
Clinical Approaches to Treating Children With Autism
A variety of strategies can be employed to successfully treat this patient population.
The authors have no commercial conflicts of interest to disclose.
This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of autism spectrum disorder (ASD).
- Discuss how to prepare for the safe and effective treatment of children with ASD.
- List the supportive accommodations that promote successful dental care for children with autism.
- Integrate adjunctive hygiene measures in self-care regimens.
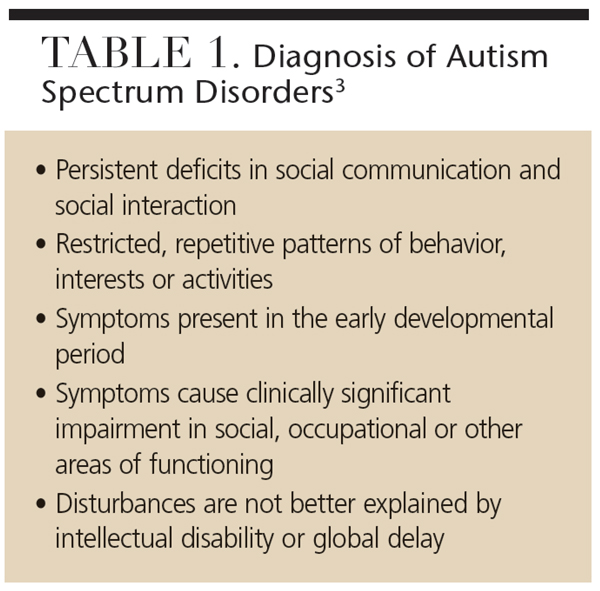
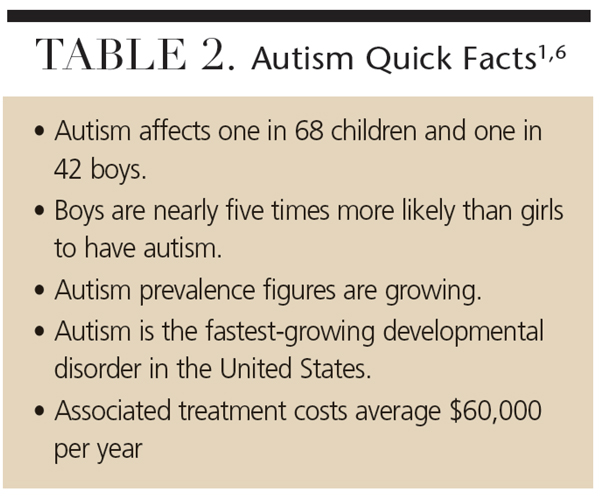
More than 700,000 children have been diagnosed with autism spectrum disorder (ASD) in the United States. Approximately one in 68 children has ASD,1 making autism the most common developmental disorder in this country. As a spectrum disorder, affected individuals display a variety of symptoms and levels of severity.2 The most recent definition for ASD published in the American Psychological Association’s Diagnostic and Statistical Manual states that impairment in social communication and restricted/repetitive interests and behaviors are the hallmarks of ASD (Table 1).3 Approximately 70% of children with autism have some speech ability, with more than 20% attaining fluency.4 Similarly, although most children with ASD continue living at home in adulthood, roughly one in 10 may grow up to live and work on their own (Table 2).1,5,6
With such a high prevalence rate, dentists will most likely encounter patients with autism.2 Children with autism are at particular risk for oral health problems, as up to 15% are not receiving dental care.7,8 This is partially because unusual behaviors and heightened sensory sensitivities can make clinical interactions difficult. Communication irregularities can also interfere with care delivery. Although these barriers can pose a challenge, treating children with ASD can be a manageable and enjoyable part of dental practice.
For a child with autism, dental visits can be overwhelming. Dental chairs that change positions, bright overhead lights, shiny instruments and facial contact can seem scary and unusual. Not knowing how the child will react can be very stressful for parents/caregivers. In fact, it is not unusual for parents/caregivers to simply avoid taking the child to the dentist because they are worried the experience will be negative, or they have already had a failure at other medical and dental offices.9
SUCCESSFUL FIRST VISIT
Practitioners can work with parents/caregivers to make the first visit pleasant. The parent/caregiver and child should not feel pressured to accomplish treatment on the initial visit. Rather, it should provide an opportunity for the child to see the office and meet the staff. In many cases, when the child returns for subsequent visits, the fear of the unknown will be greatly diminished.
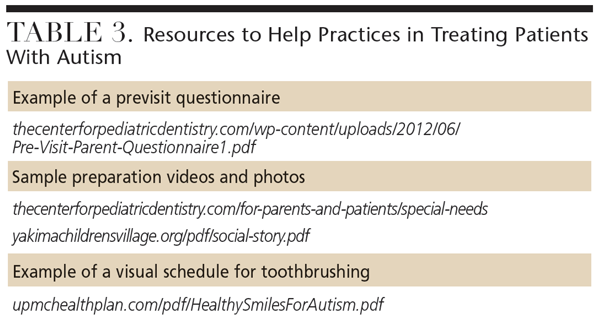
 Likewise, the provider should take this opportunity to learn as much as possible about the patient. A previsit questionnaire is a simple way to accomplish this (Table 3). This gives parents/caregivers a chance to provide helpful information, such as the child’s use and understanding of language, strengths and interests, and possible behavioral triggers. Including a section about the child’s previous history with dental treatment is also important, as this will allow the team to adopt approaches that have proven successful for the child. It will also help clinicians avoid stressors that could stimulate the fight-or-flight response. The previsit questionnaire also allows parents/caregivers to voice their concerns and offer information they think will be helpful.10 Nobody knows the child better than his or her parents/caregivers. As such, they can be very effective in interpreting the child’s unique behaviors.
Likewise, the provider should take this opportunity to learn as much as possible about the patient. A previsit questionnaire is a simple way to accomplish this (Table 3). This gives parents/caregivers a chance to provide helpful information, such as the child’s use and understanding of language, strengths and interests, and possible behavioral triggers. Including a section about the child’s previous history with dental treatment is also important, as this will allow the team to adopt approaches that have proven successful for the child. It will also help clinicians avoid stressors that could stimulate the fight-or-flight response. The previsit questionnaire also allows parents/caregivers to voice their concerns and offer information they think will be helpful.10 Nobody knows the child better than his or her parents/caregivers. As such, they can be very effective in interpreting the child’s unique behaviors.
When working with children who have ASD, it can be easy to focus on their limitations. Instead, try to capitalize on their strengths. If the child is very visual, for example, providing photos or a video of the office before the visit can be helpful (Table 3).11 These types of preparation aids are referred to as social stories, visual schedules or storyboards.12,13 When creating a preparation aid, the child’s preferred media format should be considered. Some children will respond best if the aid is displayed on a tablet, while others might do better with a printed version. Some families develop preparation aids on their own, but it can be helpful to develop an office-specific aid that can be hosted on the practice’s website.
Many children with autism prefer established routines.14 Preparing at home helps children develop a dental routine that can be followed when they arrive at the office. Providing the family with a practice dental kit that may include exam gloves, gauze and a plastic dental mirror is an effective strategy to facilitate this routine and increase compliance with the dental exam. Parents/caregivers should first establish a routine of brushing at home. Once established, the dental mirror can be introduced during this routine. Children then become accustomed to having items other than the toothbrush placed in their mouths. When they arrive at the dental office, parents/caregivers can demonstrate the home brushing technique and how they used the dental mirror. It is then easier for the dentist to replicate the same toothbrushing technique and mirror examination.
ACCOMMODATE THE CHILD
 Making accommodations to put the child at ease sets the stage for success. Families should be asked to bring the child’s favorite comfort objects to dental visits. Parents/caregivers might also consider bringing another adult who the child loves and trusts. Another adult can be helpful in keeping the child occupied, listening to information from the provider, or simply lending moral support.
Making accommodations to put the child at ease sets the stage for success. Families should be asked to bring the child’s favorite comfort objects to dental visits. Parents/caregivers might also consider bringing another adult who the child loves and trusts. Another adult can be helpful in keeping the child occupied, listening to information from the provider, or simply lending moral support.
Bringing additional help can be particularly useful if the child arrives early and needs to wait for an extended period. While every attempt should be made to seat the child on time, this is not always possible.15 It is important to determine the best location to wait. Some children will easily find ways to entertain themselves in a reception area, but others may be more at ease waiting in the car or taking a walk outside. Consideration should also be given to the examination area. Many children with ASD will do best, particularly for the initial visits, if they are scheduled in a private room.
Some patients will adapt easily to the dental routine, becoming comfortable with the office and dental team within the first few visits. Research indicates that up to half of children with ASD might fall into this category.16–20 Others may not accept dental care as readily. These children may benefit from applied behavioral analysis therapy, which focuses on desensitization and reinforcing desired behaviors and modifying undesirable ones.21,22 Many children with ASD are already enrolled in these types of therapies. Dentists should ask parents/caregivers about strategies that have been successful in the past so clinicians know what rewards will be most effective and how often skills might be practiced.23 While a customized approach works best, the following type of program may work well for many patients:
First visit: The aim is to meet and greet the dental staff. Clinicians should review the previsit questionnaire with parents/caregivers, discuss preparation aids and provide a practice exam kit. An attempt should be made to have the child sit in a dental chair. It’s advisable to take a photograph that can be viewed at home.
Second visit: The child may sit in the dental chair while the parent/caregiver demonstrates brushing technique and the use of the dental mirror. The provider can then replicate the technique.
Third and subsequent visits: Clinicians and patients should repeat the skills learned at last visit, while adding new skills.
 It is important to introduce a new item or skill and then pause to give the child time to digest what has happened. In most circumstances, it is best to begin slowly and wait for the child to decide whether he or she will allow the next step. One technique is to first use an object such as a dental mirror to count the clinician’s gloved fingers. The child is then asked to have his or her fingers counted. Once the child is comfortable with the counting routine, the object can be moved to his or her lips or open mouth for the same count. Soon, the clinician has established a rapport with the patient and the child has learned a new skill. It is extremely helpful to maintain the routine for all visits, including using the same order of procedures, the same operatory and the same staff.
It is important to introduce a new item or skill and then pause to give the child time to digest what has happened. In most circumstances, it is best to begin slowly and wait for the child to decide whether he or she will allow the next step. One technique is to first use an object such as a dental mirror to count the clinician’s gloved fingers. The child is then asked to have his or her fingers counted. Once the child is comfortable with the counting routine, the object can be moved to his or her lips or open mouth for the same count. Soon, the clinician has established a rapport with the patient and the child has learned a new skill. It is extremely helpful to maintain the routine for all visits, including using the same order of procedures, the same operatory and the same staff.
Children who are profoundly impaired or who cannot regularly make office visits may need advanced behavior guidance, such as protective stabilization, sedation or general anesthesia to receive care. If an office does not provide these services, a referral to a specialist or a hospital-based or university-based program is best.
For children with ASD, cooperation is often facilitated by clinicians who exude a calm energy, move at a steady pace and communicate effectively. Using short, simple sentences is advisable, as this will allow the child to absorb key messages. It is also important to avoid sarcasm, metaphor and jargon, as patients with ASD tend to be very literal.24 Telling the patient to “hop up in the seat,” for instance, may lead to bounding into the dental chair. Perhaps most important is a clinician’s ability to be creative and maintain a sense of humor.
Children with ASD may have sensory processing differences. If so, determining whether the child is a hyporesponder who seeks sensory input, or a hyperresponder who avoids sensory input, is helpful.25 Children who seek sensory input can be accommodated by applying deep pressure with a weighted blanket or X-ray vest, allowing the patient to view dental procedures using a handheld mirror, and encouraging the child to squeeze toys during the visit. Children who avoid sensory input can be supported by minimizing noises, using unscented and unflavored products, placing dark glasses over their eyes to block light, and reclining the dental chair in advance to minimize motion.14,26,27
MAINTAIN PATIENTS’ ORAL HEALTH
Regular oral surveillance is critical to maintaining the dental health of children with ASD. Otherwise, caries can go undocumented and unchecked, causing pain that children may be unable to communicate to parents/caregivers. In turn, pain from oral health conditions can contribute to negative behaviors, sleeping difficulties and learning problems.28,29 These risks can be minimized by establishing a routine of professional examination and preventive care.
Children with ASD typically have poorer oral hygiene than their peers, which may be complicated by sensory sensitivity experienced when brushing.30,31 Dental professionals can encourage good brushing habits by asking a few important questions:
- Has the family tried both power and manual toothbrushes? Some children with ASD respond favorably to vibrations from power brushes, while others find them disconcerting. A multi-angled toothbrush can be helpful when parents/caregivers have limited time to help children brush.
- Does the child have a difficult time with the flavor of the toothpaste being used? If so, other toothpastes should be tried; alternately, parents/caregivers can dip the brush in a fluoride mouthrinse. This won’t provide the same preventive effects as toothpaste, but it is better than not receiving any topical fluoride exposure at all.
- Does the child like numbers or timers? Brushing can sometimes be facilitated by using a timer. A standard hourglass or egg timer may work well for some children, while others may prefer a digital version. Novel toothbrush apps are also available online to encourage proper brushing.
- Does the child like music? Some toothbrushes play two minutes of music to motivate the child to brush for the appropriate period.
- Does the child use visual schedules? If so, cards or visual schedules can be created for toothbrushing (Table 3).
- Where does the family usually brush the child’s teeth? For children who do not want to use the bathroom, brushing their teeth in the family room, while lying on the ground, or even in their beds may prove successful.
Clinicians should also inquire about the child’s diet. Pediatric patients with ASD may eat only a small number of preferred foods (e.g., certain tastes, textures or colors) or follow a restricted diet (e.g., a gluten-free/casein-free diet). This may mean the child frequently consumes foods that are damaging to dentition. While it is unlikely that the child’s preferences will be easily altered, parents/caregivers can be encouraged to limit the frequency of snacks. Another challenge arises during behavioral therapy when the child is receiving food rewards, such as candy. Therapy typically lasts for several hours each day, and rewarding positive behavior with sweets raises caries risk. Food is a powerful primary reinforcer, and it can be challenging to break from this habit. For situations in which this is not feasible, sugar-free candies are a viable alternative. Given the increased prevalence and availability of technology, allowing screen time on a tablet may be an alternative to food-based rewards for some children.
CONCLUSION
Providing dental care for children with ASD can be both a challenging and rewarding experience. By taking the time to work with families, oral health professionals not only provide needed dental services, but also contribute to the child’s ability to receive dental care and achieve a lifetime of oral health.
References
- Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators; Centers for Disease Control and Prevention. Prevalence of autism spectrum disorder among children aged 8 years — autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014;63:1–21.
- Centers for Disease Control and Prevention. Facts About Autism Spectrum Disorder. Available at: cdc.gov/ncbddd/autism/facts.html. Accessed November 30, 2015.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, Virginia: American Psychiatric Publishing; 2013.
- Anderson DK, Lord C, Risi S, et al. Patterns of growth in verbal abilities among children with autism spectrum disorder. J Consult Clin Psychol. 2007;75:594–604.
- Anderson KA, Shattuck PT, Cooper BP, Roux AM, Wagner M. Prevalence and correlates of postsecondary residential status among young adults with an autism spectrum disorder. Autism. 2014;18:562–570.
- Autism Speaks. What Is Autism? Available at: autismspeaks.org/what-autism. Accessed November 30, 2015.
- Lai B, Milano M, Roberts MW, Hooper SR. Unmet dental needs and barriers to dental care among children with autism spectrum disorders. J Autism Dev Disord. 2012;42:1294–1303.
- Lewis CW. Dental care and children with special health care needs: a population-based perspective. Acad Pediatr. 2009;9:420–426.
- Nelson LP, Getzin A, Graham D, et al. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent. 2011;33:29–36.
- Nelson TM, Sheller B, Friedman CS, Bernier R. Educational and therapeutic behavioral approaches to providing dental care for patients with autism spectrum disorder. Spec Care Dentist. 2015;35:105–113.
- Backman B, Pilebro C. Visual pedagogy in dentistry for children with autism. ASDC J Dent Child. 1999;66:294,325–331.
- Gray C. Social Stories 10.0: The new defining criteria. Available at: cp.iqnection.com/cms/downloadfile.php?file_id=141472. Accessed November 30, 2015.
- Gray C. Social Stories and Comic Strip Conversations With Students With Asperger Syndrome and High-Functioning Autism. New York: Plenium; 1998.
- Kuhaneck HM, Chisholm EC. Improving dental visits for individuals with autism spectrum disorders through an understanding of sensory processing. Spec Care Dentist. 2012;32:229–233.
- Raposa KA. Behavioral management for patients with intellectual and developmental disorders. Dent Clin North Am. 2009;53:359–373.
- Marshall J, Sheller B, Williams B, Mancl L, Cowen C. Cooperation predictors for dental patients with autism. Pediatr Dent. 2007;29:369–376.
- Loo C, Graham R, Hughes C. Behaviour guidance in dental treatment of patients with autism spectrum disorder. Int J Paediatr Dent. 2009;19:390–398.
- Klein U, Nowak AJ. Characteristics of patients with autistic disorder (AD) presenting for dental treatment: a survey and chart review. Spec Care Dentist. 1999;19:200–207.
- Lowe O, Lindemann R. Assessment of the autistic patient’s dental needs and ability to undergo dental examination. ASDC J Dent Child. 1985;52:29–35.
- DeMattei R, Cuvo A, Maurizio S. Oral assessment of children with an autism spectrum disorder. J Dent Hyg. 2007;81:65.
- Connick C, Pugliese S, Willette J, Palat M. Desensitization: strengths and limitations of its use in dentistry for the patient with severe and profound mental retardation. ASDC J Dent Child. 2000;67:250-255.
- The Nancy Lurie Marks Family Foundation. D-Termined Program of Repetitive Tasking and Familiarization in Dentistry. Available at: nlmfoundation.org/media/dental_clips.htm. Accessed November 30, 2015
- Maguire K, Lange B, Sherling M, Grow R. The use of rehearsal and positive reinforcement in the dental treatment of uncooperative patients with mental retardation. Journal of Developmental and Physical Disabilities. 1996;8:167–177.
- Green D, Flanagan D. Understanding the autistic dental patient. Gen Dent. 2008;56:167–171.
- Stein LI, Polido JC, Cermak SA. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr Dent. 2013;35:230–235.
- Marshall J, Sheller B, Mancl L, Williams B. Parental attitudes regarding behavior guidance of dental patients with autism. Pediatr Dent. 2008;30:400–407.
- Luscre D, Center D. Procedures for reducing dental fear in children with autism. J Aut Dev Disord. 1996;26:547–556.
- Edelstein B, Vargas C, Candelaria D, Vemuri M. Experience and policy implications of children presenting with dental emergencies to US pediatric dentistry training programs. Pediatr Dent. 2006;28:431–437.
- Sheiham A. Dental caries affects body weight, growth and quality of life in preschool children. Br Dent J. 2006;201:625–626.
- Marshall J, Sheller B, Mancl L. Caries-risk assessment and caries status of children with autism. Pediatr Dent. 2010;32:69–75.
- Jaber M. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. 2011;19:212–217..




