 VIOLETASTOIMENOVA/E+/GETTY IMAGES PLUS
VIOLETASTOIMENOVA/E+/GETTY IMAGES PLUS
Shared Approach to Oral-Systemic Health
Medical-dental integration is key in the effort to improve patients’ oral-systemic health.
This course was published in the November 2021 issue and expires November 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the oral-systemic link and the role inflammation plays in oral and systemic diseases.
- Explain the advantages and challenges of medical-dental integration in the continuum of care.
- Cite examples of the impact of medical-dental integration on outcomes and the cost of healthcare.
The upper gastrointestinal system contains one of the most multifunctional organs of the human body, the oral cavity. Systemic diseases and disorders have a significant negative effect on the oral cavity’s ability to function and contribute to health and well-being. Conversely, disorders that originate here may negatively impact other organs.1 Given the importance and complex functionality of the oral cavity, the healthcare system must recognize and address this oral-systemic connection to enhance patients’ quality of life.2,3 Though medicine and dentistry have been separated by financing, training and education, practice location, language, and even anatomy, the two disciplines must work together in addressing the shared health of patients.
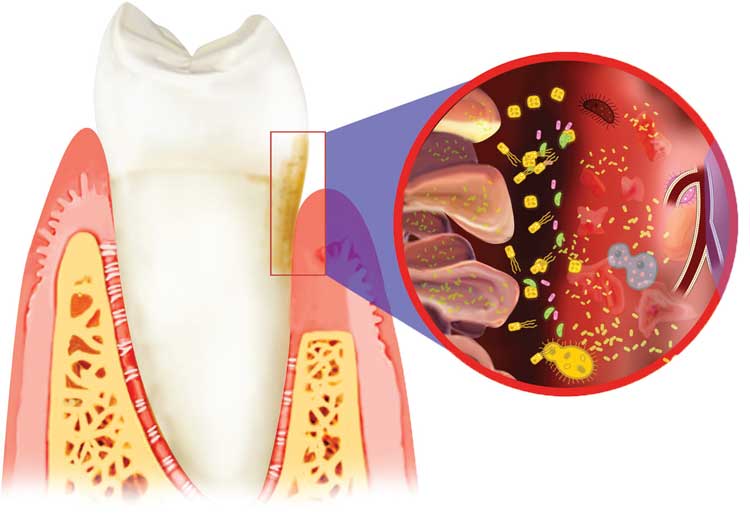
The nutritional quality of an individual’s diet and intake frequency play a primary role in health, especially oral health. When introduced with regularity, fermentable foods and fluids produce an oral environment that causes fluctuations in pH, prolonged secretion by aciduric bacteria, and a potentially unhealthy mix of microorganisms.4 This dysbiosis promotes tissue damage and infection. As seen in Figure 1, chronic oral dysbiosis contributes to systemic inflammation and increases in the plasma concentration of acute-phase proteins, granulocytes, inflammatory cytokines, and coagulation factors.5 These circulating inflammatory mediators exacerbate other inflammatory conditions, including arthritis, cardiovascular disease and diabetes.6 This systemic inflammatory state makes it difficult to effectively treat and arrest systemic disease without addressing oral dysbiosis and inflammation.
Collective Desire to Improve Healthcare
Science continues to demonstrate the value of addressing the inflammatory processes of the oral cavity to improve systemic health. Previous research has found improved glycemic control in patients with type 2 diabetes who have had well-managed periodontal disease, as well as risk mitigation of other associated inflammatory disorders, such as cardiovascular disease.7,8 An economic analysis of integrated care models found that periodontal treatment coverage among patients with type 2 diabetes would be expected to avert tooth loss by 34%, and microvascular diseases, such as nephropathy, neuropathy and retinopathy, by approximately 20%.9 The authors concluded that utilization of periodontal treatment across a healthcare sector could realize a net savings of $5904 per capita.
Reciprocal value is evident in a recent report from the U.S. Centers for Disease Control and Prevention that projected annual healthcare savings of $100 million if dentists would screen for diabetes, hypertension and high cholesterol.10 In a recent evaluation of interprofessional and colocated healthcare teams, 1729 previously unengaged or non-engaged medical patients with diabetes closed care gaps after an integrated dental visit.11 Dental patients seen by a fully integrated care team were more likely to close care gaps for cancer screenings and diabetic care than patients at other dental offices. Additionally, a care site that implemented flu shots in dental offices reported that 98% of surveyed patients positively rated their care experience, with 67% mentioning convenience as a primary factor in their satisfaction.11
The development of early childhood caries can be prevented on multiple levels based on interventions by parents/caregivers and primary healthcare providers. During the first three years of life, children are seen in the medical setting for well-child visits and immunizations approximately 11 times, while they may see a dentist once or twice, if at all.12 Given the importance of this period for oral health, the integration of preventive measures to support oral health by a broader healthcare team can have significant impact on quality of life. A big-data report found that when children experience an oral health interaction during well-child-visits by a medical care team, they are more likely to be seen by a dentist, have preventive dental care, and to be seen at an earlier age than those who did not.13
Shared Need to Produce Revenue
Medical-dental integration (MDI) has traditionally been a hard sell to most healthcare teams. The main hurdles correlate with a need for medical and dental practices to reach their financial goals, and include lack of overall team capacity, a time-compressed medical or dental visit driven by production goals, and lower reimbursement rates for MDI services. The last five years have seen significant advancement of reimbursement opportunities for medical care teams. At presstime, 43 states reimburse medical providers through their Medicaid programs for addressing children’s oral health, including services provided in the context of a well-child visit, such as fluoride application, oral health evaluation, and oral health risk assessment. These programs pay between $11 and $78 for various oral healthcare services, up to age 21.12 State-based projections of annual revenue for medical care sites found $55,432 to $73,102 in additional reimbursement for adding oral health to 20 well-child visits per week.12 Multiple medical commercial insurance companies reimburse for oral health services; however, they usually only pay for the first four to six years of life.
While dental billing codes for medical screening and primary care services are available, the reimbursement pathways for dental teams are more limited than those available to medical teams. Most insurance carriers and state Medicaid agencies do not typically reimburse for MDI-related services by oral health practitioners. According to a report from the American Academy of Pediatric Dentistry, approximately 8% of state Medicaid plans reimburse for codes associated with medical screening or other MDI opportunities, such as nutritional counseling (CDT-D1310), consultation with medical healthcare professional (CDT-D9311), and care coordination (CDT-D9992).14 Codes for diabetes screening/monitoring (CDT-D0411–D0412) and vaccine administration (CDT-D1701–D1707) have recently been approved, but it will take time to determine their utilization and understand opportunities for reimbursement. Currently, dental teams will find more MDI-related financial opportunities in alternative payment models or accountable care organizations. These models often pay for performance and offer incentives for achieving quality benchmarks for specific process and health outcomes measures. In 2018, 60% of U.S. healthcare payments were tied to quality and value.14 While commercial dental plans were exclusively fee for service, an estimated 33% of all Medicaid dental claims were associated with alternative payment models in 2017.15
Opportunities and Challenges
Buoyed by shared science, several successful MDI initiatives have filled the oral health knowledge gap. These initiatives train healthcare personnel to incorporate oral health into day-to-day practice and empower multidisciplinary approaches to prevention and treatment. While these initiatives have laid the foundation for MDI, there is a need to see greater adoption and improved scaling of best practices. At least four key areas of action are needed to continue to drive and positively impact MDI models: technology as a teammate, support beyond the champions, payment reform to better align cost of services, and changing patient expectations.
Technology As a Teammate
Many healthcare providers face a heavy production schedule mixed with too many administrative responsibilities. Over the last decade, these tasks have been complicated by digital technology that can be unwieldy and requires manual data entry. Clinicians also face regulatory reporting requirements — albeit with limited reporting capability. These deficiencies and provider dissatisfaction have led healthcare organizations to increase investment in process automation and artificial intelligence. A 2021 report found that 94% of provider executives, 92% of life sciences executives, and 91% of health plan executives said improving the clinician experience is a priority for their organizations.16 Approximately 73% of this group said their organizations are already automating the healthcare team’s administrative tasks as a step toward improving the provider experience. According to a report from the Council for Affordable Quality Healthcare, the healthcare industry could save $16.3 billion (including $3 billion in dental costs) by automating common administrative transactions and tasks.17 By streamlining communication between insurance companies and care teams, improving electronic health record (EHR) usability and reporting mechanisms, and enhancing electronic referral opportunities for interprofessional care teams, providers would have more time for patient interaction, decrease overhead and external dependencies, and improve opportunities for holistic care.
Health information technology is beginning to provide solutions for integrating data and shared information between medicine and dentistry.18 Improvement in these tools is vital for MDI, as medical and dental teams would be more likely to coordinate care if EHR systems were easier to use by all parties.19 While medicine is currently using data standards to pass patient information back and forth with medical EHRs, dental data standards are still in testing. Data standards are documented agreements on the format, definitions, coding structure, use, alterations, and management of data. Under these standards, EHR systems and software can assign unique identifiers to dental care information, such as risk status, clinical diagnosis, and medical histories, to name a few. This will make it possible to electronically capture and send a patient’s dental care information and reports across different EHR systems, utilize technology to better connect traditionally fragmented care teams, and reduce the time spent on administrative tasks.
Support Beyond the Champions
Many medical and dental care teams feel they do not have enough time to move beyond problem-based or acute care encounters, and face increasing pressure to meet daily production demands. This has led to compassion fatigue, burnout, and increased depression among U.S. healthcare providers — which have been exacerbated by the COVID-19 pandemic.20 Traditional MDI piloting and improvement collaboratives depend on individual innovators and early adopters to promote initiatives and institutional adoption and sustainability of MDI. A report found that these “significant-change” champions utilized for change-management programs often burn out, lose motivation, and experience too many system challenges to support program sustainability.21 To be sustainable, change-management programs and processes must include payer and business operations, clinical care delivery, and community and organizational stakeholders. For change to extend beyond the champions and early adopters, it is helpful — and probably necessary — to favorably answer at least three questions.22
- How will the change relieve, rather than add to, the clinical workload?
- How will the change measurably improve the patient’s health and care experience?
- Is there an ongoing revenue stream to support the continuation of the work?
After all, more work without measurable benefit or funding is a non-starter for clinicians, patients and business managers.
Payment Reform
The current healthcare system results in significant inequities that interfere with an MDI continuum of care. Individuals below the poverty level spend 10 times more as a percentage of earned income on dental care than wealthier families.23 These inequities are compounded by the fact that twice as many people lack dental coverage compared to medical insurance. Furthermore, fewer than half of those with dental coverage use dental services, compared to over 80% of people with medical insurance who use the medical system.24 Coverage gaps make it difficult to coordinate care delivery and complete closed-loop referrals; they also place a financial strain on both the individual and care model. Current changes in benefit design, mixed with financial healthcare reform, are needed to create a more equitable and better performing care delivery system. Market research has demonstrated that patients, Medicaid administrators, and employers want oral healthcare benefits focused on the impact the service has on health and quality of life, as opposed to prioritizing payment for dental procedures.25
Changing Patient Expectations
Patients are changing their expectations of care delivery and becoming more consumer-oriented with their healthcare choices. Informed by more than just cost, these expectations are guided by: patients proactively using their health information to make better-informed care decisions; improved financial rewards and mainstream health and wellness marketing that encourage personal health involvement; and accessibility to determine the reputation of a provider, care site or health business with online reviews and peer communities. In a 2020 health consumer report, surveyed patients were more willing to tell care providers when they disagree, more comfortable to use technology for health data monitoring and provider accountability, and more willing to share data for health improvement.26 The report also found that top factors for an “ideal health experience” include a trusted relationship with the care team or health organization, an encounter that is convenient and not rushed, limited wait times, ease with booking appointments, and interactions during care delivery that allow for loyalty and relationship building.
The changes underway in healthcare have led to the development of care delivery models that focus on service aspects (such as convenience and speed), as well as the use of technology, standardization, big data, and more non-dentist/non-physician staff in care delivery.27 As patients interact with these models, there will be a tug-of-war between achieving an economically prudent experience and individualized care that addresses the emotional contexts of health status.28,29 The joy of practice for most healthcare professionals is the creation of these personal connections and building trust — goals that patients also value in a healthcare setting.
Conclusion
Opportunities abound at every level of the healthcare system to facilitate MDI in order to improve oral-systemic outcomes. The shared science surrounding inflammation’s impact on oral and systemic health, and the systemic quid pro quo of addressing that inflammation, can be translated into interprofessional practice. Innovative models of benefit design and financial reform of healthcare can drive practitioners to better integrate medicine and dentistry. Health information technology and data standardization can facilitate communication, collaboration, and integration toward a value-based model of care. Organizational culture that nurtures innovation and collaboration with communities will support a more sustainable model of change, particularly if workload, measurable benefits, and financial viability can be favorably addressed. Though barriers exist, they are not insurmountable, and models already exist that are overcoming these challenges.
References
- Babu NC, Gomes AJ. Systemic manifestations of oral diseases. J Oral Maxillofac Pathol. 2011;15:144–147.
- National Association of Community Health Centers and CareQuest Institute for Oral Health. Oral Health Value-Based Care: The Federally Qualified Health Center (FQHC) Story. Available at: https://www.carequest.org/system/files/Oral-Health-Value-Based-Care-The-Federally-Qualified-Health-Center-Story.pdf?mc_cid=cb3f567776&mc_eid=84dd925fca. Accessed October 15, 2021.
- Rubin MS, Edelstein BL. Perspectives on evolving dental care payment and delivery models. J Am Dent Assoc. 2016;147:50–56.
- Moynihan PJ. The role of diet and nutrition in the etiology and prevention of oral diseases. Bull World Health Organ. 2005;83:694–699.
- Fitzsimmons TR, Sanders AE, Slade GD, Bartold PM. Biomarkers of periodontal inflammation in the Australian adult population. Aust Dent J. 2009;54:115–122.
- Sanz M, Ceriello A, Buysschaert M, et al. Scientific evidence on the links between periodontal diseases and diabetes: Consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the International Diabetes Federation and the European Federation of Periodontology. Diabetes Res Clinical Pract. 2018;137:231–241.
- Altamash M, Klinge B, Engström P-E. Periodontal treatment and HbA1c levels in subjects with diabetes mellitus. J Oral Rehabil. 2016;43:31–38.
- Peng CH, Yang YS, Chan KC, Kornelius E, Chiou J-Y, Huang C-N. Periodontal treatment and the risks of cardiovascular disease in patients with type 2 diabetes: a retrospective cohort study. Intern Med. 2017;56:1015–1021.
- Choi SE, Sima C, Pandya A. Impact of treating oral disease on preventing vascular diseases: A model-based cost-effectiveness analysis of periodontal treatment among patients with type 2 diabetes. Diabetes Care. 2020;43:563–571.
- U.S. Centers of Disease Control and Prevention. Return on Investment: Healthcare System Savings. Available at: https://www.cdc.gov/oralhealth/infographics/roi-healthcare.html. Accessed October 15, 2021.
- Zokaie T. Redefining Total Health: Medical Dental Integration in the Northwest. In: APHA’s 2019 Annual Meeting and Expo. 2019.
- Silk H, Deutchman M. Offering oral health services in your office. Fam Pract Manag. 2014;21:21–24.
- Tiwari T, Rai N, Brow A, Tranby EP, Boynes SG. Association between medical well-child visits and dental preventive visits: a big data report. JDR Clin Trans Res. 2019;4:239–245.
- American Academy of Pediatric Dentistry. Are your kids covered? Available at: https://www.aapd.org/assets/1/7/AreYourKidsCoveredfinal.pdf. Accessed October 15, 2021.
- Boynes SG, Brown C, Tranby EP. Exploring alternative payment models for oral health care. Decisions in Dentistry. 2020;6(1):30–32,35.
- PWC Health Research Institute. Top health industry issues of 2021: Will a shocked system emerge stronger? Available at: https://www.pwc.com/us/en/industries/health-industries/top-health-industry-issues.html. Accessed October 15, 2021.
- 2020 CAQH Index. Closing the Gap: The Industry Continues to Improve, But Opportunities for Automation Remain. Available at: https://www.caqh.org/sites/default/files/explorations/index/2020-caqh-index.pdf. Accessed October 15, 2021.
- CareQuest Institute for Oral Health. Oral Health Interoperability and Care Coordination. Available at: https://www.carequest.org/system/files/Interoperability%20and%20Care%20Coordination.pdf. Accessed October 15, 2021.
- Boynes SG, Lauer A, Deutchman M, Martin AB. An assessment of participant-described interprofessional oral health referral systems across rurality. J Rural Health. 2017;33:427–437.
- Potter P, Deshields T, Divanbeigi J, et al. Compassion fatigue and burnout: prevalence among oncology nurses . Clin J Oncol Nurs. 2010;14:E56–E62.
- Chrusciel D. What motivates the significant/strategic change champion(s)? J Org Change Manag. 2008:21:148–160.
- Lynch DA. Three questions to guide any change effort. Fam Pract Manag. 2014;21:40.
- Halasa-Rappel YA, Brow A, Frantsve-Hawley J, Tranby EP. Poor Families Spent 10 Times More of Their Income on Dental Care Than Wealthier Families. Available at: https://www.carequest.org/system/files/CareQuest-Institute-Poor-Families-Spend-10-Times-More-Brief-Part1.pdf. Accessed October 15, 2021.
- Mertz EA. The dental-medical divide. Health Aff (Millwood). 2016;35:2168–2175.
- DentaQuest. Reversible Decay: Oral Health Is a Public Health Problem We Can Solve. Available at: https://dentaquest.com/pdfs/reports/reversible-decay.pdf/. Accessed October 15, 2021.
- Deloitte. Are consumers already living the future of health care? Available at: https://www2.deloitte.com/lu/en/pages/life-sciences-and-healthcare/articles/consumer-health-trends.html. Accessed October 15, 2021.
- Hoff T. The challenges of consumerism for primary care physicians. Am J Manag Care. 2020;26:e1–e3.
- American Association of Family Physicians. The Medical Home. Available at: https://www.aafp.org/family-physician/practice-and-career/delivery-payment-models/medical-home.html. Accessed October 15, 2021.
- Paige L. 8 ways to compete successfully with retail clinics. Available at: https://www.medscape.com/viewarticle/908745_1. Accessed October 15, 2021.
From Decisions in Dentistry. November 2021;7(11)32-35.




