively erupting.
COMMON PROBLEMS IN GROWING DENTITION
Crowding is the most common orthodontic issue for patients of all ages. It initiates with incisor liability — the size discrepancy between the primary incisors and permanent incisors. The sum of the maxillary four permanent incisors is, on average, 7.6 mm larger than the primary incisors, and the sum of the mandibular four permanent incisors is 6.0 mm larger than the primary incisors.1 Providers can compensate for this space discrepancy via interdental spacing in primary incisors, labial eruption of permanent incisors, distal movement of mandibular primary canines by lateral incisor forces, and increases in inter-canine width.
After mandibular lateral incisor eruption is complete at 8 to 9 years of age, there is no further arch length increase — though there is a decrease in the normative arch development. The normative arch length decrease is initiated by an early mesial shift, with eruption of the lower first permanent molars and loss of about 1 mm. The arch length is then increased by approximately 2 mm due to the labial eruption of permanent incisors. Next, there are two additional decreases in arch length due to late mesial shift closing the leeway space 2 to 3 mm per quadrant, and the uprighting of lower incisors as the mandible completes forward growth. The average arch length is decreased 2 to 3 mm per side, and arch perimeter decreases approximately 4 to 6 mm in total.2,3 The majority of children show 1 to 4 mm of lower incisor crowding during this stage.2
At this point, any crowding in the anterior region is an established problem and no self-improvement is anticipated through future growth. Additionally, any premature loss of primary posterior teeth (due to caries or other causes) will make space problems more complicated due to decreasing arch length.
SPACE MANAGEMENT IN MIXED DENTITION
The majority of crowding in the mixed dentition is a combination of tooth size discrepancy and arch length deficiency, and is exacerbated by premature loss of primary teeth due to caries. The management of space issues requires consideration of early correction of incisor crowding, and preservation of leeway space. The early preservation a leeway space can alleviate 72% of crowding cases.4 The well-planned, early use of leeway space can assist in the normal eruption of permanent canines and premolars. The following space management modality is based on visible incisor crowding in mixed dentition.
1. Incisor crowding less than 4 mm, with no premature loss of primary teeth
Interproximal reduction (IPR) of a primary canine:
Indication: Lower lateral incisor is lingually erupting at 7 to 8 years of age; lower primary canine’s root is intact, and no resorption has occurred from the lateral incisor. Use a No. 699 or No. 168 bur to apply IPR at the mesiolingual corner of primary canine down to the gingival contact. This will enable the force of the tongue to push the incisor forward to relieve crowding.5
Preserving E-space and guidance eruption of a lower permanent canine and first premolar:
This can be achieved by placing a passive lower lingual holding appliance (LLHA) and monitoring canine and first premolar eruption distally to minimize malposition of canine labial to lateral incisor by either extracting the primary first molar or IPR mesial of the primary second molar by early use of E-space.
2. Incisor crowding more than 4 mm and arch length deficiency
This usually occurs when there has been premature loss of one or more primary teeth. According to Owen,6 96% of space is closed within 12 months following the premature loss of a primary tooth. The highest and earliest space closure is loss of upper primary second molar due to the permanent first molar mesialization. The rate of space closure in maxillary teeth is faster than in mandibular teeth, and is greatest in the first six months after loss, before slowing and ceasing at 12 months. The space closure in the maxilla is caused by mesial movement of teeth posterior to the extraction space. In the mandibular space, closure is caused by distal movement of teeth anterior to the space. Factors that can increase the rate of space closure include crowded mandibular incisors, deep bite, young age, and abnormal oral habits.
PREMATURE LOSS OF A PRIMARY CANINE
The most common space loss in mixed dentition is premature loss of either one or both lower primary canines. This can create a series of problems; for example, the incisors could tip lingually and distally, which causes a mandibular dental midline shift; an anterior overjet could increase and deepen the anterior overbite; the permanent canines could erupt ectopically or become impacted; and both arch length and perimeter could be reduced. Almost all articles and textbooks instruct clinicians to extract the contra-lateral primary canine if one is lost prematurely. The goal of this extraction is to maintain symmetry of the lower midline by allowing mandibular anteriors to make a distal shift bilaterally.7–10 This strategy will require future extraction of permanent premolars in a lateral orthodontic treatment of a bilateral loss of primary canines.
Appropriate treatment approaches
1. If there is early loss of a primary canine without space loss:
a. Place a lower lingual arch with a soldered spur to prevent the incisors from shifting (Figure 3).
2. If there is space loss and space is available to regain:
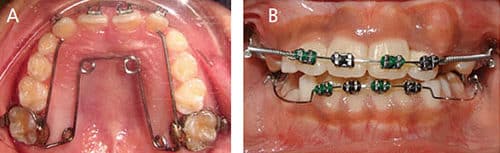
a. Plan for Phase I orthodontic treatment involving expansion, a 2×4 edgewise appliance, and placement of an LLHA to retain. The goal is to decompensate for the displacement of the lower incisors and regain space for the lower permanent canine (Figures 4A and 4B).
3. If incisor crowding is more than 6 mm, the dental midline is significantly skewed, and the permanent incisor is blocked from the arch:
a. Extract the contra-lateral primary canine. Obtain an orthodontic evaluation for non-extraction or serial extraction orthodontic treatment, as needed.
Premature loss of a primary first molar
In these presentations, there will be no significant mesial movement of the lower permanent molar, although there is some potential for space loss in the maxilla when the permanent first molar has not yet erupted. A space maintainer is recommended if the primary first molar is lost before or during the eruption of the permanent first molar.11
Premature loss of a primary second molar
Without space loss:
1. When the permanent first molar has erupted and the primary second molar has been lost:
a. A space maintainer is required.
b. Treatment options include using a band and loop, Nance appliance, transpalatal arch, or a lower lingual holding arch.
2. When the permanent first molar has not yet erupted and the primary second molar has been lost:
a. A distal shoe space maintainer should be placed.
With space loss:
1. There is no easy solution when the primary second molar is lost and space loss has occurred. Treatment depends on the severity of the space loss, along with additional dental and skeletal considerations.
a. Treatment options range from a simple, local space-regaining appliance
to lengthy Phase I treatment.
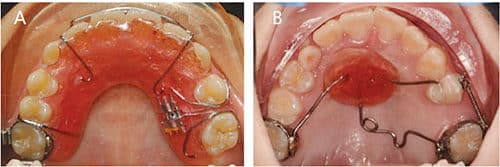
b. Appliance options include a molar distalizer with a Nance as an anchorage, pendulum appliance, distal jet appliance, partial 2×4 brackets with open coil spring, or removable space regainers (Figures 5A and 5B).
Posterior crossbite in primary and mixed dentition
Posterior crossbite is one of the common problems in mixed dentition. The crossbite can be unilateral or bilateral, a single tooth or a group of posterior teeth, dental or skeletal, or a combination of these. Prevalence is 5% to 8% in U.S. studies and 4% to 23% in European studies.12,13 Crossbite etiology can include hereditary factors, congenital anomalies, constriction of the maxilla, mouth breathing, nonnutritive sucking habits, localized tooth interference, atypical eruption problems and trauma.
Unilateral posterior crossbite
In primary dentition, 90% of crossbites involve the primary canine and first and second primary molars. The primary lateral incisor is also involved in 60% of cases. Posterior crossbites present with constricted maxilla, reduced inter-canine width, and functional shift at closure, with the chin shifting to the crossbite side. With this shift, the condyle rotates on its axis and translates downward and forward on the non-crossbite side. Therefore, the crossbite side appears as a Class II occlusion or distal step, while the non-crossbite side appears as a Class I/III occlusion or mesial step (Figures 6A through 6C). If left untreated, this functional shift will result in asymmetric jaw growth and the potential for temporomandibular joint disorders.14–16

Bilateral posterior crossbite
Bilateral posterior crossbites are usually skeletal in origin. Arising from a constricted maxilla, in most cases bilateral posterior crossbites have no functional shift and no midline discrepancy. They are often associated with mouth breathing, anterior open bite or dolichocephalic growth.
It is important to accurately diagnose a unilateral posterior or bilateral posterior crossbite with functional shift before initiating treatment. The first step is to check the centric relation (CR) and centric occlusion (CO). A true unilateral posterior crossbite does not shift from CR to CO. The second step is to examine the symmetry of the maxillary arch. A true posterior crossbite presents with asymmetry of the arch, with narrowing on the crossbite side.
Crossbite treatment approaches
Early intervention in posterior crossbites is simple, effective and stable. The best age to intervene is in late primary dentition or early mixed dentition. Up to 45% of posterior crossbites in primary dentition are self-correcting upon development of the permanent dentition.17
Common treatment modalities for posterior crossbite include:
- Eliminating any patient habits associated with the posterior crossbite.
- Removing tooth interference that causes a CR/CO shift; this can correct unilateral crossbite partially or completely in primary dentition.
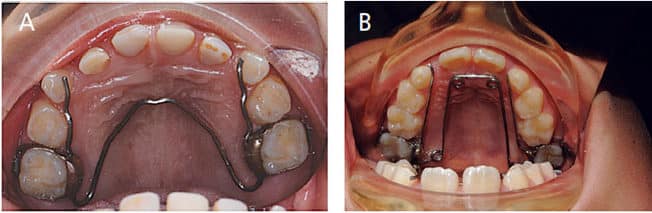
- Assisting in maxillary and/or mandibular expansion using various appliances, such as the quad-helix, W-arch and others (Figures 7A and 7B).
Retention and relapse
Any expansion of the maxilla will also require over-correction and retention. Both rapid expansion and slow expansion should continue until the lingual cusp of the upper molar touches the buccal cusp of the lower molar. After expansion, the expander should be maintained for three to six months to prevent relapse from elastic recoil.18 Research has shown that without retention, expansion will relapse by 45%, on average. A fixed retention appliance can reduce relapse to 10% to 23%, while a removable retention appliance can reduce relapse to 22% to 25%.19
CONCLUDING POINTS AND SUMMARY
Most parents/caregivers do not wish to see their child’s self-esteem negatively affected by poor occlusion and esthetics. Understanding the benefits of improving a child’s appearance and correcting malocclusion at an early age is of value to all dental practitioners. These malocclusions include premature space loss, arch size/tooth size discrepancy, anterior crossbite, posterior crossbite, and craniofacial development problems.
In summary:
- In primary dentition, premature loss of a primary tooth is not a concern for arch length reduction until a posterior permanent tooth is actively erupting.
- Within 4 mm, incisor crowding in mixed dentition can be managed by IPR on primary canines and preserving leeway space.
- Patients with more than 4 mm incisor crowding or premature loss of a primary canine/molar need a thorough space analysis and skeletal development evaluation. A Phase I treatment including expansion, a 2×4 edgewise appliance, or serial extraction may be considered.
- Early correction of posterior crossbite is effective and efficient in either primary or mixed dentition. It needs to be overcorrected and retained at least three months after completion of activation.
Trends show that parents/caregivers are seeking orthodontic treatment for children at an earlier age. It has been demonstrated that many early dental and skeletal anomalies can be corrected or reduced in severity in primary or early mixed dentition by clinicians who remain abreast of the latest developments in this area of treatment.
Acknowledgement: The authors thank Jean M. Calvo, DDS, MPH, a resident at the University of California, San Francisco, School of Dentistry, for her help in preparing this manuscript.
REFERENCES
- Mayne WR. Serial extraction. In: Graber TM, Swain BF, eds: Current Orthodontic Concepts and Techniques. 2nd ed. Philadelphia: WB Saunders; 1969.
- Bishara SE, Jakobsen JR, Treder J, Nowak A. Arch width changes from 6 weeks to 45 years of age. Am J Orthod Dentofacial Orthop. 1997;111:401–409.
- Moorrees CF, Reed RB. Changes in dental arch dimensions expressed on the basis of tooth eruption as a measure of biologic age. J Dent Res. 1965;44:129–141.
- Gianelly AA. Crowding: timing of treatment. Angle Orthod. 1994;64:414–418.
- Bell RA, Sonis A. Space supervision and guidance of eruption in management of lower transitional crowding: a non-extraction approach. Semin Orthod. 2014;20:16–35.
- Owen DG. The incidence and nature of space closure following the premature extraction of deciduous teeth: a literature survey. Am J Orthod 1971;59:37–49.
- Shapira Y, Kuftinec M. The ectopically erupted mandibular lateral incisor. Am J Orthod. 1982;82:426–438.
- Hollander CS, Full CA. Midline correction by extraction of the remaining mandibular canine — myth or reality. J Dent Child. 1992;59:207–211.
- Atkinson CD. The case against early extraction of mandibular primary canines. J Am Dent Assoc. 1982;104:302–304.
- Sayin MO, Türkkahraman H. Effects of lower primary canine extraction on the mandibular dentition. Angle Orthod. 2006;76:31–35.
- Northway WM, Wainright RL, Demirjian A. Effect of premature loss of deciduous molars. Angle Orthod. 1984;54:295–329.
- Bell R, Kiebach T. Posterior crossbites in children: developmental-based diagnosis and implications to normative growth patterns. Semin Orthod. 2014;20:77–113.
- Kutin G, Hawes RR. Posterior cross-bites in the deciduous and mixed dentitions. Am J Orthod. 1969;56:491–504.
- Hesse KL, Artun J, Joondeph DR, Kennedy DB. Changes in condylar position and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997;111:410–418.
- Myers DR, Barenie JT, Bell RA, Williamson EH. Condylar position in children with functional posterior cross-bite: before and after crossbite correction. Pediatr Dent. 1980;2:190–194.
- Pinto AS, Buschang PH, Throckmorton GS, Chen P. Morphological and positional asymmetries of young children with functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2001;120:513–520.
- Malandris M, Mahoney EK. Aetiology, diagnosis and treatment of posterior cross-bite in the primary dentition. Int J Pediatr Dent. 2004;14:155–166.
- Zimring JF, Isaacson RJ. Forces produced by rapid maxillary expansion. 3. Forces present during retention. Angle Orthod. 1965:178-186.
- Timms D. Rapid Maxillary Expansion. Chicago: Quintessence Publishing Co; 1981.
The authors have no commercial conflicts of interest to disclose.
From Decisions in Dentistry. January 2020;6(1):18–21.