Applications for Three-Dimensional Printing in Dentistry
Although its full potential for oral health care delivery is unknown, this additive method of fabrication has indications for treatment planning, orthodontics, oral surgery, restorative dentistry and other therapies.
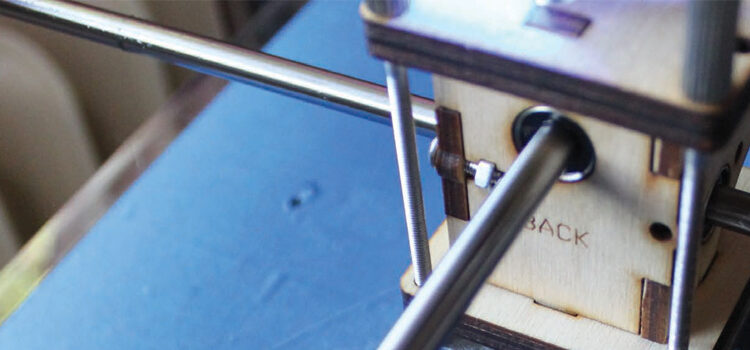
Technological advances in dentistry have increased accuracy, eased delivery and decreased chairtime, thus allowing dental teams to provide more effective treatment. The integration of digital impressions and computer aided design/computer aided manufacturing (CAD/CAM) are examples of how technology has revolutionized the approach to treatment. The evolution of newer modalities — including three-dimensional (3D) printing — has broadened the scope of dental practice. It has also benefited lab fabrication by creating a 3D final product via an additive process. Among other indications, 3D printing and CAD/CAM technologies allow precise fabrication of aligners, removable prosthetics and surgical templates for implants.1

© AMELIE-BENOIST/BSIP/SCIENCE SOURCE IMAGES
The use of 3D printing also has applications for oral and maxillofacial treatment, including orthognathic surgeries (Figure 1). It can produce models used for treatment planning and preoperative positioning of the jaws, as well as in the fabrication of splints and similar devices.2 Moreover, it is compatible with CAD software and digital files obtained during magnetic resonance imaging.3 The future is encouraging for the fabrication of crowns, bridges, inlays, onlays and dentures using 3D printing, but further research is needed to demonstrate the durability of the final product in the oral environment.
The 3D printing process starts by creating a virtual image of an object to be produced. This requires CAD software that converts the information into a digital file. If the goal is to replicate an existing object, a 3D scanner provides the digitized information, but in the creation of an entirely new object, a 3D modeling program produces the virtual design for the printer to follow.4
In the case of objects to be replicated, obtaining the image is similar to the process used with the milling technique, but the production processes used in milling and 3D printing are distinct. The milling technique utilizes a subtractive method in which the final product is carved from an existing block of material. The 3D printing process uses an additive approach in which the final product is created (i.e., printed) in layers.1
METHODS AND PROCESSES
Multiple 3D printing methods allow rapid prototyping, such as stereolithography (SLA), inkjet-based systems, selective laser sintering (SLS), and fused deposition modeling (FDM).5 Each of these technologies is utilized for the production of dental items, yet each offers advantages in the creation of particular types of products. Of these, SLA is widely utilized for reconstruction surgeries and producing surgical templates for implants. The use of SLS has demonstrated utility in the production of removable partial denture (RPD) frameworks, while the FDM method is useful for production of direct wax ups of dental restorations.5
In the dental field, SLA and inkjet-based systems are the most commonly used technologies. Once the digital image is obtained, both SLA and inkjet-based printing utilize 3D modeling software that cuts the final image into horizontal layers, and prints these in increments to create the final product.4 In the SLA process, the layers are laser cured, and the final step is to cure the entire model. Compared to inkjet-based systems, SLA technology is intended to produce larger objects, but it is a more cumbersome and less cost-effective production method.6
The inkjet-based technique utilizes a process in which a liquid polymer is cured layer by layer via a light source (e.g., UV or laser). A support system composed of gel-like material is employed during production.6 This support material can easily be eliminated with water once the printer is finished, and the item can be used immediately without having to wait for a final cure. This technique provides a quick and easy means of fabricating smaller objects in a precise manner.6
The SLS process uses a layer-by-layer deposition of a specific powder on a building cylinder. The layers are fused via a computer-operated laser. The laser facilitates optimal melting of the powder and, thus, efficient bonding through sintering of subsequent layers. Moreover, a wide variety of dental materials — such as nylon, thermoplastic composites, metals, casting waxes and ceramics — can be utilized with this method. For example, SLS technology has successfully produced cobalt chromium RPD frameworks.5
By comparison, FDM technology produces objects using a layer-by-layer deposition of a thermoplastic polymer material. The material is delivered through a nozzle apparatus, where it is transformed into a semi-liquid state and ejected onto the building base. The nozzle is temperature controlled and the motion is computer operated, resulting in the deposition of the thermoplastic polymer material. The semi-liquid thermoplastic material becomes solid within 0.1 second and bonds to the previous layer. The fabrication process occurs in a chamber in which the temperature is set just below the melting temperature of the thermoplastic material. This process is utilized for production of wax ups, and could produce approximately 150 items per hour.5
DENTAL IMPLICATIONS
There are various treatment modalities in which 3D printing can be advantageous. Orthognathic surgeries, for example, can be enhanced through the use of 3D printing. This is accomplished by performing a radiographic analysis, followed by a transfer of mandibular movements to the models. Surgical simulation is performed on the dental models to create the desired postoperative occlusion.7 Based on this preoperative analysis, a surgical wafer is fabricated using 3D printing. Used during the surgical phase, these wafers are essentially acrylic-based interocclusal splints that help to develop optimal occlusion.7
Conventional orthognathic surgeries require alginate impressions of the arches, obtaining a facebow record, and articulating the casts onto a semi-adjustable articulator. The dental models are manually positioned into the final postoperative occlusion, and the orthognathic surgical wafers are produced. The process can be cumbersome and time consuming, and can potentially contribute to errors.7 Cousley and Turner compared conventional fabrication methods for orthognathic surgical wafers with 3D printing.7 Alginate impressions were obtained for both arches and dental stone models were prepared. A 3D scanner produced digital images of the models, which were used to print the wafer utilized in developing final postoperative occlusion.7 The authors concluded that, compared to the conventional technique, 3D printing eliminated steps — including facebow recording and transfer to the articulator — that could affect the accuracy of the surgical wafer.7
This technology has also been used in mandibular reconstruction procedures. Cohen et al reported three clinical cases of mandibular reconstruction, including partial mandibulectomy performed in cases with ameloblastoma.6 Using 3D printing for oral and maxillofacial surgical procedures provides an opportunity to perform a preoperative finishing of the final mandibular reconstruction. It also allows surgeons to view 3D models and determine the essential preoperative steps that will allow more precise results.6
Orthognathic surgeries require a model surgery prior to the actual procedure, and the effectiveness of 3D printing and digital model surgery has been evaluated clinically. Model surgery provides a view of the postoperative jaw movement in three dimensions.8 Traditionally, this is accomplished with a manual model technique that can potentially lead to inaccuracies due to manual errors. Research by Kim et al suggests these inaccuracies could be minimized through digital modeling and 3D printing technology.8 Comparing the accuracy of manual and digital model surgery, their study showed that interocclusal wafers fabricated through digital printing were more accurate and precise than those fabricated with manual methods.8
Traditional orthognathic surgeries are performed with preoperative planning utilizing plaster study models. These conventional methods have limitations, however, such as a lack of control over movements of the cranium during the preoperative surgery performed on the plaster study model.9 Advances in digital technology have facilitated a combined approach utilizing traditional and digital methods — with improved postoperative results.9 The use of cone beam computed tomography (CBCT) allows clinicians to integrate 3D modeling software and facilitates the manipulation of the skull details into presurgical treatment planning.9 Metzger et al reported the use of such combined techniques on a patient with Class 3 malocclusion. The study suggests that even though digital aspects present advantages, in the interest of a more comprehensive result, the significance of manual manipulation should not be overlooked.9
key takeaways
- Three-dimensional (3D) printing creates a product via an additive production method, as opposed to milling, which is a subtractive process.
- This technology has indications for various dental uses, including orthognathic surgeries, oral and maxillofacial procedures, the fabrication of implant surgical guides, and prosthetic design and production.
- Some of the advantages of 3D printing include the precision of the final product, time savings, and the elimination of laboratory delays.
- Processes to create crowns, bridges, onlays, inlays and complete dentures could be accomplished using 3D printing, but further research is needed to clinically prove the effectiveness of this method for these procedures.
SURGICAL TEMPLATES
In implantology, 3D printing and CAD technology are also gaining acceptance for creating surgical templates.10 According to Fuster-Torres et al, the use of a CAD/CAM system, along with stereolithographic rapid prototyping, produces a surgical template that allows more accurate placement and orientation of implants.10
In 2014, Vidal and Vidal described a method that utilizes digital scanners, 3D printing and CBCT to allow implant planning in a complete digital protocol. The method involves taking intraoral and extraoral images in order to evaluate the esthetic requirements. The smile line, tooth position and gingival margins are evaluated and marked digitally.11 Study models are scanned with a 3D scanner, creating a virtual digital wax up. This allows clinicians to determine the desired implant position.11 Next, a tomographic implant guide is produced using CAD software and 3D printing. The guide is subsequently positioned while CBCT images are obtained and utilized in a virtual surgery to determine final implant placement and position.11
The actual surgical guide is modeled and printed when the CBCT image of the tomographic guide and digital wax up are integrated and confirmed as a viable placement plan.11 The study showed that the implants were accurately placed, as per the presurgical implant planning conducted through the combined use of CBCT, scanning and 3D printing. The implant sites showed proper healing and were later restored appropriately.11 This combined use of technological advances was shown to be more precise than conventional methods of manual wax up and fabrication of surgical templates.11
Three-dimensional printing represents a promising technology that could bring an array of advanced treatment modalities
Schneider et al conducted a literature review to examine the accuracy and clinical application of computer-guided, template-based implant dentistry. They found six clinical trials that demonstrated a survival rate of 91% to 100% after a 12-month to 60-month observation period for implants placed using computer-based systems.12 Ghiuta et al studied the efficacy of using a CAD/CAM system along with stereolithographic printing for the fabrication of implant surgical templates, and the subsequent functional loading of the implants.13 The results indicated that the implants were placed without complications.13 The surgery was flapless and the postoperative examination showed no signs of pain, bleeding or swelling.13
FABRICATING RESTORATIONS
When fabricating restorations, conventional CAD/CAM milling systems provide a number of advantages to clinicians and patients, including precision (and, in the case of in-office milling systems, same-day restorations). But there are also disadvantages to subtractive production methods. Milling the restoration from a ceramic block, for example, wastes some of the raw material. In addition, exposure to tooling during production presents the possibility of microscopic cracks in the ceramic surface. These shortcomings could be minimized or even eliminated with 3D printing.14
Elbert et al examined the effectiveness of direct inkjet 3D printers in producing zirconia-based dental prostheses. The study utilized a ceramic suspension composed of zirconia powder, distilled water, boehmite sol and dispersants. The results suggest this process is capable of producing components of the size and shape — and with the occlusal features — of a crown.14 Although the printed prosthetics showed some microscopic cracks, the density of the printed components was estimated at 96.9% — which would provide the strength and physical properties needed for oral function.14
Another study described the technique of producing core and fixed partial denture (FPD) frameworks and robocasting crown structures using a process in which ceramic materials are built up using additive technology.15 The study described two methods of robocasting. One utilized a process in which the core is printed from zirconia-based ink via a stereolithography file. The second is a fugitive process in which carbon black is codeposited with the ceramic material.15 The carbon black is removed during sintering.15
A study by Hussein and Hussein included the fabrication of an RPD framework for a mandibular Kennedy Class 1 arch utilizing a study cast made from a silicone-based impression material.3 A digital file of the cast was generated with a 3D scanner, and the RPD framework was created using software to design the components, such as the connectors and clasps. The framework was printed using polymer powder and a CO2 laser. The authors concluded that the final result exhibited optimal adaptation to the original cast.3 While production costs were comparable to conventional methods, the authors reported that printed fabrication was more efficient.3
Bibb et al assessed the efficacy of a method that combined CAD and 3D printing via selective laser melting (SLM). The study utilized a 3D scan of a partially edentulous patient cast, which allowed digital design of the RPD’s components.16 Using SLM, one framework was fabricated from stainless steel, and a second was produced using cobalt chromium alloy, thus providing two frameworks for comparative purposes. Compared to the stainless steel framework, the cobalt chromium framework proved more efficient. Both exhibited accurate fit on the patient cast, but the retentive components of the stainless steel framework showed deformation after repeated insertion and removal.16 In addition to showing no signs of deformation, the cobalt chromium framework fit well on the cast, and also in the patient.16 Compared to manual investment and casting procedures — and in terms of preparation time and opportunity for errors — this research supports the viability of using 3D printing to produce RPD frameworks.16
CONCLUSION
Although 3D applications are becoming more common, at this juncture we do not know this technology’s full potential for oral health care delivery. One area that shows promise, for example, is its use in producing crowns, bridges and complete dentures. Although precise fit appears to be a major advantage, human tactile sense may still be helpful in producing ideal restorations. More extensive studies of 3D printing are required to prove the overall effectiveness of this modality for restorative procedures and other dental therapies.
As dentistry continues to evolve, it is important for clinicians keep abreast of advances that have the potential to benefit both practitioners and patients. In this regard, 3D printing represents a promising technology that could bring an array of advanced treatment modalities to the dental community.
References
- Bunek S, Brown C, Yakas M. The Evolving Impressions of Digital Dentistry. Inside Dentistry. 2014. Available at: https://id.cdeworld.com/courses/4733- The_Evolving_Impressions_of_Digital_Dentistry. Accessed June 10, 2016.
- Yun PY. The application of three-dimensional printing techniques in the field of oral and maxillofacial surgery. J Korean Assoc Oral Maxillofac Surg. 2015;41:169–170.
- Hussein MO, Hussein LA. Novel 3D modeling technique of removable partial denture framework manufactured by 3D printing technology. Int J Adv Res. 2014;9:686–694.
- 3DPrinting.com. What is 3D printing and How Does it Work? Available at: http://3dprinting.com/what-is-3d-printing/#whatitis. Accessed June 10, 2016.
- Azari A, Nikzad S. The evolution of rapid prototyping in dentistry. Rapid Prototyping J. 2009;15:216–225.
- Cohen A, Laviv A, Berman P, Nashef R, Abu-Tair J. Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:661–666.
- Cousley R, Turner M. Digital model planning and computerized fabrication of orthognathic surgery wafers. J Orthod. 2014;41:38–45.
- Kim BC, Lee CE, Park W, et al. Clinical experiences of digital model surgery and the rapid prototyped wafer for maxillary orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:278–285.
- Metzger MC, Hohlweg-Majert B, Schwarz U, Teschner M, Hammer B, Schmelzeisen R. Manufacturing splints for orthognathic surgery using a three dimensional printer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e1–e7.
- Fuster-Torres MA, Albalat-Estela S, Alcaniz-Raya M, Penarrocha-Diago M. CAD/CAM dental systems in implant dentistry: Update. Med Oral Patol Oral Cir Bucal. 2009;14:E141–E145.
- Vidal F, Vidal R. Development of a novel protocol for digital implant planning using cone beam CTs, scanners and 3D printers: the full digital implant planning protocol. Clin Oral Implants Res. 2014;25(Suppl):175.
- Schneider D, Marquardt P, Zwahlen M, Jung RE. A systematic review on the accuracy and the clinical outcome of computer guided template-based implant dentistry. Clin Oral Implants Res. 2009;20(Suppl):73–86.
- Ghiuta C, Cristache CM, Mihai A, et al. Predictable computer guided flapless surgery for dental implants insertion. Acta Medica Transilvanica. 2015;20(2):119–122.
- Ebert J, Ozkol E, Zeichner A, et al. Direct inkjet printing of dental prostheses made of zirconia. J Dent Res. 2009;88:673–676.
- Silva NR, Witek L, Coelho PG, Thompson VP, Rekow ED, Smay J. Additive CAD/CAM process for dental prostheses. J Prosthodont. 2011;20:93–96.
- Bibb R, Eggbeer D, Williams R. Rapid manufacture of removable partial denture frameworks. Rapid Prototyping J. 2006;12:95–99.
From Decisions in Dentistry. July 2016;1(09):28–30,32.


![The controversy around adding fluoride to drinking water was recently highlighted by an article in the Wall Street Journal, which addressed its possible negative neurological effects on children.[1] The article cited recent studies on what levels of fluoride are needed to protect teeth without risking possible cognitive harm to prenatal children and infants. Link in bio.
[1] Data on link.
---
#dentistry #dentist #dental #smile #dentista #teeth #cosmeticdentistry #dentistryworld #dentalphotography #odonto #tooth #dentistrylife #orthodontics #dentalcare #dentalhygienist #dentalimplants #oralhealth #veneers #dentalstudent #dentalassistant #dentalclinic #dentistlife #dentalhygiene #teethwhitening #oralsurgery #dds #endodontics #continuingeducation #education](http://decisionsindentistry.com/wp-content/plugins/instagram-feed/img/placeholder.png)