
Developing a Comprehensive Care Plan for Patients
Root resorption is the conclusion after data collection is complete in this case study of a 90-year-old woman.
The beginning of an appointment should start with a patient assessment, which includes a patient interview.1 The interview is used to determine if the patient has a chief complaint or any perceived changes since his or her last dental visit. The information provided by the patient can initiate the assessment of a selected area of the oral cavity. A thorough examination is still essential because early dental problems may be symptom free and clinically undetectable.2,3
Case Study
A 90-year-old woman returns to the dental office for her 4-month recare visit. The patient is a retired judge in favorable general health and is not currently taking any medications. The patient presents with no oral pain or concerns; however, she has a history of performing subpar oral hygiene. She does not practice routine flossing and presents with marginal biofilm at each appointment. An initial oral examination and full-mouth probing were performed by the dental hygienist. At the time of the visit, the buccal aspect of the lower right first premolar presented with an increase in pocket depth—from 2 mm to 6 mm. A dark purple discoloration of the soft tissue was also noted in this area (Figure 1,).

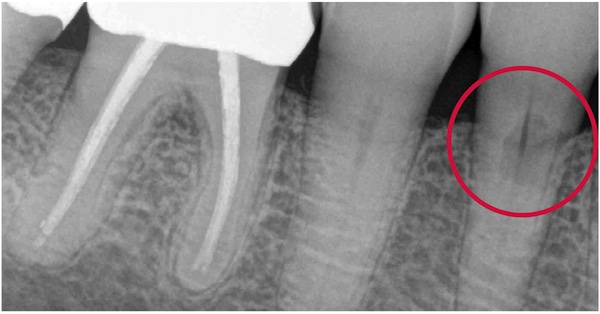
A full-mouth radiographic survey had been taken 15 months prior to this appointment. At that time, the radiographs had been evaluated by the dentist and no disease had been noted (Figure 2). Upon exploration with an ODU 11/12 explorer, a subgingival concavity in the root structure was detected approximately 4 mm below the cementoenamel junction and extending to the base of the pocket area. The dentinal surface of the root was hard, but the concave area was soft when gently explored with the ODU 11/12. Reflecting the tissue gently with a Marquis probe reveled an irregular defect in the root surface (Figure 3). The patient did not experience any pain when the subgingival defect was explored or probed.


When a concerning finding is made during the assessment stage of an appointment, the dental hygienist needs to form a dental hygiene diagnosis.1 This step involves data collection and consultation with the supervising dentist to discuss a comprehensive care plan for the patient.1 A new radiograph of the area may be necessary to complete the data collection process.
Understanding the problem is key to formulating the correct treatment plan. Careful attention to the location of abnormal findings, their clinical and radiographic appearance, and the presence of any etiologic agents can make accurate detection, diagnosis, and management possible. Detailed scaling of the root defect may not be the appropriate treatment for this tooth. Without a diagnosis, the tooth may be damaged by the incorrect treatment. Determination of a diagnosis and subsequent sequenced treatment plan is of paramount importance.
In this case, the dentist determined that a new periapical radiograph should be taken of the concerning area. A comparison of the past radiograph to the new radiograph showed a significant change to the root structure of the lower right first premolar. The new radiograph showed a large radiolucency in the root surface, with no apparent change in the nerve canal (Figure 4). These findings, combined with the clinical examination, revealed that the tooth presented with possible root resorption.
The next step was to determine which type of resorption was present on the root surface. Clinicians must understand how to differentiate between internal and external root resorption. Internal root resorption is its own unique entity, whereas external resorption can display many forms.4,5 Internal root resorption starts within the root canal space or pulp chamber, and the cells of origin are the pre-dentin lining of the pulpal area.4,5 Radiographs will show a radiolucency that involves the pulpal area of the tooth. Internal root resorption may focus on the coronal aspect of the tooth, causing bleeding into the crown. This can turn the crown a pink or purple color, otherwise known as “pink tooth.”6,7
The next installment of Perio Update on April 12 will discuss the different forms of root resorption.
References
- American Dental Hygienists’ Association. Standards for Clinical Dental Hygiene Practice. Available at: adha.org/resources-docs/떐-Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf. Accessed May 18, 2022.
- Mayo Clinic. Periodontitis—Symptoms and Causes. Available at: mayoclinic.org/diseases-conditions/periodontitis/symptoms-causes/syc-20354473. Accessed May 18, 2022.
- Mayo Clinic. Cavities/Tooth Decay—Symptoms and Causes. Available at: mayoclinic.org/diseases-conditions/cavities/symptoms-causes/syc-20352892. Accessed May 18, 2022.
- Blicher B. Differentiating resorption. Available at: aae.org/specialty/communique/differentiating-resorption. Accessed May 18, 2022.
- Tronstad L. Root resorption—etiology, terminology and clinical manifestations. Endo Dent Trauma. 1988;4:241–252.
- Warnsinck CJ, Shemesh H. [External cervical root resorption]. Ned Tijdschr Tandheelkd.2018;125:109–115.
- Battista P. Clinical manifestations of internal resorption. Decisions in Dentistry. 2016;2(6):24–27.
This information originally appeared in Smith D. The role of the dental hygienist in external root resorption. Dimensions of Dental Hygiene. 2022;20(6)14–21.


