Mitigate the Risk of On-the-Job Exposure
Oral health professionals should be knowledgeable about disease transmission and the risk of bloodborne pathogens to minimize occupational exposures
This course was published in the June 2023 issue and expires June 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 148
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of human immunodeficiency virus and hepatitis B and C virus infections.
- Discuss the keys to preventing bloodborne infection.
- Explain strategies for managing occupational exposures and follow-up care.
The United States Centers for Disease Control and Prevention (CDC) estimates that 1.2 million people in the United States are infected with the human immunodeficiency virus (HIV), with 50,000 new cases diagnosed annually. Additionally, the CDC reports approximately 200,000 new cases of hepatitis C virus (HCV) and 21,000 new cases of hepatitis B virus (HBV) each year in the US, although these numbers are likely low due to under-reporting.1–3
Oral health professionals are at risk for these infections due to potential exposure to contaminated blood while providing patient care. Unlike HBV, vaccination against HIV and HCV is not possible. Therefore, healthcare workers are required to use universal precautions with all patients, even when a patient’s status is unknown.
Despite strict adherence to universal precautions, occupational exposures via needlesticks, surgical instruments, fragmented teeth, or splash injuries are still possible. Knowledge of what constitutes an occupational exposure and the appropriate actions to minimize infection risk is key. Occupational exposures should be treated as emergencies with timely post-exposure consultation, management, and treatment, which may include the HBV vaccine, HBV immune globulin, and/or post-exposure prophylaxis for HIV.2,3
Dental practices should identify a local infectious disease expert who can facilitate prompt assessment and administration of necessary medical and pharmacologic care. Dental professionals should also be aware of the National Clinicians’ Post-Exposure Hotline — 888-448-4911 — which is endorsed by the CDC and operational 24/7.
While US data regarding occupational exposures among nurses and physicians are available in the medical literature, comparative data for dental professionals are scarce.4–8 However, as of 2011, the CDC has reported 57 cases of known HIV infection acquired through occupational exposures, with another 143 possible infections among healthcare workers.
The most effective way to prevent infection with bloodborne pathogens is to avoid injuries and consistently use personal protective equipment. The CDC has identified specific injuries that pose a threat to healthcare workers, including percutaneous injuries (needlestick or laceration caused by a sharp object), exposure of highly vascularized mucous membranes to infected blood, and contact of blood with compromised skin (eg, dermatitis, abrasions, or burns).9
Risks for Oral Health Professionals
Dental professionals are at risk of occupational exposures through instruments used in patient care, such as hollow-bore and solid needles, burs, scalpels, scalers, surgical elevators, explorers, solid needles, and orthodontic wires.6,8–10
In a 2018 meta-analysis of 55 studies on dental professionals, burs were responsible for the highest number of percutaneous injuries.8 The prevalence of occupational exposures among dental specialists ranged from 7.8% to 89.17%, with orthodontists experiencing the lowest prevalence and endodontists having the highest
Ensuring safety in professional practice requires maintaining accurate medical records for all patients in a dental practice. This is crucial in identifying any communicable diseases before dental work is performed. Universal precautions should be strictly followed, ensuring that the presence of a communicable disease does not affect the point-of-care experience but rather informs the clinician about necessary care in the event of an occupational exposure.
Type of Infections
HBV is more easily transmitted than HIV and HCV, and it can lead to serious complications such as cirrhosis and hepatocellular carcinoma. Vaccination against HBV is recommended for dental professionals.
The rate of transmission is highest when the source patient tests positive for both the hepatitis B surface antigen and the hepatitis B e antigen.11 HBV can remain viable on inanimate objects for more than 7 days, and transmission can occur even when no blood is visible.11,12
Oral health professionals who do not develop immunity despite receiving the complete three-dose vaccine series may be given a fourth dose of the vaccine or a second three-dose series at a higher dosage.13 If the additional vaccination does not establish immunity, individuals are identified as “non-responders” and remain susceptible to HBV infection. These individuals should know they are candidates for hepatitis B immune globulin and/or a repeat vaccination series in the event of an occupational exposure. It is important for these individuals to identify a medical provider in advance of an occupational exposure with whom they can consult in the event of an injury. Having this preemptive plan in place will facilitate timely assessment and administration of hepatitis B immune globulin when indicated. According to the CDC, hepatitis B immune globulin should be administered within 24 hours post-exposure.11
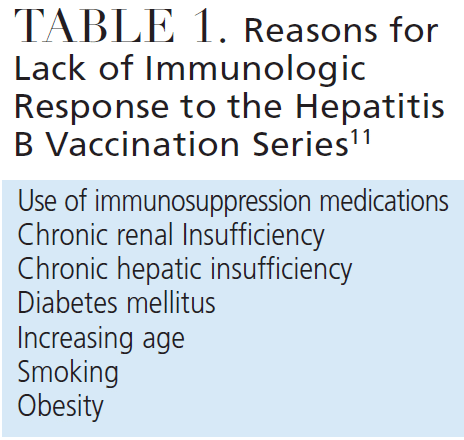
For these reasons, dental professionals must be aware of the potential risk of acquiring HBV during their professional work. Clinicians must also understand their own HBV immunity. The HBV vaccine became available in 1982 and was added to routine vaccination schedules in the 1990s, resulting in widespread immunity among the general population. The standard vaccination procedure involves a series of three doses that can provide lifelong immunity.13 However, approximately 5% of vaccinated individuals never develop immunity despite completing the entire vaccination series. The lack of immunity is likely multifactorial, with many cases attributed to chronic disease and/or the use of immunomodulating medications.13 Table 1 outlines conditions that may impair the immune system, thereby preventing the production of sufficient antibodies to provide immunity against HBV.11,12
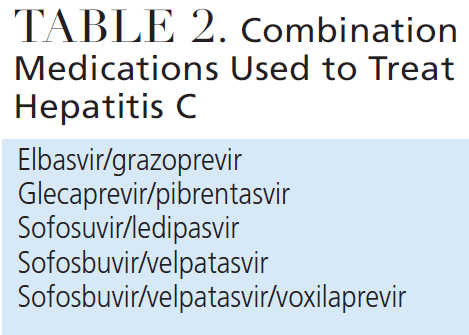
Currently, more than 2 million people in the US have HCV.2 However, the risk of transmission following an occupational exposure from patients with HCV is relatively low, ranging from 0.1% to 2%.2,14,15 Since 2014, combination antiviral treatments have become available for individuals with HCV (Table 2). These medications offer curative treatment for most patients; however, their high cost makes them inaccessible for many, leading to continued transmission of the virus.
In the US, more than 1 million people are living with HIV, which can is now managed as a chronic illness. HIV is a retrovirus, and a combination of medications can be used to interfere with viral replication at different stages of the process. When taken as prescribed, current antiretroviral medications can effectively suppress the virus to undetectable levels in the majority of patients.
For patients with HIV, it is crucial to document their most recent viral load and current medication regimen. If a patient has documented resistance to any antiretroviral medications, they should not be used for any future post-exposure prophylaxis for the clinician.
Patients co-infected with HIV and HBV should be noted, particularly if the dental professional is susceptible to HBV. In the event of an exposure during patient care, the co-infection status of the source patient will impact the selection of prophylactic medications that can protect against both viruses.
If a clinician experiences an exposure and the HIV status of the patient is unknown, both individuals should undergo testing, preferably using a rapid HIV-antibody test. Studies indicate that the risk of acquiring HIV following an occupational exposure is low, approximately 0.3% for a percutaneous exposure to HIV-positive blood and 0.09% for a splash injury involving HIV-infected blood.9
Currently, more than 30 antiretroviral medications are available to treat HIV, which can be classified into six groups. The appropriate selection of a medication regimen — which may include nucleoside reverse transcriptase inhibitors, non-nucleoside reverse transcriptase inhibitors, protease inhibitors, fusion inhibitors, integrase strand transfer inhibitors, and CCR5 coreceptor antagonists — following an exposure requires knowledge of the different classes. Due to the possibility of resistance, these medications should only be prescribed by infectious disease specialists or clinicians who have experience in prescribing antiretroviral medications for at least 100 patients with HIV.
After an exposure, clinicians should seek professional help if they experience symptoms of anxiety and/or depression, as occupational exposures can significantly impact mental health.16
Managing Occupational Exposure
Occupational exposures to HIV, HBV, and HCV can occur through needlesticks or lacerations from sharp instruments contaminated with the blood of an infected patient, saliva containing blood, or splash injuries to mucous membranes or nonintact skin. The risk of disease transmission following an occupational exposure depends on factors such as the amount of free virus in the source patient’s blood, the amount of blood involved in the injury, the type of injury, and the severity of a penetrating injury.9,11
When dental professionals experience an exposure to a bloodborne pathogen, the CDC recommends the following steps:
- Wash the site of the needlestick or laceration. Cleaning the area with regular soap and water is advised. The use of chlorhexidine 2% solution or chlorhexidine gluconate 4% solution has not shown superiority to soap and water, but it is also not contraindicated. The CDC does not recommend using caustic agents such as bleach.2
- Flush and irrigate areas where splash injuries occurred. If a splash injury occurs, clinicians should generously flush and irrigate the specific body area with water. For injuries involving the mouth, nose, or intact skin, thorough flushing and irrigation are recommended.
- Irrigate the eyes with clean water, saline, or sterile irrigants. In the case of a splash injury involving the eyes, clinicians should generously irrigate the eyes using an agent that does not cause irritation.
- Document the exposure/injury. Dental professionals should be familiar with the procedures for reporting incidents and exposures to the individual responsible for managing and documenting exposures in the dental practice. Documentation should include the exact time of the injury, location of the injury, type of injury, and how it occurred. This information is crucial not only for immediate response but also for developing strategies to prevent similar injuries in the future. Additionally, all suspected occupationally acquired infections must be reported to state health departments.
Following an occupational exposure, dental professionals may experience various emotions, including panic. Not only should the immediate emotional response be considered, but also the potential emotional impact in the weeks and months after the injury. The medical literature has reported increased rates of anxiety and/or depression among healthcare providers who have experienced occupational exposures.16
Ensuring patient safety is paramount, especially if the exposure requires the dental professional to temporarily leave the patient-care environment. The patient should be informed about the injury and another colleague may need to complete the visit or procedure. The patient is now considered the “source patient” and may be asked to undergo testing for communicable diseases, particularly if the hepatitis and HIV status is unknown and the exposure/injury was significant.
Selecting Post-exposure Prophylaxis Medications
Selecting an appropriate regimen of antiretroviral medications for post-exposure prophylaxis is a complex task that should not be undertaken by dental professionals themselves, even if there is a desire to initiate treatment. Typically, a regimen consists of three medications from at least two classes. The preferred regimen for post-exposure prophylaxis includes raltegravir and a combination of tenofovir/emtricitabine. When determining the optimal regimen, the prescriber will consider the medical history of the exposed clinician and review all existing medications to minimize potential adverse drug interactions.
Certain antiretrovirals should be avoided in patients with renal insufficiency (eg, elvitegravir and tenofovir), while caution should be exercised when administering atazanavir with H2 antagonists and proton pump inhibitors due to potential drug interactions. Atazanavir can also cause PR interval prolongation, so it should be used with caution in patients with cardiac conduction disorders. Darunavir may cause hepatotoxicity, and the use of abacavir requires HLA testing before initiation, which may not be practical in the context of post-exposure prophylaxis. These medication profiles highlight the complexity of their use and underscore the need for extensive pharmacologic knowledge of antiretroviral medications when selecting an appropriate regimen.
The prescriber should also consider the pill burden and side effect profiles of the antiretroviral medications, as well as the dosing schedule of the post-exposure regimen. Compliance may be affected by the dosing schedule, and it is important to consider how it may interfere with the daily activities of the exposed clinician. Alternative regimens may be available based on prior resistance testing of the source patient. All antiretroviral medications have side effects, and since post-exposure prophylaxis is prescribed for 4 weeks, a regimen with tolerable side effects should be chosen. In some cases, additional prescription medications, such as antiemetics and antispasmodics, may be necessary to alleviate the side effects of antiretrovirals.
Ideally, a serious occupational exposure should be managed by an infectious disease expert who can address the side effects of the prescribed medications. If an infectious disease expert is not available, an emergency medicine or family medicine provider can prescribe appropriate prophylactic medications under the guidance of experts at the National Clinicians Post-Exposure Hotline. It is important not to delay prophylactic treatment while awaiting evaluation by an infectious disease specialist.
Post-Exposure Follow-Up Care
After an occupational exposure, the exposed clinician will undergo HIV and hepatitis testing at specific intervals. HIV testing is conducted at 6 weeks, 12 weeks, and 4 to 6 months after the exposure. The screening involves a fourth generation enzyme-linked immunosorbent assay (ELISA) test, which simultaneously detects the HIV p24 antigen and antibodies to HIV. The advantage of using a 4th generation ELISA is that it eliminates the need for confirmatory Western blot testing, which was required with earlier generation ELISA tests. Additionally, the use of a fourth generation ELISA allows for follow-up testing to be completed within 4 months instead of the previous 6-month period.
During the follow-up period, counseling and education for the exposed clinician will emphasize the importance of engaging in safe sexual activities. The clinician must also be advised to refrain from donating blood, plasma, or semen. Strict adherence to the prescribed antiretroviral medication regimen is crucial during this time to minimize the risk of viral transmission. If the clinician consistently tests negative for HIV throughout the observation period, no further antiretroviral medications are necessary beyond the initial 4-week prophylaxis.
If the source patient’s HIV and hepatitis status is unknown at the time of the exposure and the source patient undergoes testing that returns negative results for HIV and hepatitis, the prophylaxis can be discontinued before the completion of the 4-week regimen.
Special circumstances may impact the counseling and education provided during the follow-up period. For instance, if a dental professional is lactating at the time of a significant exposure, she will be advised to discontinue breastfeeding due to the potential risk of transmitting HIV to her child if she becomes infected. Similarly, individuals taking prophylactic medications for HIV should delay attempts to conceive by avoiding unprotected intercourse.
Conclusion
Oral health professionals should be knowledgeable about disease transmission and the risk of bloodborne pathogens to minimize occupational exposures. Although transmission of HIV and hepatitis following occupational exposures is rare, oral health professionals must continue working diligently to reduce their risk. Continued education in this area is warranted, as evidence suggests that healthcare workers tend to under-report percutaneous injuries.17
References
- Schillie S, Webster C, Osborne M, Wesolowski L, Ryerson AB. CDC recommendations for hepatitis C screening among adults – United States, 2020. MMWR Recomm Rep. 2020;69:1–17.
- Schillie S, Vellozzi C, Reingold A, et al. Prevention of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2018;67(No. RR-1):1–31.
- United States Centers for Disease Control and Prevention. Updated US public health service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001;50(RR-11):1-52.
- Wyżgowski P, Rosiek A, Grzela T, Leksowski K. Occupational HIV risk for health care workers: risk factor and the risk of infection in the course of professional activities. Ther Clin Risk Manag. 2016;12:989–994.
- Panlilio A, Orelien J, Srivastava P, Jagger J, Cohn R, Cardo D. Estimate of the annual number of percutaneous injuries among hospital-based healthcare workers in the United States 1997-1998. Infect Control Hosp Epidemiol. 2004;25:556–562.
- Shah SM, Merchant AT, Dosman JA. Percutaneous injuries among dental professionals in Washington State. BMC Public Health. 2006;6:269.
- Sofola OO, Folayan MO, Denloye OO, Okeigbemen SA. Occupational exposure to bloodborne pathogens and management of exposure incidents in Nigerian dental schools. J Dent Educ. 2007;71:832–837.
- Pereira MC, Mello FW, Ribeiro DM, et al. Prevalence of reported percutaneous injuries on dentists: A meta-analysis. J Dent. 2018;76:9-18.
- United States Centers for Disease Control and Prevention. Public Health Service guidelines for the management of healthcare worker exposures to HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001;50(RR-11):1–52.
- Cleveland J, Barker L, Gooch B, Bertrami E, Cardo D. Use of HIV postexposure prophylaxis by dental health care personnel: An overview and update recommendations. J Am Dent Assoc. 2002;133:1619–1626.
- United States Centers for Disease Control and Prevention. Guidance for evaluating healthcare personnel for hepatitis b virus protection and for administering postexposure management. MMWR Recomm Rep. 2013;62(RR-10):1–19.
- Denault D, Gardner H. OSHA Bloodborne Pathogen Standards. Available at: ncbi.nlm.nih.gov/books/NBK570561. Accessed May 17, 2023.
- Walayat S, Ahmed Z, Martin D, Puli S, Cashman M, Dhillon S. Recent advances in vaccination of non-responders to standard dose hepatitis B virus vaccine. World J Hepatol. 2015;7:2503–2509.
- Alter MJ. HCV routes of transmission: what goes around comes around. Semin Liver Dis. 2011;31:340–346.
- Egro FM, Nwaiwu CA, Smith S, Harper JD, Spiess AM. Seroconversion rates among health care workers exposed to hepatitis C virus-contaminated body fluids: The University of Pittsburgh 13-year experience. Am J Infect Control. 2017;45:1001–1005.
- Wald J. The psychological consequence of occupational blood and body fluid exposure injuries. Disabil Rehabil. 2009;31:1963–1969.
- Joshi NV, Joshi M, Rathod V, Langde D. Occupational exposures to bloodborne pathogens and its underreporting in dental teaching environment in an Indian dental school. Indian J Dent Res. 2021;32:305–309.
From Decisions in Dentistry. June 2023;9(6):32-35.




