Recognize the Signs of Eating Disorders
By noting the early symptoms of anorexia nervosa and bulimia nervosa, oral health professionals can help patients receive the treatment they need.
The authors have no commercial conflicts of interest to disclose.
This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Define anorexia nervosa and bulimia nervosa.
- Discuss predisposing factors for these eating disorders.
- Identify the oral complications for anorexia and bulimia.
- Detail the tools used for eating disorder diagnosis.
- List strategies for helping patients with anorexia or bulimia
protect their oral health.
Bulimia and anorexia are classified as compulsive psychosocial disorders affecting individuals’ perceptions and relationships with their bodies and food, which results in distorted eating behavior and habits.7,8 A distorted body image and an intense preoccupation with food and weight, coupled with a morbid fear of becoming obese, are common elements in both.9 The cause of these disorders is a complex interaction of genetic, biological, behavioral, psychological and social factors.10
Anorexia commonly begins during adolescence or young adulthood. Although it rarely begins before puberty or after age 40, cases of early and late onset have been described. Anorexia is characterized by excessive dieting that leads to severe weight loss and an intense fear of gaining weight.
Similar to anorexia, bulimia usually begins in adolescence or young adulthood, and onset before puberty or after age 40 is uncommon. Bulimia is characterized by recurrent and impulsive eating sprees, during which large quantities of food are consumed, followed by gastric purging, use of laxatives, diuretics, fasting or excessive exercise to prevent weight gain. Binges are often associated with an intense negative emotional experience, such as rejection, depression or stress, followed by strong feelings of guilt.11 Individuals with anorexia who restrict food intake may also have episodes of binge eating and vomiting, and those with bulimia who regularly binge and purge to prevent weight gain may also have periods of severe food restriction.12
PREVALENCE
In the past, affected girls or women usually came from middle to high socioeconomic backgrounds, but now eating disorders have become common in all socioeconomic groups.13,14 There often exists a family history of psychoneuroses, particularly depression, schizophrenia, obsessive-compulsive personalities and alcoholism. These factors appear to predispose some individuals to difficulties in self-restraint, poor self-esteem and insecurities. The intake of food and food choices often becomes the means by which affected individuals attempt to gain control of personal issues.15 Although a specific etiology for the pathogenesis of anorexia and bulimia remains elusive, interest has focused on environmental and social factors, biological vulnerability, and psychological and genetic predisposition.16
The prevalence of eating disorders is similar among nonHispanic whites, Hispanics, African-Americans, and Asians in the U.S. — with the exception that anorexia is more common among nonHispanic whites.17,18 Latinos do not have elevated rates of bulimia or anorexia, however, binge eating disorders (not associated with purging) are more common among this group.19
There has been a rise in the number of reported cases of eating disorders among boys and men.20,21 Individuals of both genders who are involved in sports that necessitate weight control in order to achieve success, such as bodybuilding, cheerleading, dancing (especially ballet), distance running, diving, figure skating, gymnastics, horse racing, rowing, swimming, boxing and wrestling are at increased risk for eating disorders.22,23
ANOREXIA NERVOSA![1215-eating-3]()
Anorexia is associated with life-threatening medical issues, including cardiac arrest and suicide. Suicide rates of 12 per 100,000 per year have been reported.11 Approximately 1% of female adolescents meet the American Psychiatric Association’s diagnostic criteria for anorexia,11,13,24,25 and the highest rate of occurrence is between the ages of 15 and 19.26 Although it varies between studies, a lifetime prevalence of 0.9% for women and 0.3% for men has been reported.27 A review of almost 50 years of research has confirmed that anorexia has the highest rate of death of any psychiatric disorder.28 Overall, individuals with anorexia have a six-fold increase in mortality compared to the general population.29,30
Evidence suggests that anorexia has biological, psychological and sociocultural components. Predisposed individuals are at greater risk when living in an industrial society that associates slimness with beauty. An obsessive and compulsive goal of thinness can lead to unhealthy weight loss below the minimum recommended for age and height. Excessive weight loss can result from severe and selective food restriction, excessive exercise, and/or use of purgatives and laxatives. An impaired sense of personal identity, perceptual disturbances, childhood obesity, familial history of eating disorders, rigid relationships with over-protective parents who discourage adolescent autonomy, a personality characterized by perfectionism, cognitive disturbances and neuroendocrine vulnerability are predisposing factors.31
Almost all organ systems are affected by the behavior and diet choices associated with anorexia, including metabolic, cardiovascular and endocrine disturbances caused by self-induced starvation and generalized cachexia (wasting syndrome). Mild diabetes insipidus and abnormal thermoregulatory responses when exposed to temperature extremes have been reported. Dysfunction of the hypothalamic-pituitary-adrenal axis can result in amenorrhea and osteoporosis in women relative to diminished estrogen secretion. Hypotension, bradycardia, muscle loss and weakness, and severe dehydration can result in kidney failure, fainting, fatigue, and dry hair and skin.7,32–34 Diminished libido and impotence have been reported in affected men.23 Fortunately, some of the metabolic and physical disturbances and physical changes are reversible with therapy that encourages appropriate medical care and healthy weight gain, coupled with psychological counseling.35 Individuals with anorexia are at high risk, however, for relapse — even with professional intervention.36
BULIMIA NERVOSA
The etiology of bulimia is unknown, but appears to be associated with individual, family and sociocultural values, such as admiring thinness, and certain personality traits, such as perfectionism.37 The disorder is associated with marked distress and occurs on average at least once per week over an extended period.11 The prevalence of bulimia is about 1% to 1.5% among women, with 20 to 24 being the typical age of onset.26,36
Binge eating occurs frequently at night and is followed by purging (vomiting/emesis) of the gastric contents. The goal of vomiting is to prevent weight gain. Individuals who primarily practice binge/purge behavior are often of normal or near normal weight, and may not initially demonstrate signs of serious medical involvement or complications.38
Outgoing personalities and compulsive behaviors are common among individuals with bulimia. Episodes of depression, anxiety, fascination with food, distorted body perception, feelings of inadequacy and helplessness appear to predispose an individual to bulimia.39 Individuals who practice behaviors associated with bulimia are also at risk for early death, including an elevated risk of suicide.11 They are at significant risk for electrolyte imbalances and associated cardiac issues, dehydration, gastric rupture, inflammation and possible rupture of the esophagus, peptic ulcers and pancreatitis, laxative dependency, and excessive amount of fat in the feces.40,41
ORAL COMPLICATIONS
Dietary choices and the duration and frequency of binge/purge behavior are the primary variables that impact the oral complications associated with anorexia and bulimia. Regurgitating the acidic contents of the stomach can result in loss of tooth structure if the practice is habitual and long-standing. Dental erosion (perimolysis) is a common finding in patients with bulimia, but can also be observed in individuals with anorexia.42 The lingual and incisal/occlusal enamel surfaces of the maxillary incisors and premolars are most affected because they are less protected by the tongue and have less contact with pooled saliva. The occlusal surfaces of the mandibular premolars and molars may also be affected — but not as frequently as those in the maxilla because the tongue affords some protection, as does salivary buffering and the close contact with the mucous membranes of the cheeks.42 Aggressive tooth brushing, especially immediately after regurgitation, can increase the loss of tooth structure due to enamel fragility.
Because of weight-related distractions, individuals with anorexia may neglect their personal grooming and hygiene, including their teeth and oral soft tissues. In contrast, individuals with bulimia are conscious of their personal appearance and typically practice good oral hygiene.
Reports of caries incidence among individuals with eating disorders have been inconsistent.43–45 These conflicting observations may be the result of varying intensity of personal oral hygiene practices, cariogenicity of the diet, genetic predisposition, fluoride exposure and salivary flow.
Painless, nonpathological enlargement of the parotid(s) and submandibular salivary glands is often seen in patients who practice binge/purge behavior. These enlargements can occur unilaterally or bilaterally.46 The definitive cause has not been established,47 but the gland enlargements are self-limiting and the gland returns to normal size when the binge/purge behavior is discontinued.
Pharyngeal tears and erythema of the palate, pharynx and posterior tongue can result from the use of fingers or other objects — such as tongue blades and spoons — to induce gagging and regurgitation. The low pH of the vomitus can add additional insult to the soft tissues.48 Angular cheilosis and necrotizing gingivitis are associated with loss of moisture and protective qualities of saliva.42,49 Dehydration of the oral cavity’s soft tissues can be exaggerated if the individual is regularly taking prescription or over-the-counter medications, as many medications reduce salivary secretions.
IDENTIFICATION AND DIAGNOSIS
Identifying patients with eating disorder behaviors may be challenging for oral health professionals.50 DeBate et al51 reported that dental hygienists were more skilled in identifying oral manifestations of eating disorders than dentists. They also found that only 16% of surveyed dentists had knowledge of the oral cues commonly found among individuals with eating disorders.
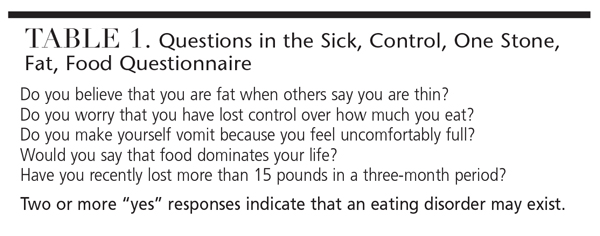
The sick, control, one stone, fat, food (SCOFF) questionnaire was developed and evaluated in the United Kingdom (1 stone equals 14 pounds).52 A screening instrument designed for nonspecialists, it was designed to alert health professionals that an eating disorder might exist. When tested among a group of women age 18 to 50, the questionnaire was found to be very reliable in detecting individuals with unreported eating disorders.52 A strong suggestion of an eating disorder exists if a patient responds “yes” to two or more of the five questions (Table 1). A questionnaire similar to the SCOFF was developed and validated for use in the U.S. This assessment tool is more detailed and includes 18 questions.53–55
Another study examined the responses of 126 girls between the ages of 12 and 17 to a questionnaire that also included the five SCOFF questions.56 The study sought to determine the awareness level of adolescent girls regarding eating disorders, and if they practiced behavior consistent with anorexia or bulimia. In addition, the investigators compared each study participant’s personal body image to her body mass index (BMI) percentile to determine if there was a disconnect between actual and perceived weight status. It was found that 18.25% of the participants answered “yes” to two or more of the SCOFF questions. This suggested that an eating disorder might exist. It was also discovered that those who were suspected of having an eating disorder had a much higher average BMI percentile (87.2%) versus those whose responses did not suggest they had an eating disorder (60.7%). When compared to the nonsuspect group, there was also a greater lack of awareness about eating disorders among subjects who were suspected of having an eating disorder.
These findings suggest it would be of value to ask all adolescent and young adults who display physical signs and symptoms of eating disorders to complete a weight/eating habits questionnaire. Determining patients’ BMI scores would provide additional information.57 If patients are younger than 18 and the results suggest they have, or are at risk of developing, an eating disorder, these findings should be discussed first with patients before involving parents or guardians. Should suspicions be confirmed, a referral to a physician or mental health professional is indicated for more extensive counseling. Issues associated with body image can be sensitive and require considerable tact in order not to shame or cause embarrassment. But oral health professionals can play a significant role in identifying individuals at risk, educating patients about the health consequences, and encouraging them to seek professional assistance.58 Dental offices should keep literature about eating disorders in their waiting rooms, along with information about local referral sources. Brochures are available from the National Eating Disorders Association (nationaleatingdisorders.org) and National Institute of Mental Health (nimh.nih.gov).
CONCLUSION
Early referral of patients with eating disorders to appropriate sources of care is critical. Comprehensive case management of patients with anorexia or bulimia requires a team of specialists, including physician and/or mental health professional, nutritionist and dentist and dental hygienist.11,59 Patients should be encouraged to rinse after each purge, but delay toothbrushing for several hours. The delay in brushing will reduce the loss of damaged tooth enamel rods and encourage tooth remineralization. Rinsing with a solution of water and sodium bicarbonate (baking soda) immediately after gastric purging will also help neutralize the vomited stomach contents.60 The daily use of a neutral sodium fluoride rinse or topical application of a neutral sodium fluoride gel in custom trays — in addition to using a fluoride toothpaste — can also help strengthen dental enamel.61
Oral health professionals must be able to recognize not only individuals with eating disorders, but also those who are at risk. An improved prognosis for recovery depends on early identification and intervention.11,62 Dental health professionals can play a pivotal role in the detection of early signs and symptoms of anorexia and bulimia, referral for treatment, and provision of patient-specific preventive oral health care.59,62,63
References
- Nicholls D, Viner R. Eating disorders and weight problems. BMJ. 2005;330:950–953.
- National Association of Anorexia Nervosa and Associated Disorders. About Eating Disorders: Statistics. Available at: anad.org/get-information/about-eatingdisorders/ eating-disorders-statistics/. Accessed November 5, 2015.
- Currin L, Schmidt U, Treasure J, Jick H. Time trends in eating disorder incidence. Br J Psychiatry. 2005;186:132–135.
- Kreipe RE, Birndorf SA. Eating disorders in adolescents and young adults. Med Clin North Am. 2000:84:1027–1049.
- Pritts SD, Susman J. Diagnosis of eating disorders in primary care. Am Fam Physician. 2003;67:297–304.
- National Association of Anorexia Nervosa and Associated Disorders. About Eating Disorders: Males & Eating Disorders. Available at: anad.org/getinformation/ males-eating-disorders/. Accessed November 5, 2015.
- National Eating Disorders Association. Get the Facts on Eating Disorders. Available at: nationaleating – disorders.org/get-facts-eating-disorders. Accessed November 5, 2015.
- National Alliance on Mental Health. Eating Disorders. Available at: http:// www .nami.org/Learn-More/Mental-Health- Conditions/Eating-Disorders. Accessed November 5, 2015.
- Herzog DB, Copeland PM. Eating disorders. N Engl J Med. 1985;313:295–303.
- NIMH. Eating Disorders. National Institute of Mental Health. Available at: nimh.nih.gov/ health/publications/eatingdisorders/ indes.shtml. Accessed November 5, 2015.
- Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, Va: American Psychiatric Association; 2013:338–350.
- Psychology Today. Anorexia symptoms — A Cognitive Behavioral Therapy Guide. Available at: psychology today.com/blog/inpractice/ 201301/ anorexia-symptomscognitive- behavioral-therapy-guide. Accessed November 5, 2015.
- Hsu LK. Epidemiology of the eating disorders. Psychiatr Clin North Am. 1996;19:681–700.
- Emans SJ. Eating disorders in adolescent girls. Pediatr Int. 2000;42:1–7.
- Lo Russo L, Campisi G, Di Fede O, Di Liberto C, Panzarella V, Lo Muzio L. Oral manifestations of eating disorders: a critical review. Oral Dis. 2008;14:479–484.
- Garner DM. Pathogenesis of anorexia nervosa. Lancet. 1993;341:1631–1635.
- Striegel-Moore RH, Dohm FA, Kraemer HC, et al. Eating disorders in white and black women. Am J Psychiatry. 2003;160:1326–1331.
- Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358.
- Alegria M, Woo M, Cao Z, Torres M, Meng XL, Striegel-Moore R. Prevalence and correlates of eating disorders in Latinos in the United States. Int J Eat Disord. 2007;40(Suppl):S15–S21.
- Anderson AE. Anorexia nervosa and bulimia in adolescent males. Pediatr Ann. 1984;13:901–904, 907.
- Crisp AH, Burns T, Bhat AV. Primary anorexia nervosa in the male and female: a comparison of clinical features and prognosis. Br J Med Psychol. 1986;59:123–132.
- American Academy of Pediatrics Committee on Sports Medicine and Fitness. Promotion of health weight-control practices in young athletes. Pediatrics. 1996:97:752–753.
- Touyz SW, Kopec-Schrader EM, Beumont PJ. Anorexia nervosa in males: a report of 12 cases. Aust NZ J Psychiatry. 1993;27:512–517.
- Eisenberg D, Nicklett EJ, Roeder K, Kirz NE. Eating disorder symptoms among college students: prevalence, persistence, correlates, and treatment-seeking. J Am Coll Health. 2011;59:700–707.
- Anorexia Nervosa and Related Eating Disorders. Statistics: How many people have eating disorders? Available at: anred.com/stats.html. Accessed November 5, 2015.
- Favaro A, Caregaro L, Tenconi E, Bosello R, Santonastaso P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J Clin Psychiatry. 2009;70:1715–1721.
- National Institute of Mental Health. Study Tracks Prevalence of Eating Disorders. Available at: nimh.nih.gov/ news/sciencenews/ 2007/study-tracks-prevalence-ofeating- disorders.shtml. Accessed November 5, 2015.
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A metaanalysis of 36 studies. Arch Gen Psychiatry. 2011;68:724–731.
- National Eating Disorders Association. Mortality and Eating Disorders. Available at: nationaleatingdisorders.org/mortality-andeating- disorders. Accessed November 5, 2015.
- Franko DL, Keel PK. Suicidality in eating disorders: occurrence, correlates, and clinical implications. Clin Psychol Rev. 2006;26:769–782.
- Piazza E, Piazza N, Rollins N. Anorexia nervosa: controversial aspects of therapy. Compr Psychiatry. 1980;21:177–189.
- Long TJ. Anorexia nervosa. Prim Care. 1987;14:177–201.
- Gottdiener JS, Gross HA, Henry WL, Borer JS, Ebert MH. Effects of self induced starvation on cardiac size and function in anorexia nervosa. Circulation.1978;58:425–433.
- Palmblad J, Fohlin L, Lundstrom M. Anorexia nervosa and polymorphonuclear (PMN) granulocyte reactions. Scand J Haematol. 1977;19:334–342.
- Eating Disorder Information — Prognosis. Available at: eating disorder information.org/prognosis.html. Accessed November 5, 2015.
- Sim LA, McAlpine DE, Grothe KB, Himes SM, Cockerill RG, Clark MM. Identification and treatment of eating disorders in the primary care setting. Mayo Clin Proc. 2010;85:746–751.
- WebMD. Bulimia Nervosa Health Center: Bulimia Nervosa — Cause. Available at: webmd.com/mental-health/ eatingdisorders/ bulimia-nervosa/bulimia-nervosacause. Accessed November 5, 2015.
- Mehler PS. Clinical practice. Bulimia nervosa. N Engl J Med. 2003;349:875–881.
- Johnson C. Initial consultation for patients with bulimia and anorexia nervosa. In Garner DM, Garfinkel PE, eds. Handbook of Psychotherapy for Anorexia Nervosa and Bulimia. New York: Guilford Press; 1984:19–51.
- Johnson GL, Humphries LL, Shirley PB, Mazzoleni A, Noonan JA. Mitral valve prolapsed in patients with anorexia nervosa and bulimia. Arch Intern Med. 1986;146:1525–1529.
- Crow SJ, Peterson CB, Swanson SA, et al. Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry. 2009;166:1342–1346.
- National Eating Disorders Association. Dental Complications of Eating Sisorders. Available at: nationaleating disorders.org/ dental-complications-eating-disorders. Accessed November 5, 2015.
- Lo Russo L, Campisi G, Di Fede O, Di Liberto C, Panzarella V, Lo Muzio L. Oral manifestations of eating disorders: a critical review. Oral Dis. 2008;14:479–484.
- Frydrych AM, Davies GR, McDermott BM. Eating disorders and oral health: a review of the literature. Aust Dent J. 2005;50:6–15.
- Yagi T, Ueda H, Amitani H, Asakawa A, Miyawaki S, Inui A. The role of gherlin, salivary secretions, and dental care in eating disorders. Nutrients. 2012;4:967–989.
- Coleman H, Altini M, Nayler S, Richards A. Sialadenosis: a presenting sign in bulimia. Head Neck. 1998;20:758–762.
- Brady JP. Parotid enlargement in bulimia. J Fam Pract. 1985;20:496–502.
- Carni JD. The teeth may tell: Dealing with eating disorders in the dentist’s office. J Mass Dent Soc. 1981;30:80–86.
- Lamey PJ, Lamb AB. Prospective study of aetiological factors in burning mouth syndrome. Br Med J (Clin Res Ed). 1988:296:1243–1246.
- DeBate RD, Tedesco LA. Increasing dentists’ capacity for secondary prevention of eating disorders: identification of training, network, and professional contingencies. J Dent Educ. 2006;70: 1066–1075.
- DeBate RD, Tedesco LA, Kerschbaum WE. Knowledge of oral and physical manifestations of anorexia and bulimia nervosa among dentists and dental hygienists. J Dent Educ. 2005;69:346–354.
- Luck AJ, Morgan JF, Reid F, et al. The SCOFF questionnaire and clinical interview for eating disorders in general practice: comparative study. BMJ. 2002;325:755–756.
- Mond JM, Myers TC, Crosby RD, et al. Screening for eating disorders in primary care: EDE-Q versus SCOFF. Behav Res Ther. 2008;46:612–622.
- Perry L, Morgan J, Reid F, et al. Screening for symptoms of eating disorders: reliability of the SCOFF screening tool with written compared to oral delivery. Int J Eat Disord. 2002;32:466–472.
- Parker SC, Lyons J, Bonner J. Eating disorders in graduate students: exploring the SCOFF questionnaire as a simple screening tool. J Am Coll Health. 2005;54:103–107.
- Hicks TM, Lee JY, Nguyen T, La Via M, Roberts MW. Knowledge and practice of eating disorders among a group of adolescent dental patients. J Clin Pediatr Dent. 2013;38:39–43.
- Martin JB. The development of ideal body image perceptions in the United States. Nutrition Today. 2010;45(3):111–112.
- Burkhart N, Roberts M, Alexander M, Dodds A. Communicating effectively with patients suspected of having bulimia nervosa. J Am Dent Assoc. 2005;136;1130–1137.
- Milosevic A. Eating disorders and the dentist. Br Dent J. 1999;186:109–113.
- Wolcott RB, Yager J, Gordon G. Dental sequel to the binge-purge syndrome (bulimia): Report of cases. J Am Dent Assoc. 1984;109:723–725.
- American Academy of Pediatric Dentistry. Reference Manual. Pediatr Dent. 2013;35:43–44, 167–170.
- Old Dominion University. Dental Health Professionals and Secondary Prevention of Eating Disorders. Available at: odu.edu/ ao/ instadv/ quest/EatingDisorders.html. Accessed November 5, 2015.
- American Academy of Pediatric Dentistry. Reference Manual. Pediatr Dent. 2013;35:45–47,171–174.